-
PDF
- Split View
-
Views
-
Cite
Cite
C. Langley, D. S. Memel, J. R. Kirwan, J. Pollock, S. Hewlett, D. Gubbay, J. Powell, Using the Health Assessment Questionnaire and welfare benefits advice to help people disabled through arthritis to access financial support, Rheumatology, Volume 43, Issue 7, July 2004, Pages 863–868, https://doi.org/10.1093/rheumatology/keh184
Close - Share Icon Share
Abstract
Objectives. To test, in a variety of health settings, the ability of the Health Assessment Questionnaire (HAQ) disability index to predict the eligibility of patients with moderate or severe arthritis for disability living allowance or attendance allowance.
Methods. The study included patients from 20 general practices and four hospital out-patient departments across four areas in the southwest of England. Adults with an established diagnosis of rheumatoid arthritis, or osteoarthritis of the hip or knee, and who were not in receipt of Disability Living Allowance (DLA) or Attendance Allowance (AA) were sent an HAQ. Those who scored 1.5 or more were offered an appointment with a welfare advice worker at which they completed an application for DLA or AA. After 3 months they were contacted by the advice worker and asked about the outcome of their applications.
Results. Over half of those who completed an HAQ scored 1.5 or over (moderate to severe disability as measured by the HAQ) and were offered advice from experienced welfare benefits advisors. Of these, 87% applied for DLA or AA. Sixty-nine per cent of the applicants were successful. Those scoring 1.75 and over were more likely to be awarded benefit (73% success CLs 67, 79) than people scoring between 1.5 and 1.625 where 55% (CLs 41,69) of applicants were successful.
Conclusion. The HAQ was shown to be a good predictor of eligibility for AA or DLA. It can be used, in a variety of health settings, to indicate patients who, with help from an experienced advisor, are likely to gain increased financial help.
Arthritis is the most common physical reason for people, especially the elderly, becoming disabled and encountering difficulty in performing activities of daily living (ADL) [1]. Overcoming such problems involves extra costs, but disabled people often have low incomes [2, 3]. Disability benefits are available but are not claimed by approximately half of those who are eligible [4].
Disability Living Allowance (DLA, for people under 65) and Attendance Allowance (AA, for those aged 65 and over) are non-means-tested benefits of up to £95 a week awarded to people on the basis of their need for personal care and/or their difficulties with mobility (see Box 1). Doctors and nurses in primary care and hospital out-patient clinics are often unaware of their patients’ functional difficulties [5, 6] and are often unclear whether they would qualify under social security legislation. It is possible that community nurses who see patients in their own homes could play some role in identifying people eligible for AA [7]. However, a recent development has been to employ experienced welfare advisors within general practices and other health settings [8]. Advantages include easier access, a less stigmatizing situation and the availability of experienced advisors with both the necessary knowledge and time to spend on their clients [9–11].
*2002–2003 figures.
These are benefits for people who have physical and/or mental health problems and are awarded on the basis of their care and supervision needs regarding the activities of daily living and, for DLA, mobility needs.
Both benefits are tax free and neither are means tested, are not affected by savings, nor dependent on National Insurance contributions. The recipient can be in work or not, living alone or not, have a carer or not.
They can be spent in any way chosen by the recipient, e.g. on food, heating, transport, aids, furniture, paid help in the house/garden, phone bills, clothing, holidays etc.
In some cases being awarded DLA or AA can lead to other payments such as increased income support, housing benefit and council tax benefit. Other additions can include disabled parking (Blue Badge), Motability scheme, free road tax, free or reduced cost health care (prescriptions, eye care, dental treatment) and transport to and from hospital.
DLA can be claimed by people up to the age of 65. It is made up of two levels of mobility component and three levels of care and the amount can be between £14.90* weekly (low care or mobility only) and £95.55* weekly (high rate care and upper level mobility).
AA can be claimed by those aged over 65 and has two levels, £37.65* weekly and £56.25* weekly, depending on whether the person needs help at night as well as during the day.
Unless the person's needs change, DLA and AA are awarded for a number of years—often for life.
The Health Assessment Questionnaire (HAQ) is commonly used by rheumatologists to reliably assess functional disability in arthritis [12] and its use has been advocated in primary care [13]. It is a 20-item instrument covering activities of daily living which the respondent indicates they can do ‘without any difficulty’, ‘with some difficulty’, ‘with much difficulty’ or are ‘unable to do’. Answers are moderated by questions about the use of aids and devices and help needed from other people. Rasch analysis has indicated it is a reasonably linear scale [14]. The HAQ is easily self-completed within 4 to 5 min and takes a minute or less to score. It gives a score of between 0 and 3 in steps of 0.125, where 3 means complete dependency in eight areas of daily living. The HAQ is therefore much more accessible than the DLA and AA forms which often take up to 2 h to complete. However, it was designed to assess functional status rather than the care and mobility needs which are addressed in detail during assessment for provision of DLA and AA.
A previous pilot study found that 79% of patients with arthritis with a HAQ score of 2 or more who applied with the help of a welfare benefits advisor qualified for benefits [15]. The present study aimed to test whether this was true in a wider context and whether the HAQ could be used similarly for people with moderate disabilities as signified by a score of 1.5 to less than 2. The main outcome measures were (a) the number applying for DLA or AA, (b) success rates for different levels of the HAQ and (c) the amount of benefit awarded.
Methods
Participants
Patients were recruited from four hospital rheumatology departments and 20 general practices in and around four towns in the southwest of England (Bristol, Gloucester, Taunton and Barnstaple). Eligible patients were over 16 and had been diagnosed, for a least 1 yr, with either rheumatoid arthritis affecting any joints or osteoarthritis of the hip or knee (the joints most commonly associated with disability due to osteoarthritis). In addition general practice patients were selected only if they had a current repeat prescription for painkillers and/or non-steroidal anti-inflammatory drugs (NSAIDs) indicating that arthritis was a current active problem. Hospital patients were either identified at the time of attending a rheumatology out-patient clinic or from rheumatology case registers. General practices contacted all such patients on their practice lists or a random sample of 100 if there were more than 100 on the medical records database.
Sample size
Based on the responses in the pilot study [15], which had indicated that a greater proportion of hospital patients were already receiving benefits, the number of patients to contact was initially set as 100 for each of eight general practices and 200 for each of the four hospital rheumatology departments. It was estimated that about 300 applications for benefits would be made.
The aim was to provide estimates of the award success rates in at least three HAQ bands (1.5–1.74, 1.75–1.9, ≥2). With 10% absolute precision a sample size of 96 per band was required to obtain any estimate with specified 95% confidence limits, and 68 per band with specified 90% confidence limits [16].
Procedure
When contacted the patients received an explanatory information sheet and a reply slip on which they could indicate if they were interested in joining the study and whether they were already in receipt of DLA or AA. These were returned by post to the organizing research unit.
All those who expressed an interest in joining and who were not in receipt of benefits were posted an HAQ and a consent form. Those scoring 1.5 and above were then contacted by telephone and offered an appointment with an experienced welfare benefits advice worker. The call was also an opportunity for participants to ask any further questions and for the researchers to briefly reiterate the purpose of the study and confirm informed consent. The study was approved by the South & West MREC and by LRECs in all the areas where there was participation.
The contact details of those who accepted the interview were then passed to the welfare benefits advisors for that locality. All the advisors were experienced and trained to give disability benefits advice and worked in the local Citizens’ Advice Bureau (CAB) or professional advice agency. Advisors contacted clients to arrange a convenient time and place for an interview at which they received advice and completed the benefit forms. Arrangements had been made for these to take place at the participant's general practice or hospital but some clients preferred a home visit or to visit the advice centre. After allowing 3 months’ decision time, the advisors contacted their clients to ascertain the outcome. This was recorded along with other details on a standard recording form and returned to the research unit.
Analysis
Recruitment was unbalanced across the original three HAQ bands with half of the final sample being in the top band. It was therefore decided to group HAQ scores into four ordinally related bands based on a minimum number of 50 cases per band. The proportion of people applying successfully for different scores of the HAQ was calculated and tested for statistical significance using χ2 for heterogeneity and trend. The success rate was similarly calculated for DLA and AA, and for GP and hospital samples separately. Secondary analysis explored the relationship between age and a successful application.
Results
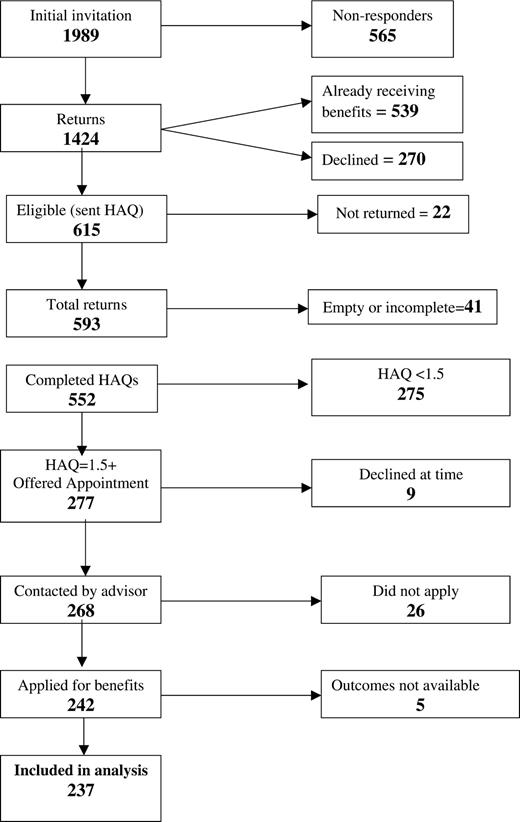
The total number who were sent an initial invitation through general practices and hospital outpatients was 1989. The number of participants at each stage is shown in Fig. 1. The details of recruitment by types of source and locality are included in Table 1.
Comparison of study sites across different localities
| Locality . | Study sites . | Number invited to participate . | Number eligible and sent HAQ . | Number offered appointment (HAQ ≥ 1.5) . | Number applied for benefit . | Number (%) successful . |
|---|---|---|---|---|---|---|
| North Bristol | General practices | 415 | 129 | 55 | 50 | 32 (64) |
| Hospital rheumatology | 154 | 49 | 23 | 19 | 13 (68) | |
| Gloucester | General practices | 204 | 69 | 20 | 20 | 11 (55) |
| Hospital rheumatology | 188 | 60 | 30 | 27 | 19 (70) | |
| Taunton | General practices | 169 | 69 | 27 | 23 | 18 (78) |
| Hospital rheumatology | 449 | 116 | 55 | 45 | 28 (62) | |
| North Devon | General practices | 273 | 90 | 41 | 29 | 23 (79) |
| Hospital rheumatology | 137 | 33 | 26 | 24 | 19 (79) | |
| Combined | General practices | 1061 | 357 | 143 | 122 | 84 (69) |
| Hospital rheumatology | 928 | 258 | 134 | 115 | 79 (69) | |
| Total | 1989 | 615 | 277 | 237 | 163 (69) |
| Locality . | Study sites . | Number invited to participate . | Number eligible and sent HAQ . | Number offered appointment (HAQ ≥ 1.5) . | Number applied for benefit . | Number (%) successful . |
|---|---|---|---|---|---|---|
| North Bristol | General practices | 415 | 129 | 55 | 50 | 32 (64) |
| Hospital rheumatology | 154 | 49 | 23 | 19 | 13 (68) | |
| Gloucester | General practices | 204 | 69 | 20 | 20 | 11 (55) |
| Hospital rheumatology | 188 | 60 | 30 | 27 | 19 (70) | |
| Taunton | General practices | 169 | 69 | 27 | 23 | 18 (78) |
| Hospital rheumatology | 449 | 116 | 55 | 45 | 28 (62) | |
| North Devon | General practices | 273 | 90 | 41 | 29 | 23 (79) |
| Hospital rheumatology | 137 | 33 | 26 | 24 | 19 (79) | |
| Combined | General practices | 1061 | 357 | 143 | 122 | 84 (69) |
| Hospital rheumatology | 928 | 258 | 134 | 115 | 79 (69) | |
| Total | 1989 | 615 | 277 | 237 | 163 (69) |
Comparison of study sites across different localities
| Locality . | Study sites . | Number invited to participate . | Number eligible and sent HAQ . | Number offered appointment (HAQ ≥ 1.5) . | Number applied for benefit . | Number (%) successful . |
|---|---|---|---|---|---|---|
| North Bristol | General practices | 415 | 129 | 55 | 50 | 32 (64) |
| Hospital rheumatology | 154 | 49 | 23 | 19 | 13 (68) | |
| Gloucester | General practices | 204 | 69 | 20 | 20 | 11 (55) |
| Hospital rheumatology | 188 | 60 | 30 | 27 | 19 (70) | |
| Taunton | General practices | 169 | 69 | 27 | 23 | 18 (78) |
| Hospital rheumatology | 449 | 116 | 55 | 45 | 28 (62) | |
| North Devon | General practices | 273 | 90 | 41 | 29 | 23 (79) |
| Hospital rheumatology | 137 | 33 | 26 | 24 | 19 (79) | |
| Combined | General practices | 1061 | 357 | 143 | 122 | 84 (69) |
| Hospital rheumatology | 928 | 258 | 134 | 115 | 79 (69) | |
| Total | 1989 | 615 | 277 | 237 | 163 (69) |
| Locality . | Study sites . | Number invited to participate . | Number eligible and sent HAQ . | Number offered appointment (HAQ ≥ 1.5) . | Number applied for benefit . | Number (%) successful . |
|---|---|---|---|---|---|---|
| North Bristol | General practices | 415 | 129 | 55 | 50 | 32 (64) |
| Hospital rheumatology | 154 | 49 | 23 | 19 | 13 (68) | |
| Gloucester | General practices | 204 | 69 | 20 | 20 | 11 (55) |
| Hospital rheumatology | 188 | 60 | 30 | 27 | 19 (70) | |
| Taunton | General practices | 169 | 69 | 27 | 23 | 18 (78) |
| Hospital rheumatology | 449 | 116 | 55 | 45 | 28 (62) | |
| North Devon | General practices | 273 | 90 | 41 | 29 | 23 (79) |
| Hospital rheumatology | 137 | 33 | 26 | 24 | 19 (79) | |
| Combined | General practices | 1061 | 357 | 143 | 122 | 84 (69) |
| Hospital rheumatology | 928 | 258 | 134 | 115 | 79 (69) | |
| Total | 1989 | 615 | 277 | 237 | 163 (69) |
Characteristics of responders
The response rate to the initial contact was 71.6%. Just over 70% of responders were female and the overall mean age was 66.5 yr. With respect to gender and age there were no statistically significant differences between responders and non-responders. Fifty-three per cent of the initial sample were contacted through general practice and 59% of responders came from that source.
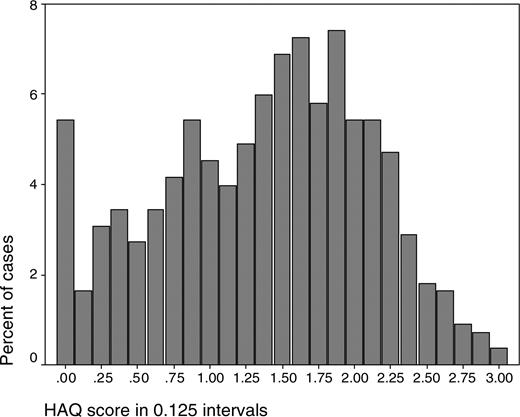
Thirty-eight per cent of responders were already in receipt of benefits. Six hundred and fifteen were eligible at this stage of the study and were sent an HAQ. If more than one question was omitted the HAQ was deemed incomplete. Three respondents had omitted one question so that their scores, being divided by 7, gave figures between the 0.125 steps. In the results these cases were included in the next higher 0.125 band. The distribution of scores of the 552 completed HAQs is shown in Fig. 2. Fifty per cent scored 1.5 or more and were offered appointments with advice workers.
Characteristics of completers
An approximately equal numbers of those who completed applications came from GP and hospital routes, but whereas 77% of the GP sample applied for AA because they were aged 65 or older, the applications of the hospital sample were divided equally between AA and DLA. Over 87% of those offered an interview applied for benefit. Completed data were obtained for 237 participants.
Outcomes
Successful application
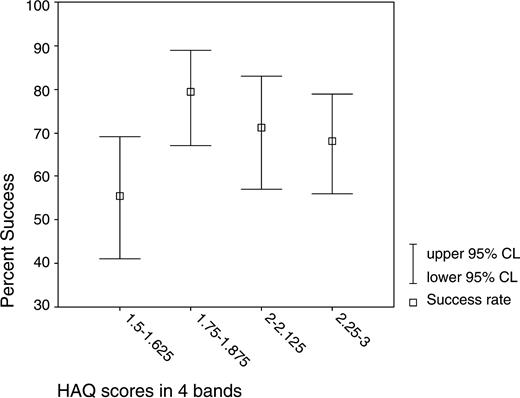
Table 2 and Fig. 3 show the success rates for the HAQ scores in four bands together with 95% confidence limits for the success rate.
Success rates for HAQ scores grouped into four bands
| . | . | Successful applications . | . | |
|---|---|---|---|---|
| HAQ score bands . | Numbers applying (result known) . | Number . | Proportion (%) (95% CI) . | |
| A (1.5–1.625) | 56 | 31 | 55.4 (41, 69) | |
| B (1.75–1.875) | 63 | 50 | 79.4 (67, 89) | |
| C (2–2.125) | 52 | 37 | 71.2 (57, 83) | |
| D (2.25–3) | 66 | 45 | 68.2 (56, 79) | |
| Total | 237 | 163 | 68.8 (63, 75) | |
| . | . | Successful applications . | . | |
|---|---|---|---|---|
| HAQ score bands . | Numbers applying (result known) . | Number . | Proportion (%) (95% CI) . | |
| A (1.5–1.625) | 56 | 31 | 55.4 (41, 69) | |
| B (1.75–1.875) | 63 | 50 | 79.4 (67, 89) | |
| C (2–2.125) | 52 | 37 | 71.2 (57, 83) | |
| D (2.25–3) | 66 | 45 | 68.2 (56, 79) | |
| Total | 237 | 163 | 68.8 (63, 75) | |
Success rates for HAQ scores grouped into four bands
| . | . | Successful applications . | . | |
|---|---|---|---|---|
| HAQ score bands . | Numbers applying (result known) . | Number . | Proportion (%) (95% CI) . | |
| A (1.5–1.625) | 56 | 31 | 55.4 (41, 69) | |
| B (1.75–1.875) | 63 | 50 | 79.4 (67, 89) | |
| C (2–2.125) | 52 | 37 | 71.2 (57, 83) | |
| D (2.25–3) | 66 | 45 | 68.2 (56, 79) | |
| Total | 237 | 163 | 68.8 (63, 75) | |
| . | . | Successful applications . | . | |
|---|---|---|---|---|
| HAQ score bands . | Numbers applying (result known) . | Number . | Proportion (%) (95% CI) . | |
| A (1.5–1.625) | 56 | 31 | 55.4 (41, 69) | |
| B (1.75–1.875) | 63 | 50 | 79.4 (67, 89) | |
| C (2–2.125) | 52 | 37 | 71.2 (57, 83) | |
| D (2.25–3) | 66 | 45 | 68.2 (56, 79) | |
| Total | 237 | 163 | 68.8 (63, 75) | |
Success rates and confidence limits for HAQ scores in four bands.
There was a significant overall variation across the bands in the proportion of applicants awarded benefits (χ2 3df = 8.13, P = 0.043) but this was not a linear trend (χ2 1df = 0.972, P = 0.325). The substantial rise in award rate between bands A and B is not sustained in bands C and D. For lower scores between 1.5 and 1.625 the success rate was reduced but still exceeded 50%. The figures do not include people who successfully asked for review or appealed against the decision. The outcome of application was not related to age or gender (data not shown).
Generalizability
Table 1 shows the details of participation and success rates for sites according to type or site (GP or hospital) and locality. As shown in Table 1 there was no difference, overall, between the successful application rates of general practice patients compared with those contacted through hospital out-patients. The distribution patterns of successes across the four HAQ bands differed slightly (data not shown), but not significantly, and was consistent with the higher proportion of AA applications from the general practice sample. The observed differences between geographical localities areas were not significant (overall χ2 = 3.69, 3df, P = 0.439).
Outcomes for different diagnoses
Subdividing the data into rheumatoid arthritis (RA) and osteoarthritis (OA) showed that the distribution of HAQ scores were very similar for both groups. There were no significant differences between patients with RA and those with OA regarding success levels for the four HAQ bands. Since the majority of RA patients were from the hospital samples and the majority of OA patients were derived from the GP samples, this matches the lack of difference mentioned above.
Differences in outcomes for DLA/AA
Almost twice as many people applied for AA as DLA (155 and 82 respectively) but the overall proportion of successful applications was very similar (AA 67.1% and DLA 72%). Whilst AA award rates were consistently and equally higher in HAQ bands greater than 1.625, DLA award rates indicated a peak in the 1.75–1.875 band that was not sustained in the higher bands. The overall shape of the relationship as illustrated in Fig. 3 therefore hides these differences in the award profiles. The asymptotic curve for AA (which is awarded to older applicants) may reflect the maximum award prediction impact of a HAQ score of 1.75. For the (younger) DLA applicants, however, the lower success rates in HAQ bands C and D compared with band B, if not a chance effect, might indicate different criteria being adopted in the formal assessments. A summary of results for the two benefits analysed separately is shown in Table 3.
Success rates for DLA and AA separately
| . | DLA . | . | AA . | . | ||
|---|---|---|---|---|---|---|
| HAQ band . | Number of applicants . | Proportion successful (%) (95% CL)* . | Number of applicants . | Proportion successful (%) (95% CL)* . | ||
| A (1.5–1.625) | 21 | 66.7 (43, 85) | 35 | 48.6 (31, 66) | ||
| B (1.75–1.875) | 24 | 87.5 (68, 97) | 39 | 74.4 (58, 87) | ||
| C (2–2.125) | 19 | 68.4 (43, 87) | 33 | 72.7 (54, 87) | ||
| D (2.25–3) | 18 | 61.1 (36, 83) | 48 | 70.8 (56, 83) | ||
| . | DLA . | . | AA . | . | ||
|---|---|---|---|---|---|---|
| HAQ band . | Number of applicants . | Proportion successful (%) (95% CL)* . | Number of applicants . | Proportion successful (%) (95% CL)* . | ||
| A (1.5–1.625) | 21 | 66.7 (43, 85) | 35 | 48.6 (31, 66) | ||
| B (1.75–1.875) | 24 | 87.5 (68, 97) | 39 | 74.4 (58, 87) | ||
| C (2–2.125) | 19 | 68.4 (43, 87) | 33 | 72.7 (54, 87) | ||
| D (2.25–3) | 18 | 61.1 (36, 83) | 48 | 70.8 (56, 83) | ||
*χ2 test for heterogeneity, 3df: DLA = 4.33 (P = 0.230); AA = 7.15 (P = 0.067). χ2 test for trend, 1df: DLA = 0.60 (P = 0.440); AA = 3.15 (P = 0.076).
Success rates for DLA and AA separately
| . | DLA . | . | AA . | . | ||
|---|---|---|---|---|---|---|
| HAQ band . | Number of applicants . | Proportion successful (%) (95% CL)* . | Number of applicants . | Proportion successful (%) (95% CL)* . | ||
| A (1.5–1.625) | 21 | 66.7 (43, 85) | 35 | 48.6 (31, 66) | ||
| B (1.75–1.875) | 24 | 87.5 (68, 97) | 39 | 74.4 (58, 87) | ||
| C (2–2.125) | 19 | 68.4 (43, 87) | 33 | 72.7 (54, 87) | ||
| D (2.25–3) | 18 | 61.1 (36, 83) | 48 | 70.8 (56, 83) | ||
| . | DLA . | . | AA . | . | ||
|---|---|---|---|---|---|---|
| HAQ band . | Number of applicants . | Proportion successful (%) (95% CL)* . | Number of applicants . | Proportion successful (%) (95% CL)* . | ||
| A (1.5–1.625) | 21 | 66.7 (43, 85) | 35 | 48.6 (31, 66) | ||
| B (1.75–1.875) | 24 | 87.5 (68, 97) | 39 | 74.4 (58, 87) | ||
| C (2–2.125) | 19 | 68.4 (43, 87) | 33 | 72.7 (54, 87) | ||
| D (2.25–3) | 18 | 61.1 (36, 83) | 48 | 70.8 (56, 83) | ||
*χ2 test for heterogeneity, 3df: DLA = 4.33 (P = 0.230); AA = 7.15 (P = 0.067). χ2 test for trend, 1df: DLA = 0.60 (P = 0.440); AA = 3.15 (P = 0.076).
Amount of benefit awarded
The DLA awarded to the whole study cohort amounted to £2309.25 per week and the AA awarded to £4492.20 per week. Together these give an annual total of more than £353 000 (2002–2003 rates). It is not known how many patients would have completed the benefits forms if they had not been in the study.
Discussion
Limitations of the study
This study is the first major study to examine the usefulness of a routinely used and standardized assessment tool in order to advise disabled people to seek advice on welfare benefits and to apply for disability benefit. As with many projects that seek to be innovative within the naturally occurring population, there were certain limitations that could not be foreseen and/or overcome.
The recruitment method used meant that a large number of people had to be contacted, including those who were not eligible to participate in the study because they were already receiving benefits or because their disability score was low (HAQ of 1.5 or less). The initial target was to invite 1600 people to participate (100 from each general practice and 200 from each hospital) in order to gain 300 who completed all stages of the project. However, early recruitment figures indicated that more patients than estimated were already receiving benefit and more had low HAQ scores than noted in previous studies [5,15] so additional general practices and more hospital out-patients were included in the study. Such wastage would not occur if appropriate patients were identified as part of routine clinical practice as severity is known and patients could be asked if they were already in receipt of benefits.
The 35 people who did not accept an interview or who decided not to apply for benefits were spread between all the HAQ bands. We did not request reasons for non-application but patients spontaneously commented that, for example, they did not feel they were sufficiently disabled to qualify for benefit or that they did not need extra money.
In order to ensure that all the applications were of a similar high standard the study included the use of professional advice workers available to patients in a healthcare setting but did not address the added value of this approach. Advisors are increasingly available in health settings [9] and this was an approach which was successful in the pilot study. Provision of welfare advisors has been shown to be a service much in demand [17] and there are some reports that doctors experience a reduced workload in general practices which include welfare benefits advisors [9]. Using a screening tool such as the HAQ would maximize the efficiency of such a service.
The analysis has not provided a clear cut-off point between encouraging and discouraging people concerning benefits applications. The study did not aim to demonstrate the negative value of lower scores. Approximately half of those who scored half-way on the HAQ scale were awarded benefit, but the paper records gave no obvious reason why these should have been selected. Inspection of the data showed that it was not attributable to any particular advisor and it is reasonable to assume that it happened as part of the Department of Work and Pensions (DWP) assessment procedure. It is important to recognize that some people with lower scores may succeed due to other morbidity factors, not included in the study, which are not well reflected in the HAQ which was devised to test for disability due to arthritis. The results show that a high score was likely to be met with successful application but 50% of those who scored 1.5 also made successful applications, thus leaving open the clear possibility that people with lower HAQ scores may still qualify for benefit.
Generalizability and implications
The sample was taken from both hospital and general practice populations and these have been shown to have different characteristics [15]. In addition participants came from urban and rural environments, from research and non-research general practices and from teaching and non-teaching hospitals. In all groups the results were similar and this suggests a wide generalizability of the findings.
A number of initiatives have suggested that healthcare professionals could play a legitimizing role in encouraging people to apply for DLA or AA and that welfare advice should be available in the same environment as people seek healthcare advice [11, 18]. This study has extended this from primary care to the hospital out-patient situation.
In some cases the health professional may be fully aware of functional difficulties [7], especially if the patient is often seen at home because she or he is housebound. More commonly, however, doctors and nurses are unsure about their patients’ levels of disability [5] and could use the HAQ to reduce this uncertainty. Moreover, given the ease of self-completion of the HAQ, this model has the potential for dissemination direct to the public without using health professionals. This could be done by the Department for Work and Pensions (DWP) or by charities such as Arthritis Care.
The figures of benefits awarded do not include extra ‘passported’ benefits such as increased income support and free or cheaper healthcare items (Box 1). Welfare benefits advisors, including those engaged in the study, give clients a complete benefit check so that although data on additional benefits were not systematically collected, we do know that there were additional amounts gained which do not appear in our results. DLA and AA, especially for older people, is often awarded for life. Thus the total increased income was considerable for many of the participants. Whilst it is beyond the scope of this study to suggest how the increased finances might improve health and quality of life, the levels of benefit awarded could, for example, prevent someone on a fixed pension falling into poverty. Although the overall amount awarded was substantial (over £350 000 per annum) there were some costs in providing this service. While these are clearly modest in relation to the income gained, a detailed analysis is under way and will be reported elsewhere.
Conclusion
Over 70% of applicants who scored 1.75 or more on the HAQ and applied for benefit with the help of a welfare benefits advisor were awarded DLA or AA. This means of helping people with arthritis to gain disability benefits was generalizable across different sites and localities, including general practices and hospitals, rural and urban areas. The HAQ is therefore recommended as a guide in encouraging people with arthritis to apply for DLA or AA. Until further research is undertaken to provide more precise estimates, a HAQ score of 1.75 can be taken as an indication that patients with arthritis who apply for DLA or AA have a very good chance of securing a substantial increase in income for life.
We thank Christine Dadd for her invaluable work on the project on which our paper is based, Caroline Coleman for her contribution to the design of the study and her facilitation with Citizens’ Advice personnel, Robin Means for his advice concerning the design, Maggie Hehir for input into the design and her role, together with SH, as independent assessor of raw data and Kate Francis for her valuable administrative work.
We thank the staff and doctors at the following general practices and rheumatology out-patients: Bristol—Southmead Health Centre (both practices), Bradgate Surgery, Horfield Health Centre, Lawrence Hill Health Centre, Cossham Hospital; Gloucester—Abbotswood Surgery, Churchdown Surgery, Gloucester Royal Hospital, Standish Hospital; Barnstaple—Queen's Medical Centre, Brannam Medical Centre, Waterside Primary Care, (Ilfracombe), North Devon District Hospital; Taunton—Warwick House Medical Centre, St. James Medical Centre, Taunton and Somerset Hospital.
We thank managers and staff at the following advice agencies: North Bristol Advice Centre, Barton Hill Advice Service, Gloucester CAB, Barnstaple CAB, Taunton CAB.
A Nuffield Foundation Research Grant was received.
The authors have declared no conflicts of interest.
References
Department for Work and Pensions. Disability care and mobility benefits—February 2002 quarterly statistical enquiry.
Kestenbaum A. Disability costs and charges for community care London: The Disablement Income Group,
Craig P, Greenslade M.
Memel D, Kirwan J. General practitioners’ knowledge of functional and social factors in patients with rheumatoid arthritis.
Rubenstein LV, McCoy JM, Cope DW et al. Improving patient quality of life with feedback to physicians about functional status.
Hoskins R. Welfare benefits’ screening and referral: a new direction for community nurses?
National Audit Office. Tackling pensioner poverty: Encouraging take-up of entitlements. London: The Stationery Office,
Kemp M. Serious benefits: the success of CAB benefit take-up campaigns. London: Citizens Advice,
Abbott S, Hobby L. Welfare benefits advice: improving access and improving health.
Galvin K, Sharples A, Jackson D. Citizens Advice Bureaux in general practice: an illuminative evaluation.
Kirwan J, Reeback J. Stanford health assessment questionnaire modified to assess disability in British patients with rheumatoid arthritis.
Tennant A, Hillman M, Fear J, Pickering A, Chamberlain MA. Are we making the most of the Stanford Health Assessment Questionnaire?
Memel D, Kirwan J, Langley C, Hewlett S, Hehir M. Prediction of successful application for disability benefits for people with arthritis using the Health Assessment Questionnaire.
Lwanga SK, Lemeshow S.
Hopton J, Dlugolecka M. Patients perceptions of need for primary health care services: useful priority setting?
Author notes
Air Balloon Surgery, Bristol, 1University of Bristol Academic Rheumatology, Bristol, 2Faculty of Health and Social Care, University of the West of England, Bristol, 3Barton Hill Advice Service, Easton, Bristol, UK.



Comments