-
PDF
- Split View
-
Views
-
Cite
Cite
W Cheungpasitporn, C Thongprayoon, W Kittanamongkolchai, A Sakhuja, M A Mao, S B Erickson, Impact of admission serum potassium on mortality in patients with chronic kidney disease and cardiovascular disease, QJM: An International Journal of Medicine, Volume 110, Issue 11, November 2017, Pages 713–719, https://doi.org/10.1093/qjmed/hcx118
Close - Share Icon Share
Abstract
Little is known about the effect of admission potassium (K) on risk of in-hospital mortality in chronic kidney disease (CKD) and cardiovascular disease (CVD) patients.
The aim of this study was to assess the relationship between admission serum K and in-hospital mortality in all hospitalized patients stratified by CKD and/or CVD status.
All adult hospitalized patients who had admission serum K between years 2011 and 2013 were enrolled. Admission serum K was categorized into seven groups (<3.0, 3.0–3.5, 3.5–4.0, 4.0–4.5, 4.5–5.0, 5.0–5.5 and ≥5.5 mEq/L). The odds ratio (OR) of in-hospital mortality by admission serum K, using K 4.0–4.5 mEq/L as the reference group, was obtained by logistic regression analysis.
73,983 patients were studied. The lowest incidence of in-hospital mortality was associated with serum K within 4.0–4.5 mEq/L. A U-shaped curve emerged demonstrating higher in-hospital mortality associated with both serum K < 4.0 and >4.5 mEq/L. After adjusting for potential confounders, both serum K < 4.0 mEq/L and >5.0 mEq/L were associated with increased in-hospital mortality with ORs of 3.26 (95% CI 2.03–4.98), 2.40 (95% CI 1.89–3.04), 1.38 (95%CI 1.15–1.66), 1.89 (95% CI 1.49–2.38) and 3.62 (95%CI 2.73–4.76) when serum K were within <3.0, 3.0–3.5, 3.5–4.0, 5.0–5.5, and ≥5.5 mEq/L, respectively. In CVD patients, the highest in-hospital mortality was associated with serum K < 3.0 mEq/L (OR 1.70, 95%CI 1.31–2.18). In CKD patients, the highest in-hospital mortality was associated with serum K ≥ 5.5 mEq/L (OR 3.26, 95%CI 2.14–4.90).
Admission serum K < 4.0 mEq/L and >5.0 mEq/L were associated with increased in-hospital mortality. The mortality risk among patients with various admission potassium levels was affected by CKD and/or CVD status.
Introduction
Potassium (K) is the most abundant intracellular cation in the body.1 Its steep trans-cellular gradient is vital in maintaining cell membrane potential, performance of multiple cellular functions and metabolic balance.1–4 Serum K abnormalities with hyperkalemia and hypokalemia are common clinical problems4–6 with a prevalence as high as 48% of hospitalized patients.4,7–11 Depending on the severity of potassium derangement and patients’ cardiac status and comorbidities, clinical manifestations may range from an asymptomatic electrolyte disorder to cardiac arrhythmias and arrest.1,4
Studies have demonstrated impact of various K levels on patient outcomes including mortality.2,3,12–27 In the general patient population, both hyperkalemia and hypokalemia are significantly associated with higher in-hospital mortality.3,12–14 Among patients with cardiovascular disease (CVD), abnormal admission serum potassium levels are associated with an increased risk of ventricular arrhythmias.19 Although admission hyperkalemia and hypokalemia are both predictors for poor outcomes,20–22 the highest in-hospital mortality and a higher rate of cardiac arrhythmias have been observed in hypokalemic as compared to hyperkalemic patients.20,23 In patients with chronic kidney disease (CKD), both hyperkalemia and hypokalemia are also associated with higher mortality, with highest risk observed with hyperkalemia.2
Little is known about the effect of admission potassium on risk of in-hospital mortality in CKD and CVD patients. The objective of this study was to assess the relationship between serum K levels and in-hospital mortality in all hospitalized patients, and determine the associated risk stratified by CKD and/or CVD status.
Materials and methods
All adult (age 18 year or older) patients admitted to Mayo Clinic Rochester—a tertiary referral hospital—from 1 January 2011 through 31 December 2013 were included. Exclusion criteria consisted of patients without serum K measurement within 24 h of admission and patients with end stage renal disease (ESRD). For patients with multiple admissions during this period, only the first hospital admission was analyzed. ESRD was identified based on ICD-9 (International Classification of Diseases, Ninth Revision) code assignment (Supplementary Table S1) or an estimated glomerular filtration rate (eGFR) <15 ml/min/1.73 m2. The study was approved by the Institutional Review Board.
Clinical characteristics, demographic information, and laboratory data were collected from the institutional electronic medical record system. The admission serum K level, defined as the first serum K level within 24 h of hospital admission was collected. eGFR was derived using the Chronic Kidney Disease Epidemiology Collaboration equation.28 CKD was defined as a calculated creatinine eGFR less than 60 ml/min/1.73 m2. The Charlson Comorbidity score29 was computed for co-morbidities at the time of admission. Principal diagnoses were grouped based on ICD-9 codes at admission (Supplementary Table S2).
The primary outcome was in-hospital mortality. Subgroup analysis was also performed by stratification for the presence of CKD and/or CVD.30 The secondary outcome was hospital length of stay.
Statistical analysis
Continuous variables are reported as mean ± SD for normally distributed data and median (IQR) for non-normally distributed data. All categorical variables are reported as count with percentage. We categorized admission serum K levels based on its distribution into seven strata (<3.0, 3.0–3.5, 3.5–4.0, 4.0–4.5, 4.5–5.0, 5.0–5.5 and ≥5.5 mEq/l). The most common K level reference range (4.0–4.5 mEq/l) was selected as the reference group for outcome comparison (Table 1). Baseline demographics and clinical characteristics were compared among admission potassium strata using ANOVA for continuous variables and the Chi-square test for categorical variables. We performed univariate analysis and then multivariate logistic regression analysis to evaluate for independent associations between admission K levels and in-hospital mortality. Odds ratio (OR) with 95% CI are reported. OR was adjusted for variables with statistical significance (P values < 0.05) found between groups in univariate analysis. The adjusted variables included age, sex, race, eGFR, principal diagnosis, Charlson comorbidity score, comorbidities and medications. Comorbidities were coronary artery disease (CAD), congestive heart failure (CHF), peripheral vascular disease (PVD), stroke, diabetes mellitus (DM), chronic obstructive pulmonary disease (COPD) and cirrhosis. Medications were angiotensin-converting enzyme inhibitors (ACEI), angiotensin receptor blockers (ARB), diuretics and potassium supplements. We also performed linear regression analysis to ascertain the association between admission serum K levels and hospital length of stay. Due to the skewed distribution of data, length of stay was log transformed before entering into the model. A two-tailed P values of < 0.05 was considered statistically significant. All analyses were performed using JMP statistical software (version 10, SAS Institute, Cary, NC).
Baseline clinical characteristics
| Variables . | All . | Serum potassium level at hospital admission (mEq/l) . | |||||||
|---|---|---|---|---|---|---|---|---|---|
| <3.0 . | 3.0–<3.5 . | 3.5–<4.0 . | 4.0–<4.5 . | 4.5–<5.0 . | 5.0–<5.5 . | ≥5.5 . | P . | ||
| N | 73 983 | 700 | 3943 | 17315 | 29815 | 16381 | 4463 | 1366 | |
| Age (year) | 61 ± 18 | 59 ± 18 | 60 ± 19 | 58 ± 19 | 61 ± 18 | 63 ± 17 | 66 ± 16 | 67 ± 16 | <0.001 |
| Male | 38973 (53) | 273 (39) | 1556 (39) | 7999 (46) | 16131 (54) | 9522 (58) | 2670 (60) | 822 (60) | <0.001 |
| Caucasian | 68809 (93) | 642 (92) | 3562 (90) | 15819 (91) | 27791 (93) | 15497 (95) | 4220 (95) | 1278 (94) | <0.001 |
| GFR (ml/min/1.73m2) | 80 ± 26 | 82 ± 34 | 84 ± 28 | 86 ± 26 | 82 ± 25 | 76 ± 25 | 67 ± 27 | 54 ± 27 | <0.001 |
| Principal Diagnosis | <0.001 | ||||||||
| Cardiovascular | 15716 (21) | 128 (18) | 844 (21) | 3747 (22) | 6291 (21) | 3380 (21) | 1019 (23) | 307 (22) | |
| Endocrine/Metabolic | 1879 (3) | 75 (11) | 137 (3) | 384 (2) | 558 (2) | 459 (3) | 158 (4) | 108 (8) | |
| Gastrointestinal | 6920 (9) | 80 (11) | 537 (14) | 1824 (11) | 2594 (9) | 1335 (8) | 429 (10) | 121 (9) | |
| Hematology/Oncology | 11558 (16) | 59 (8) | 347 (9) | 2000 (12) | 4756 (16) | 3209 (20) | 953 (21) | 234 (17) | |
| Infectious Disease | 2171 (3) | 51 (7) | 269 (7) | 600 (3) | 705 (2) | 374 (2) | 111 (2) | 61 (4) | |
| Respiratory | 2968 (4) | 25 (4) | 213 (5) | 638 (4) | 1098 (4) | 673 (4) | 222 (5) | 99 (7) | |
| Injury/poisoning | 11434 (15) | 140 (20) | 699 (18) | 3070 (18) | 4573 (15) | 2248 (14) | 528 (11) | 176 (13) | |
| Other | 21337 (29) | 142 (20) | 897 (23) | 5052 (29) | 9240 (31) | 4703 (29) | 1043 (23) | 260 (19) | |
| Charlson Score | 1.7 ± 2.3 | 1.8 ± 2.5 | 1.7 ± 2.3 | 1.5 ± 2.2 | 1.6 ± 2.2 | 1.9 ± 2.4 | 2.3 ± 2.6 | 2.8 ± 2.7 | <0.001 |
| Comorbidities | |||||||||
| CAD | 5260 (7) | 38 (5) | 227 (6) | 1009 (6) | 2042 (7) | 1347 (8) | 423 (9) | 174 (13) | <0.001 |
| CHF | 4679 (6) | 60 (9) | 275 (7) | 965 (6) | 1665 (6) | 1112 (7) | 421 (9) | 181 (13) | <0.001 |
| PVD | 2065 (3) | 20 (3) | 106 (3) | 371 (2) | 736 (2) | 552 (3) | 199 (4) | 81 (6) | <0.001 |
| Stroke | 5228 (7) | 52 (7) | 315 (8) | 1118 (6) | 1944 (7) | 1247 (8) | 398 (9) | 154 (11) | <0.001 |
| DM | 13752 (19) | 114 (16) | 669 (17) | 2743 (16) | 5096 (17) | 3414 (21) | 1206 (27) | 510 (37) | <0.001 |
| COPD | 6131 (8) | 56 (8) | 326 (8) | 1197 (7) | 2227 (7) | 1518 (9) | 586 (13) | 221 (16) | <0.001 |
| Cirrhosis | 1713 (3) | 24 (3) | 114 (3) | 408 (2) | 581 (2) | 369 (2) | 150 (3) | 67 (5) | <0.001 |
| Medications | |||||||||
| ACEI/ARB | 20068 (27) | 162 (23) | 974 (25) | 4067 (23) | 7930 (27) | 4745 (29) | 1627 (36) | 563 (41) | <0.001 |
| Diuretics | 22020 (30) | 341 (49) | 1659 (42) | 5452 (31) | 7974 (27) | 4508 (28) | 1490 (33) | 596 (44) | <0.001 |
| Potassium supplement | 8317 (11) | 401 (57) | 1025 (26) | 2246 (13) | 2731 (9) | 1336 (8) | 431 (10) | 147 (11) | <0.001 |
| Variables . | All . | Serum potassium level at hospital admission (mEq/l) . | |||||||
|---|---|---|---|---|---|---|---|---|---|
| <3.0 . | 3.0–<3.5 . | 3.5–<4.0 . | 4.0–<4.5 . | 4.5–<5.0 . | 5.0–<5.5 . | ≥5.5 . | P . | ||
| N | 73 983 | 700 | 3943 | 17315 | 29815 | 16381 | 4463 | 1366 | |
| Age (year) | 61 ± 18 | 59 ± 18 | 60 ± 19 | 58 ± 19 | 61 ± 18 | 63 ± 17 | 66 ± 16 | 67 ± 16 | <0.001 |
| Male | 38973 (53) | 273 (39) | 1556 (39) | 7999 (46) | 16131 (54) | 9522 (58) | 2670 (60) | 822 (60) | <0.001 |
| Caucasian | 68809 (93) | 642 (92) | 3562 (90) | 15819 (91) | 27791 (93) | 15497 (95) | 4220 (95) | 1278 (94) | <0.001 |
| GFR (ml/min/1.73m2) | 80 ± 26 | 82 ± 34 | 84 ± 28 | 86 ± 26 | 82 ± 25 | 76 ± 25 | 67 ± 27 | 54 ± 27 | <0.001 |
| Principal Diagnosis | <0.001 | ||||||||
| Cardiovascular | 15716 (21) | 128 (18) | 844 (21) | 3747 (22) | 6291 (21) | 3380 (21) | 1019 (23) | 307 (22) | |
| Endocrine/Metabolic | 1879 (3) | 75 (11) | 137 (3) | 384 (2) | 558 (2) | 459 (3) | 158 (4) | 108 (8) | |
| Gastrointestinal | 6920 (9) | 80 (11) | 537 (14) | 1824 (11) | 2594 (9) | 1335 (8) | 429 (10) | 121 (9) | |
| Hematology/Oncology | 11558 (16) | 59 (8) | 347 (9) | 2000 (12) | 4756 (16) | 3209 (20) | 953 (21) | 234 (17) | |
| Infectious Disease | 2171 (3) | 51 (7) | 269 (7) | 600 (3) | 705 (2) | 374 (2) | 111 (2) | 61 (4) | |
| Respiratory | 2968 (4) | 25 (4) | 213 (5) | 638 (4) | 1098 (4) | 673 (4) | 222 (5) | 99 (7) | |
| Injury/poisoning | 11434 (15) | 140 (20) | 699 (18) | 3070 (18) | 4573 (15) | 2248 (14) | 528 (11) | 176 (13) | |
| Other | 21337 (29) | 142 (20) | 897 (23) | 5052 (29) | 9240 (31) | 4703 (29) | 1043 (23) | 260 (19) | |
| Charlson Score | 1.7 ± 2.3 | 1.8 ± 2.5 | 1.7 ± 2.3 | 1.5 ± 2.2 | 1.6 ± 2.2 | 1.9 ± 2.4 | 2.3 ± 2.6 | 2.8 ± 2.7 | <0.001 |
| Comorbidities | |||||||||
| CAD | 5260 (7) | 38 (5) | 227 (6) | 1009 (6) | 2042 (7) | 1347 (8) | 423 (9) | 174 (13) | <0.001 |
| CHF | 4679 (6) | 60 (9) | 275 (7) | 965 (6) | 1665 (6) | 1112 (7) | 421 (9) | 181 (13) | <0.001 |
| PVD | 2065 (3) | 20 (3) | 106 (3) | 371 (2) | 736 (2) | 552 (3) | 199 (4) | 81 (6) | <0.001 |
| Stroke | 5228 (7) | 52 (7) | 315 (8) | 1118 (6) | 1944 (7) | 1247 (8) | 398 (9) | 154 (11) | <0.001 |
| DM | 13752 (19) | 114 (16) | 669 (17) | 2743 (16) | 5096 (17) | 3414 (21) | 1206 (27) | 510 (37) | <0.001 |
| COPD | 6131 (8) | 56 (8) | 326 (8) | 1197 (7) | 2227 (7) | 1518 (9) | 586 (13) | 221 (16) | <0.001 |
| Cirrhosis | 1713 (3) | 24 (3) | 114 (3) | 408 (2) | 581 (2) | 369 (2) | 150 (3) | 67 (5) | <0.001 |
| Medications | |||||||||
| ACEI/ARB | 20068 (27) | 162 (23) | 974 (25) | 4067 (23) | 7930 (27) | 4745 (29) | 1627 (36) | 563 (41) | <0.001 |
| Diuretics | 22020 (30) | 341 (49) | 1659 (42) | 5452 (31) | 7974 (27) | 4508 (28) | 1490 (33) | 596 (44) | <0.001 |
| Potassium supplement | 8317 (11) | 401 (57) | 1025 (26) | 2246 (13) | 2731 (9) | 1336 (8) | 431 (10) | 147 (11) | <0.001 |
Continuous data are presented as mean ± SD; categorical data are presented as count (%).
Baseline clinical characteristics
| Variables . | All . | Serum potassium level at hospital admission (mEq/l) . | |||||||
|---|---|---|---|---|---|---|---|---|---|
| <3.0 . | 3.0–<3.5 . | 3.5–<4.0 . | 4.0–<4.5 . | 4.5–<5.0 . | 5.0–<5.5 . | ≥5.5 . | P . | ||
| N | 73 983 | 700 | 3943 | 17315 | 29815 | 16381 | 4463 | 1366 | |
| Age (year) | 61 ± 18 | 59 ± 18 | 60 ± 19 | 58 ± 19 | 61 ± 18 | 63 ± 17 | 66 ± 16 | 67 ± 16 | <0.001 |
| Male | 38973 (53) | 273 (39) | 1556 (39) | 7999 (46) | 16131 (54) | 9522 (58) | 2670 (60) | 822 (60) | <0.001 |
| Caucasian | 68809 (93) | 642 (92) | 3562 (90) | 15819 (91) | 27791 (93) | 15497 (95) | 4220 (95) | 1278 (94) | <0.001 |
| GFR (ml/min/1.73m2) | 80 ± 26 | 82 ± 34 | 84 ± 28 | 86 ± 26 | 82 ± 25 | 76 ± 25 | 67 ± 27 | 54 ± 27 | <0.001 |
| Principal Diagnosis | <0.001 | ||||||||
| Cardiovascular | 15716 (21) | 128 (18) | 844 (21) | 3747 (22) | 6291 (21) | 3380 (21) | 1019 (23) | 307 (22) | |
| Endocrine/Metabolic | 1879 (3) | 75 (11) | 137 (3) | 384 (2) | 558 (2) | 459 (3) | 158 (4) | 108 (8) | |
| Gastrointestinal | 6920 (9) | 80 (11) | 537 (14) | 1824 (11) | 2594 (9) | 1335 (8) | 429 (10) | 121 (9) | |
| Hematology/Oncology | 11558 (16) | 59 (8) | 347 (9) | 2000 (12) | 4756 (16) | 3209 (20) | 953 (21) | 234 (17) | |
| Infectious Disease | 2171 (3) | 51 (7) | 269 (7) | 600 (3) | 705 (2) | 374 (2) | 111 (2) | 61 (4) | |
| Respiratory | 2968 (4) | 25 (4) | 213 (5) | 638 (4) | 1098 (4) | 673 (4) | 222 (5) | 99 (7) | |
| Injury/poisoning | 11434 (15) | 140 (20) | 699 (18) | 3070 (18) | 4573 (15) | 2248 (14) | 528 (11) | 176 (13) | |
| Other | 21337 (29) | 142 (20) | 897 (23) | 5052 (29) | 9240 (31) | 4703 (29) | 1043 (23) | 260 (19) | |
| Charlson Score | 1.7 ± 2.3 | 1.8 ± 2.5 | 1.7 ± 2.3 | 1.5 ± 2.2 | 1.6 ± 2.2 | 1.9 ± 2.4 | 2.3 ± 2.6 | 2.8 ± 2.7 | <0.001 |
| Comorbidities | |||||||||
| CAD | 5260 (7) | 38 (5) | 227 (6) | 1009 (6) | 2042 (7) | 1347 (8) | 423 (9) | 174 (13) | <0.001 |
| CHF | 4679 (6) | 60 (9) | 275 (7) | 965 (6) | 1665 (6) | 1112 (7) | 421 (9) | 181 (13) | <0.001 |
| PVD | 2065 (3) | 20 (3) | 106 (3) | 371 (2) | 736 (2) | 552 (3) | 199 (4) | 81 (6) | <0.001 |
| Stroke | 5228 (7) | 52 (7) | 315 (8) | 1118 (6) | 1944 (7) | 1247 (8) | 398 (9) | 154 (11) | <0.001 |
| DM | 13752 (19) | 114 (16) | 669 (17) | 2743 (16) | 5096 (17) | 3414 (21) | 1206 (27) | 510 (37) | <0.001 |
| COPD | 6131 (8) | 56 (8) | 326 (8) | 1197 (7) | 2227 (7) | 1518 (9) | 586 (13) | 221 (16) | <0.001 |
| Cirrhosis | 1713 (3) | 24 (3) | 114 (3) | 408 (2) | 581 (2) | 369 (2) | 150 (3) | 67 (5) | <0.001 |
| Medications | |||||||||
| ACEI/ARB | 20068 (27) | 162 (23) | 974 (25) | 4067 (23) | 7930 (27) | 4745 (29) | 1627 (36) | 563 (41) | <0.001 |
| Diuretics | 22020 (30) | 341 (49) | 1659 (42) | 5452 (31) | 7974 (27) | 4508 (28) | 1490 (33) | 596 (44) | <0.001 |
| Potassium supplement | 8317 (11) | 401 (57) | 1025 (26) | 2246 (13) | 2731 (9) | 1336 (8) | 431 (10) | 147 (11) | <0.001 |
| Variables . | All . | Serum potassium level at hospital admission (mEq/l) . | |||||||
|---|---|---|---|---|---|---|---|---|---|
| <3.0 . | 3.0–<3.5 . | 3.5–<4.0 . | 4.0–<4.5 . | 4.5–<5.0 . | 5.0–<5.5 . | ≥5.5 . | P . | ||
| N | 73 983 | 700 | 3943 | 17315 | 29815 | 16381 | 4463 | 1366 | |
| Age (year) | 61 ± 18 | 59 ± 18 | 60 ± 19 | 58 ± 19 | 61 ± 18 | 63 ± 17 | 66 ± 16 | 67 ± 16 | <0.001 |
| Male | 38973 (53) | 273 (39) | 1556 (39) | 7999 (46) | 16131 (54) | 9522 (58) | 2670 (60) | 822 (60) | <0.001 |
| Caucasian | 68809 (93) | 642 (92) | 3562 (90) | 15819 (91) | 27791 (93) | 15497 (95) | 4220 (95) | 1278 (94) | <0.001 |
| GFR (ml/min/1.73m2) | 80 ± 26 | 82 ± 34 | 84 ± 28 | 86 ± 26 | 82 ± 25 | 76 ± 25 | 67 ± 27 | 54 ± 27 | <0.001 |
| Principal Diagnosis | <0.001 | ||||||||
| Cardiovascular | 15716 (21) | 128 (18) | 844 (21) | 3747 (22) | 6291 (21) | 3380 (21) | 1019 (23) | 307 (22) | |
| Endocrine/Metabolic | 1879 (3) | 75 (11) | 137 (3) | 384 (2) | 558 (2) | 459 (3) | 158 (4) | 108 (8) | |
| Gastrointestinal | 6920 (9) | 80 (11) | 537 (14) | 1824 (11) | 2594 (9) | 1335 (8) | 429 (10) | 121 (9) | |
| Hematology/Oncology | 11558 (16) | 59 (8) | 347 (9) | 2000 (12) | 4756 (16) | 3209 (20) | 953 (21) | 234 (17) | |
| Infectious Disease | 2171 (3) | 51 (7) | 269 (7) | 600 (3) | 705 (2) | 374 (2) | 111 (2) | 61 (4) | |
| Respiratory | 2968 (4) | 25 (4) | 213 (5) | 638 (4) | 1098 (4) | 673 (4) | 222 (5) | 99 (7) | |
| Injury/poisoning | 11434 (15) | 140 (20) | 699 (18) | 3070 (18) | 4573 (15) | 2248 (14) | 528 (11) | 176 (13) | |
| Other | 21337 (29) | 142 (20) | 897 (23) | 5052 (29) | 9240 (31) | 4703 (29) | 1043 (23) | 260 (19) | |
| Charlson Score | 1.7 ± 2.3 | 1.8 ± 2.5 | 1.7 ± 2.3 | 1.5 ± 2.2 | 1.6 ± 2.2 | 1.9 ± 2.4 | 2.3 ± 2.6 | 2.8 ± 2.7 | <0.001 |
| Comorbidities | |||||||||
| CAD | 5260 (7) | 38 (5) | 227 (6) | 1009 (6) | 2042 (7) | 1347 (8) | 423 (9) | 174 (13) | <0.001 |
| CHF | 4679 (6) | 60 (9) | 275 (7) | 965 (6) | 1665 (6) | 1112 (7) | 421 (9) | 181 (13) | <0.001 |
| PVD | 2065 (3) | 20 (3) | 106 (3) | 371 (2) | 736 (2) | 552 (3) | 199 (4) | 81 (6) | <0.001 |
| Stroke | 5228 (7) | 52 (7) | 315 (8) | 1118 (6) | 1944 (7) | 1247 (8) | 398 (9) | 154 (11) | <0.001 |
| DM | 13752 (19) | 114 (16) | 669 (17) | 2743 (16) | 5096 (17) | 3414 (21) | 1206 (27) | 510 (37) | <0.001 |
| COPD | 6131 (8) | 56 (8) | 326 (8) | 1197 (7) | 2227 (7) | 1518 (9) | 586 (13) | 221 (16) | <0.001 |
| Cirrhosis | 1713 (3) | 24 (3) | 114 (3) | 408 (2) | 581 (2) | 369 (2) | 150 (3) | 67 (5) | <0.001 |
| Medications | |||||||||
| ACEI/ARB | 20068 (27) | 162 (23) | 974 (25) | 4067 (23) | 7930 (27) | 4745 (29) | 1627 (36) | 563 (41) | <0.001 |
| Diuretics | 22020 (30) | 341 (49) | 1659 (42) | 5452 (31) | 7974 (27) | 4508 (28) | 1490 (33) | 596 (44) | <0.001 |
| Potassium supplement | 8317 (11) | 401 (57) | 1025 (26) | 2246 (13) | 2731 (9) | 1336 (8) | 431 (10) | 147 (11) | <0.001 |
Continuous data are presented as mean ± SD; categorical data are presented as count (%).
Results
Baseline characteristics
A total of 147 358 hospital admissions were identified. After excluding 31 144 patients who lacked admission serum K measurement, 2,702 patients with ESRD and 39 529 readmissions, 73 983 unique patients were enrolled (Supplementary Figure S1). Of the 73 983 patients, 68 809 (93%) patients were Caucasian and 38 973 (53%) were male (Table 1). Mean age was 61 ± 18 years. Patient comorbidities included CAD (7%), CHF (6%), PVD (3%), stroke (7%), DM (19%), COPD (8%) and cirrhosis (3%). The admission serum K levels were normally distributed (Supplementary Figure S2).
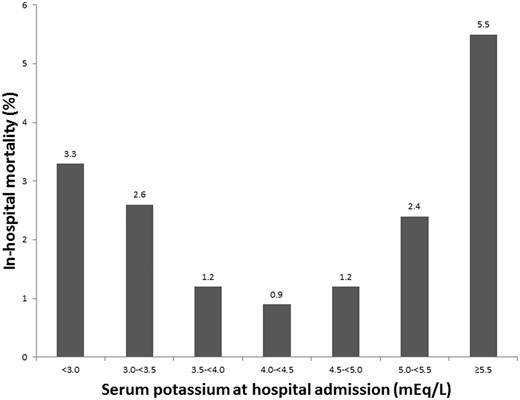
Admission serum K levels and in-hospital mortality
Among 73 983 patients, 973 (1.3%) died in the hospital. The lowest in-hospital mortality was observed in patients with admission serum K of 4.0–4.5 mEq/l. A U-shaped distribution demonstrated higher in-hospital mortality associated with both serum K < 4.0 and >4.5 mEq/l (Figure 1). When adjusted for age, sex, race, eGFR, principal diagnosis, comorbid conditions and medication, both serum K < 4.0 and >5.0 mEq/l were associated with increased risk of in-hospital mortality with ORs of 3.26 (95% CI 2.03–4.98), 2.40 (95% CI 1.89–3.04), 1.38 (95% CI 1.15–1.66), 1.89 (95% CI 1.49–2.38) and 3.62 (95% CI 2.73–4.76) when serum K were within <3.0, 3.0–3.5, 3.5–4.0, 5.0–5.5 and ≥5.5 mEq/l, respectively (Table 2[a]).
Clinical outcomes
| Outcome . | Serum potassium level at hospital admission (mEq/l) . | ||||||
|---|---|---|---|---|---|---|---|
| <3.0 . | 3.0–<3.5 . | 3.5–<4.0 . | 4.0–<4.5 . | 4.5–<5.0 . | 5.0–<5.5 . | ≥5.5 . | |
| (a) In hospital mortality | |||||||
| Hospital mortality | 23 (3.3) | 101 (2.6) | 209 (1.2) | 268 (0.9) | 191 (1.2) | 106 (2.4) | 75 (5.5) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 3.75 (2.37–5.64) | 2.90 (2.29–3.64) | 1.35 (1.12–1.61) | 1 (ref) | 1.30 (1.08–1.57) | 2.68 (2.13–3.35) | 6.40 (4.90–8.28) |
| Model 2#: | 3.26 (2.03–4.98) | 2.40 (1.89–3.04) | 1.38 (1.15–1.66) | 1 (ref) | 1.13 (0.94–1.37) | 1.89 (1.49–2.38) | 3.62 (2.73–4.76) |
| (b) Hospital Length of Stay (LOS) | |||||||
| Hospital LOS | 5 (3–9) | 5 (3–8) | 4 (3–7) | 4 (3–7) | 4 (3–7) | 5 (3–7) | 5 (3–9) |
| LOS, relative prolongation (95% CI) | |||||||
| Model 1: unadjusted | 1.24 (1.18–1.31) | 1.16 (1.14–1.19) | 1.04 (1.03–1.06) | 1 (ref) | 1.03 (1.02–1.04) | 1.10 (1.08–1.13) | 1.23 (1.18–1.28) |
| Model 2#: | 1.22 (1.16–1.29) | 1.14 (1.12–1.17) | 1.04 (1.03–1.06) | 1 (ref) | 1.01 (1.001–1.03) | 1.06 (1.04–1.08) | 1.15 (1.11–1.20) |
| Outcome . | Serum potassium level at hospital admission (mEq/l) . | ||||||
|---|---|---|---|---|---|---|---|
| <3.0 . | 3.0–<3.5 . | 3.5–<4.0 . | 4.0–<4.5 . | 4.5–<5.0 . | 5.0–<5.5 . | ≥5.5 . | |
| (a) In hospital mortality | |||||||
| Hospital mortality | 23 (3.3) | 101 (2.6) | 209 (1.2) | 268 (0.9) | 191 (1.2) | 106 (2.4) | 75 (5.5) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 3.75 (2.37–5.64) | 2.90 (2.29–3.64) | 1.35 (1.12–1.61) | 1 (ref) | 1.30 (1.08–1.57) | 2.68 (2.13–3.35) | 6.40 (4.90–8.28) |
| Model 2#: | 3.26 (2.03–4.98) | 2.40 (1.89–3.04) | 1.38 (1.15–1.66) | 1 (ref) | 1.13 (0.94–1.37) | 1.89 (1.49–2.38) | 3.62 (2.73–4.76) |
| (b) Hospital Length of Stay (LOS) | |||||||
| Hospital LOS | 5 (3–9) | 5 (3–8) | 4 (3–7) | 4 (3–7) | 4 (3–7) | 5 (3–7) | 5 (3–9) |
| LOS, relative prolongation (95% CI) | |||||||
| Model 1: unadjusted | 1.24 (1.18–1.31) | 1.16 (1.14–1.19) | 1.04 (1.03–1.06) | 1 (ref) | 1.03 (1.02–1.04) | 1.10 (1.08–1.13) | 1.23 (1.18–1.28) |
| Model 2#: | 1.22 (1.16–1.29) | 1.14 (1.12–1.17) | 1.04 (1.03–1.06) | 1 (ref) | 1.01 (1.001–1.03) | 1.06 (1.04–1.08) | 1.15 (1.11–1.20) |
model 2: Adjusted for age, sex, race, GFR, principal diagnosis, Charlson comorbidity score, CAD, CHF, PVD, stroke, DM, COPD, cirrhosis, use of ACEI/ARB, diuretics and potassium supplements.
Clinical outcomes
| Outcome . | Serum potassium level at hospital admission (mEq/l) . | ||||||
|---|---|---|---|---|---|---|---|
| <3.0 . | 3.0–<3.5 . | 3.5–<4.0 . | 4.0–<4.5 . | 4.5–<5.0 . | 5.0–<5.5 . | ≥5.5 . | |
| (a) In hospital mortality | |||||||
| Hospital mortality | 23 (3.3) | 101 (2.6) | 209 (1.2) | 268 (0.9) | 191 (1.2) | 106 (2.4) | 75 (5.5) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 3.75 (2.37–5.64) | 2.90 (2.29–3.64) | 1.35 (1.12–1.61) | 1 (ref) | 1.30 (1.08–1.57) | 2.68 (2.13–3.35) | 6.40 (4.90–8.28) |
| Model 2#: | 3.26 (2.03–4.98) | 2.40 (1.89–3.04) | 1.38 (1.15–1.66) | 1 (ref) | 1.13 (0.94–1.37) | 1.89 (1.49–2.38) | 3.62 (2.73–4.76) |
| (b) Hospital Length of Stay (LOS) | |||||||
| Hospital LOS | 5 (3–9) | 5 (3–8) | 4 (3–7) | 4 (3–7) | 4 (3–7) | 5 (3–7) | 5 (3–9) |
| LOS, relative prolongation (95% CI) | |||||||
| Model 1: unadjusted | 1.24 (1.18–1.31) | 1.16 (1.14–1.19) | 1.04 (1.03–1.06) | 1 (ref) | 1.03 (1.02–1.04) | 1.10 (1.08–1.13) | 1.23 (1.18–1.28) |
| Model 2#: | 1.22 (1.16–1.29) | 1.14 (1.12–1.17) | 1.04 (1.03–1.06) | 1 (ref) | 1.01 (1.001–1.03) | 1.06 (1.04–1.08) | 1.15 (1.11–1.20) |
| Outcome . | Serum potassium level at hospital admission (mEq/l) . | ||||||
|---|---|---|---|---|---|---|---|
| <3.0 . | 3.0–<3.5 . | 3.5–<4.0 . | 4.0–<4.5 . | 4.5–<5.0 . | 5.0–<5.5 . | ≥5.5 . | |
| (a) In hospital mortality | |||||||
| Hospital mortality | 23 (3.3) | 101 (2.6) | 209 (1.2) | 268 (0.9) | 191 (1.2) | 106 (2.4) | 75 (5.5) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 3.75 (2.37–5.64) | 2.90 (2.29–3.64) | 1.35 (1.12–1.61) | 1 (ref) | 1.30 (1.08–1.57) | 2.68 (2.13–3.35) | 6.40 (4.90–8.28) |
| Model 2#: | 3.26 (2.03–4.98) | 2.40 (1.89–3.04) | 1.38 (1.15–1.66) | 1 (ref) | 1.13 (0.94–1.37) | 1.89 (1.49–2.38) | 3.62 (2.73–4.76) |
| (b) Hospital Length of Stay (LOS) | |||||||
| Hospital LOS | 5 (3–9) | 5 (3–8) | 4 (3–7) | 4 (3–7) | 4 (3–7) | 5 (3–7) | 5 (3–9) |
| LOS, relative prolongation (95% CI) | |||||||
| Model 1: unadjusted | 1.24 (1.18–1.31) | 1.16 (1.14–1.19) | 1.04 (1.03–1.06) | 1 (ref) | 1.03 (1.02–1.04) | 1.10 (1.08–1.13) | 1.23 (1.18–1.28) |
| Model 2#: | 1.22 (1.16–1.29) | 1.14 (1.12–1.17) | 1.04 (1.03–1.06) | 1 (ref) | 1.01 (1.001–1.03) | 1.06 (1.04–1.08) | 1.15 (1.11–1.20) |
model 2: Adjusted for age, sex, race, GFR, principal diagnosis, Charlson comorbidity score, CAD, CHF, PVD, stroke, DM, COPD, cirrhosis, use of ACEI/ARB, diuretics and potassium supplements.
Admission serum K levels and hospital length of stay
The median hospital length of stay was 4 (IQR 3-7) days. When adjusted for potential confounders, both serum K < 4.0 and >4.5 mEq/l were associated with prolonged hospital length of stay (Table 2[b]) with the highest relative length of stay prolongation of 1.22 (95% CI 1.16-1.29) when admission serum K levels were <3.0, followed by relative prolongation of 1.15 (95% CI 1.11–1.20) with K ≥ 5.5 mEq/l.
Admission serum K levels in patients with CVD
Of 73 983 patients, 15 716 with CVD were studied. The lowest in-hospital mortality (1.4%) was also observed in CVD patients with admission serum K levels of 4.0–4.5 mEq/l (Table 3[a]). When adjusted for potential confounders, both serum K < 4.0 and >5.0 mEq/l were associated with an increased risk of in-hospital mortality. Hypokalemia in CVD patients with admission serum K < 3.0 mEq/l was associated with the highest in-hospital mortality with OR of 5.48 (95% CI 2.60–10.45), exceeding the risk of in-hospital mortality in those with admission serum K ≥ 5.5 mEq/l (OR 2.42, 95% CI 1.36–4.08) (Table 3[a]).
In-hospital mortality in patient subgroup
| (a) Patients admitted with principal diagnosis of CVD (n = 15 716) . | |||||||
|---|---|---|---|---|---|---|---|
| Outcome . | Serum potassium level at hospital admission (mEq/l) . | ||||||
| <3.0 . | 3.0–<3.5 . | 3.5–<4.0 . | 4.0–<4.5 . | 4.5–<5.0 . | 5.0–<5.5 . | ≥5.5 . | |
| N | 128 | 844 | 3747 | 6291 | 3380 | 1019 | 307 |
| Hospital mortality | 10 (7.8) | 34 (4.0) | 76 (2.0) | 90 (1.4) | 56 (1.7) | 34 (3.3) | 17 (5.5) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 5.84 (2.79–10.99) | 2.89 (1.91–4.28) | 1.43 (1.05–1.94) | 1 (ref) | 1.16 (0.83–1.62) | 2.38 (1.57–3.51) | 4.04 (2.30–6.70) |
| Model 2#: | 5.48 (2.60–10.45) | 2.79 (1.84–4.14) | 1.48 (1.09–2.02) | 1 (ref) | 1.02 (0.73–1.43) | 1.74 (1.14–2.60) | 2.42 (1.36–4.08) |
(b) Patients with GFR of ≤ 60 ml/min/1.73 m2 (n = 16 710) | |||||||
| Outcome | Serum potassium level at hospital admission (mEq/l) | ||||||
| <3.0 | 3.0–<3.5 | 3.5–<4.0 | 4.0–<4.5 | 4.5–<5.0 | 5.0–<5.5 | ≥5.5 | |
| N | 194 | 872 | 2885 | 5589 | 4415 | 1886 | 869 |
| Hospital mortality | 9 (4.6) | 41 (4.7) | 83 (2.9) | 117 (2.1) | 94 (2.1) | 67 (3.6) | 58 (6.7) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 2.28 (1.06–4.31) | 2.31 (1.59–3.29) | 1.39 (1.04–1.84) | 1 (ref) | 1.02 (0.77–1.34) | 1.72 (1.26–2.33) | 3.34 (2.41–4.60) |
| Model 2#: | 2.19 (1.01–4.22) | 2.04 (1.39–2.93) | 1.38 (1.03–1.83) | 1 (ref) | 1.01 (0.77–1.34) | 1.62 (1.18–2.21) | 2.95 (2.09–4.11) |
| (a) Patients admitted with principal diagnosis of CVD (n = 15 716) . | |||||||
|---|---|---|---|---|---|---|---|
| Outcome . | Serum potassium level at hospital admission (mEq/l) . | ||||||
| <3.0 . | 3.0–<3.5 . | 3.5–<4.0 . | 4.0–<4.5 . | 4.5–<5.0 . | 5.0–<5.5 . | ≥5.5 . | |
| N | 128 | 844 | 3747 | 6291 | 3380 | 1019 | 307 |
| Hospital mortality | 10 (7.8) | 34 (4.0) | 76 (2.0) | 90 (1.4) | 56 (1.7) | 34 (3.3) | 17 (5.5) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 5.84 (2.79–10.99) | 2.89 (1.91–4.28) | 1.43 (1.05–1.94) | 1 (ref) | 1.16 (0.83–1.62) | 2.38 (1.57–3.51) | 4.04 (2.30–6.70) |
| Model 2#: | 5.48 (2.60–10.45) | 2.79 (1.84–4.14) | 1.48 (1.09–2.02) | 1 (ref) | 1.02 (0.73–1.43) | 1.74 (1.14–2.60) | 2.42 (1.36–4.08) |
(b) Patients with GFR of ≤ 60 ml/min/1.73 m2 (n = 16 710) | |||||||
| Outcome | Serum potassium level at hospital admission (mEq/l) | ||||||
| <3.0 | 3.0–<3.5 | 3.5–<4.0 | 4.0–<4.5 | 4.5–<5.0 | 5.0–<5.5 | ≥5.5 | |
| N | 194 | 872 | 2885 | 5589 | 4415 | 1886 | 869 |
| Hospital mortality | 9 (4.6) | 41 (4.7) | 83 (2.9) | 117 (2.1) | 94 (2.1) | 67 (3.6) | 58 (6.7) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 2.28 (1.06–4.31) | 2.31 (1.59–3.29) | 1.39 (1.04–1.84) | 1 (ref) | 1.02 (0.77–1.34) | 1.72 (1.26–2.33) | 3.34 (2.41–4.60) |
| Model 2#: | 2.19 (1.01–4.22) | 2.04 (1.39–2.93) | 1.38 (1.03–1.83) | 1 (ref) | 1.01 (0.77–1.34) | 1.62 (1.18–2.21) | 2.95 (2.09–4.11) |
model 2: Adjusted for age, sex, race, GFR, Principal diagnosis, Charlson comorbidity score, CAD, CHF, PVD, stroke, DM, COPD, cirrhosis, use of ACEI/ARB, diuretics and potassium supplements.
In-hospital mortality in patient subgroup
| (a) Patients admitted with principal diagnosis of CVD (n = 15 716) . | |||||||
|---|---|---|---|---|---|---|---|
| Outcome . | Serum potassium level at hospital admission (mEq/l) . | ||||||
| <3.0 . | 3.0–<3.5 . | 3.5–<4.0 . | 4.0–<4.5 . | 4.5–<5.0 . | 5.0–<5.5 . | ≥5.5 . | |
| N | 128 | 844 | 3747 | 6291 | 3380 | 1019 | 307 |
| Hospital mortality | 10 (7.8) | 34 (4.0) | 76 (2.0) | 90 (1.4) | 56 (1.7) | 34 (3.3) | 17 (5.5) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 5.84 (2.79–10.99) | 2.89 (1.91–4.28) | 1.43 (1.05–1.94) | 1 (ref) | 1.16 (0.83–1.62) | 2.38 (1.57–3.51) | 4.04 (2.30–6.70) |
| Model 2#: | 5.48 (2.60–10.45) | 2.79 (1.84–4.14) | 1.48 (1.09–2.02) | 1 (ref) | 1.02 (0.73–1.43) | 1.74 (1.14–2.60) | 2.42 (1.36–4.08) |
(b) Patients with GFR of ≤ 60 ml/min/1.73 m2 (n = 16 710) | |||||||
| Outcome | Serum potassium level at hospital admission (mEq/l) | ||||||
| <3.0 | 3.0–<3.5 | 3.5–<4.0 | 4.0–<4.5 | 4.5–<5.0 | 5.0–<5.5 | ≥5.5 | |
| N | 194 | 872 | 2885 | 5589 | 4415 | 1886 | 869 |
| Hospital mortality | 9 (4.6) | 41 (4.7) | 83 (2.9) | 117 (2.1) | 94 (2.1) | 67 (3.6) | 58 (6.7) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 2.28 (1.06–4.31) | 2.31 (1.59–3.29) | 1.39 (1.04–1.84) | 1 (ref) | 1.02 (0.77–1.34) | 1.72 (1.26–2.33) | 3.34 (2.41–4.60) |
| Model 2#: | 2.19 (1.01–4.22) | 2.04 (1.39–2.93) | 1.38 (1.03–1.83) | 1 (ref) | 1.01 (0.77–1.34) | 1.62 (1.18–2.21) | 2.95 (2.09–4.11) |
| (a) Patients admitted with principal diagnosis of CVD (n = 15 716) . | |||||||
|---|---|---|---|---|---|---|---|
| Outcome . | Serum potassium level at hospital admission (mEq/l) . | ||||||
| <3.0 . | 3.0–<3.5 . | 3.5–<4.0 . | 4.0–<4.5 . | 4.5–<5.0 . | 5.0–<5.5 . | ≥5.5 . | |
| N | 128 | 844 | 3747 | 6291 | 3380 | 1019 | 307 |
| Hospital mortality | 10 (7.8) | 34 (4.0) | 76 (2.0) | 90 (1.4) | 56 (1.7) | 34 (3.3) | 17 (5.5) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 5.84 (2.79–10.99) | 2.89 (1.91–4.28) | 1.43 (1.05–1.94) | 1 (ref) | 1.16 (0.83–1.62) | 2.38 (1.57–3.51) | 4.04 (2.30–6.70) |
| Model 2#: | 5.48 (2.60–10.45) | 2.79 (1.84–4.14) | 1.48 (1.09–2.02) | 1 (ref) | 1.02 (0.73–1.43) | 1.74 (1.14–2.60) | 2.42 (1.36–4.08) |
(b) Patients with GFR of ≤ 60 ml/min/1.73 m2 (n = 16 710) | |||||||
| Outcome | Serum potassium level at hospital admission (mEq/l) | ||||||
| <3.0 | 3.0–<3.5 | 3.5–<4.0 | 4.0–<4.5 | 4.5–<5.0 | 5.0–<5.5 | ≥5.5 | |
| N | 194 | 872 | 2885 | 5589 | 4415 | 1886 | 869 |
| Hospital mortality | 9 (4.6) | 41 (4.7) | 83 (2.9) | 117 (2.1) | 94 (2.1) | 67 (3.6) | 58 (6.7) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 2.28 (1.06–4.31) | 2.31 (1.59–3.29) | 1.39 (1.04–1.84) | 1 (ref) | 1.02 (0.77–1.34) | 1.72 (1.26–2.33) | 3.34 (2.41–4.60) |
| Model 2#: | 2.19 (1.01–4.22) | 2.04 (1.39–2.93) | 1.38 (1.03–1.83) | 1 (ref) | 1.01 (0.77–1.34) | 1.62 (1.18–2.21) | 2.95 (2.09–4.11) |
model 2: Adjusted for age, sex, race, GFR, Principal diagnosis, Charlson comorbidity score, CAD, CHF, PVD, stroke, DM, COPD, cirrhosis, use of ACEI/ARB, diuretics and potassium supplements.
Admission serum K levels in patients with CKD
Of 73 983 patients, 16 710 patients with CKD were studied. The lowest incidence of in-hospital mortality (2.1%) was when admission serum K levels were within 4.0–5.0 mEq/l (Table 3[b]). A U-shaped curve emerged in CKD patients demonstrating higher in-hospital mortality associated with both admission serum K levels <4.0 and >5.0 mEq/l, with the highest mortality of 6.7% with K ≥ 5.5 mEq/l followed by K < 3 mEq/l of 4.6%. When adjusted for potential confounders, both serum K levels < 4.0 and >5.0 mEq/l were associated with an increased risk of in-hospital mortality. Hyperkalemia with admission serum K ≥ 5.5 mEq/l was associated with the highest in-hospital mortality in CKD patients with OR of 2.95 (95% CI 2.09–4.11), exceeding the risk of in-hospital mortality in those with admission serum K <3.0 mEq/l (OR 2.19, 95% CI 1.01–4.22) (Table 3[b]).
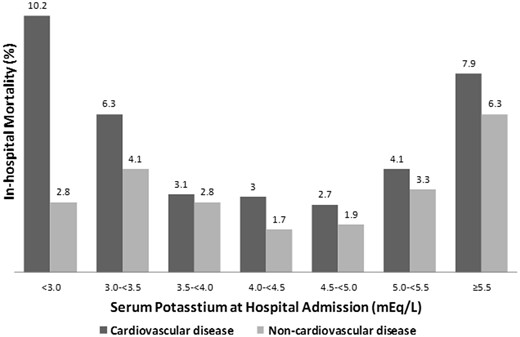
Admission serum K levels among CKD patients with and without CVD
Of 16 710 patients with CKD, 4,971 were admitted for the diagnosis of CVD. The lowest incidence of in-hospital mortality was observed when admission serum K levels were within 4.0–5.0 mEq/l both in CKD patients with and without CVD (Figure 2). The highest in-hospital mortality in CKD patients with CVD was associated with a serum K < 3.0 mEq/l (OR 4.06, 95% CI 1.35–9.95), while the highest in-hospital mortality in CKD patients without CVD was associated with serum K ≥ 5.5 mEq/l (OR 3.26, 95% CI 2.14–4.90) (Table 4[a and b)].
In-hospital mortality among CKD Patients with and without CVD
| (a) Patients with GFR of < 60 ml/min/1.73 m2 and admitted for CVD (n = 4971) . | |||||||
|---|---|---|---|---|---|---|---|
| Outcome . | Serum potassium level at hospital admission (mEq/l) . | ||||||
| <3.0 . | 3.0–<3.5 . | 3.5–<4.0 . | 4.0–<4.5 . | 4.5–<5.0 . | 5.0–<5.5 . | ≥5.5 . | |
| N | 49 | 239 | 950 | 1693 | 1285 | 539 | 216 |
| Hospital mortality | 5 (10.2) | 15 (6.3) | 29 (3.1) | 50 (3.0) | 34 (2.7) | 22 (4.1) | 17 (7.9) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 3.73 (1.25–9.02) | 2.20 (1.18–3.89) | 1.03 (0.64–1.63) | 1 (ref) | 0.89 (0.57–1.38) | 1.40 (0.82–2.30) | 2.81 (1.55–4.87) |
| Model 2#: | 4.06 (1.35–9.95) | 2.34 (1.25–4.17) | 1.07 (0.66–1.69) | 1 (ref) | 0.88 (0.56–1.36) | 1.22 (0.71–2.02) | 2.22 (1.21–3.92) |
(b) Patients with GFR of < 60 ml/min/1.73 m2 and admitted for non-CVD (n = 11 739) | |||||||
| Outcome | Serum potassium level at hospital admission (mEq/l) | ||||||
| <3.0 | 3.0–<3.5 | 3.5–<4.0 | 4.0–<4.5 | 4.5–<5.0 | 5.0–<5.5 | ≥5.5 | |
| N | 145 | 633 | 1935 | 3896 | 3130 | 1347 | 653 |
| Hospital mortality | 4 (2.8) | 26 (4.1) | 54 (2.8) | 67 (1.7) | 60 (1.9) | 45 (3.3) | 41 (6.3) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 1.62 (0.49–3.99) | 2.45 (1.52–3.83) | 1.64 (1.14–2.35) | 1 (ref) | 1.12 (0.78–1.59) | 1.98 (1.34–2.89) | 3.83 (2.55–5.67) |
| Model 2#: | 1.61 (0.48–4.01) | 2.41 (1.49–3.79) | 1.66 (1.15–2.39) | 1 (ref) | 1.09 (0.76–1.55) | 1.77 (1.19–2.60) | 3.26 (2.14–4.90) |
| (a) Patients with GFR of < 60 ml/min/1.73 m2 and admitted for CVD (n = 4971) . | |||||||
|---|---|---|---|---|---|---|---|
| Outcome . | Serum potassium level at hospital admission (mEq/l) . | ||||||
| <3.0 . | 3.0–<3.5 . | 3.5–<4.0 . | 4.0–<4.5 . | 4.5–<5.0 . | 5.0–<5.5 . | ≥5.5 . | |
| N | 49 | 239 | 950 | 1693 | 1285 | 539 | 216 |
| Hospital mortality | 5 (10.2) | 15 (6.3) | 29 (3.1) | 50 (3.0) | 34 (2.7) | 22 (4.1) | 17 (7.9) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 3.73 (1.25–9.02) | 2.20 (1.18–3.89) | 1.03 (0.64–1.63) | 1 (ref) | 0.89 (0.57–1.38) | 1.40 (0.82–2.30) | 2.81 (1.55–4.87) |
| Model 2#: | 4.06 (1.35–9.95) | 2.34 (1.25–4.17) | 1.07 (0.66–1.69) | 1 (ref) | 0.88 (0.56–1.36) | 1.22 (0.71–2.02) | 2.22 (1.21–3.92) |
(b) Patients with GFR of < 60 ml/min/1.73 m2 and admitted for non-CVD (n = 11 739) | |||||||
| Outcome | Serum potassium level at hospital admission (mEq/l) | ||||||
| <3.0 | 3.0–<3.5 | 3.5–<4.0 | 4.0–<4.5 | 4.5–<5.0 | 5.0–<5.5 | ≥5.5 | |
| N | 145 | 633 | 1935 | 3896 | 3130 | 1347 | 653 |
| Hospital mortality | 4 (2.8) | 26 (4.1) | 54 (2.8) | 67 (1.7) | 60 (1.9) | 45 (3.3) | 41 (6.3) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 1.62 (0.49–3.99) | 2.45 (1.52–3.83) | 1.64 (1.14–2.35) | 1 (ref) | 1.12 (0.78–1.59) | 1.98 (1.34–2.89) | 3.83 (2.55–5.67) |
| Model 2#: | 1.61 (0.48–4.01) | 2.41 (1.49–3.79) | 1.66 (1.15–2.39) | 1 (ref) | 1.09 (0.76–1.55) | 1.77 (1.19–2.60) | 3.26 (2.14–4.90) |
model 2: Adjusted for age, sex, race, GFR, Charlson comorbidity score, CAD, CHF, PVD, stroke, DM, COPD, cirrhosis, use of ACEI/ARB, diuretics and potassium supplements.
In-hospital mortality among CKD Patients with and without CVD
| (a) Patients with GFR of < 60 ml/min/1.73 m2 and admitted for CVD (n = 4971) . | |||||||
|---|---|---|---|---|---|---|---|
| Outcome . | Serum potassium level at hospital admission (mEq/l) . | ||||||
| <3.0 . | 3.0–<3.5 . | 3.5–<4.0 . | 4.0–<4.5 . | 4.5–<5.0 . | 5.0–<5.5 . | ≥5.5 . | |
| N | 49 | 239 | 950 | 1693 | 1285 | 539 | 216 |
| Hospital mortality | 5 (10.2) | 15 (6.3) | 29 (3.1) | 50 (3.0) | 34 (2.7) | 22 (4.1) | 17 (7.9) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 3.73 (1.25–9.02) | 2.20 (1.18–3.89) | 1.03 (0.64–1.63) | 1 (ref) | 0.89 (0.57–1.38) | 1.40 (0.82–2.30) | 2.81 (1.55–4.87) |
| Model 2#: | 4.06 (1.35–9.95) | 2.34 (1.25–4.17) | 1.07 (0.66–1.69) | 1 (ref) | 0.88 (0.56–1.36) | 1.22 (0.71–2.02) | 2.22 (1.21–3.92) |
(b) Patients with GFR of < 60 ml/min/1.73 m2 and admitted for non-CVD (n = 11 739) | |||||||
| Outcome | Serum potassium level at hospital admission (mEq/l) | ||||||
| <3.0 | 3.0–<3.5 | 3.5–<4.0 | 4.0–<4.5 | 4.5–<5.0 | 5.0–<5.5 | ≥5.5 | |
| N | 145 | 633 | 1935 | 3896 | 3130 | 1347 | 653 |
| Hospital mortality | 4 (2.8) | 26 (4.1) | 54 (2.8) | 67 (1.7) | 60 (1.9) | 45 (3.3) | 41 (6.3) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 1.62 (0.49–3.99) | 2.45 (1.52–3.83) | 1.64 (1.14–2.35) | 1 (ref) | 1.12 (0.78–1.59) | 1.98 (1.34–2.89) | 3.83 (2.55–5.67) |
| Model 2#: | 1.61 (0.48–4.01) | 2.41 (1.49–3.79) | 1.66 (1.15–2.39) | 1 (ref) | 1.09 (0.76–1.55) | 1.77 (1.19–2.60) | 3.26 (2.14–4.90) |
| (a) Patients with GFR of < 60 ml/min/1.73 m2 and admitted for CVD (n = 4971) . | |||||||
|---|---|---|---|---|---|---|---|
| Outcome . | Serum potassium level at hospital admission (mEq/l) . | ||||||
| <3.0 . | 3.0–<3.5 . | 3.5–<4.0 . | 4.0–<4.5 . | 4.5–<5.0 . | 5.0–<5.5 . | ≥5.5 . | |
| N | 49 | 239 | 950 | 1693 | 1285 | 539 | 216 |
| Hospital mortality | 5 (10.2) | 15 (6.3) | 29 (3.1) | 50 (3.0) | 34 (2.7) | 22 (4.1) | 17 (7.9) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 3.73 (1.25–9.02) | 2.20 (1.18–3.89) | 1.03 (0.64–1.63) | 1 (ref) | 0.89 (0.57–1.38) | 1.40 (0.82–2.30) | 2.81 (1.55–4.87) |
| Model 2#: | 4.06 (1.35–9.95) | 2.34 (1.25–4.17) | 1.07 (0.66–1.69) | 1 (ref) | 0.88 (0.56–1.36) | 1.22 (0.71–2.02) | 2.22 (1.21–3.92) |
(b) Patients with GFR of < 60 ml/min/1.73 m2 and admitted for non-CVD (n = 11 739) | |||||||
| Outcome | Serum potassium level at hospital admission (mEq/l) | ||||||
| <3.0 | 3.0–<3.5 | 3.5–<4.0 | 4.0–<4.5 | 4.5–<5.0 | 5.0–<5.5 | ≥5.5 | |
| N | 145 | 633 | 1935 | 3896 | 3130 | 1347 | 653 |
| Hospital mortality | 4 (2.8) | 26 (4.1) | 54 (2.8) | 67 (1.7) | 60 (1.9) | 45 (3.3) | 41 (6.3) |
| Mortality, OR (95% CI) | |||||||
| Model 1: unadjusted | 1.62 (0.49–3.99) | 2.45 (1.52–3.83) | 1.64 (1.14–2.35) | 1 (ref) | 1.12 (0.78–1.59) | 1.98 (1.34–2.89) | 3.83 (2.55–5.67) |
| Model 2#: | 1.61 (0.48–4.01) | 2.41 (1.49–3.79) | 1.66 (1.15–2.39) | 1 (ref) | 1.09 (0.76–1.55) | 1.77 (1.19–2.60) | 3.26 (2.14–4.90) |
model 2: Adjusted for age, sex, race, GFR, Charlson comorbidity score, CAD, CHF, PVD, stroke, DM, COPD, cirrhosis, use of ACEI/ARB, diuretics and potassium supplements.
Admission serum K levels and in-hospital mortality among CKD patients with and without CVD.
Discussion
In this cohort of 73 983 hospitalized patients, we demonstrate that admission K level is correlated with patient outcomes including in-hospital mortality and hospital length of stay. The admission serum K is associated with a U-shaped in-hospital mortality curve, with the nadir between K 4.0–4.5 mEq/l. Among patients with CVD, hypokalemia with a serum K < 3.0 mEq/l is associated with the highest (1.7-fold increased risk) in-hospital mortality. In-hospital mortality among CKD patients was found to be affected by the presence of concomitant CVD. In CKD patients with CVD, hypokalemia with a serum K < 3.0 mEq/l s associated with the highest (4.06-fold increased risk) in-hospital mortality, while hyperkalemia with serum K ≥ 5.5 mEq/l is associated with the highest (3.26-fold increased risk) in-hospital mortality in CKD patients without CVD.
Hypokalemia is commonly observed in patients with CVD due to loop diuretic use and low effective circulating volume (particularly with CHF) induced activation of the renin-angiotensin system (RAS).20,31 Our study showed that an admission serum K < 3.0 mEq/l was associated with the highest in-hospital mortality among CVD patients. Previously, higher in-hospital mortality has also been observed in hypokalemic patients with myocardial infarction, atrial fibrillation, and those undergoing cardiac surgery.20,24–26 Increased in-hospital mortality is likely explained by hypokalemia induced arrhythmias. Hypokalemia can increase frequency of ventricular ectopic beats, arrhythmias and sudden death in CVD patients.20,27 Goyal et al.20 demonstrated that rates of ventricular arrhythmias or cardiac arrest were significantly increased in patients with admission serum K < 3.0 mEq/l.
Hyperkalemia is a frequent metabolic complication of CKD with a prevalence as high as 31.5% in outpatient CKD patients.32 Reduced GFR and impaired sodium delivery to the distal nephron both limit renal K excretion in patients with CKD.33 In addition, comorbid conditions and medications used to manage CKD including RAS blockers also place CKD patients at higher risk for hyperkalemia.1,34–38 Hyperkalemia can result in slower electrical conduction,3,39 subsequently leading to arrhythmias and sudden cardiac death.40 Very recently, Lou et al. assessed the association between serum K and outcomes in CKD patients.2 The investigators demonstrated significant association of hyperkalemia and hypokalemia with worse outcomes including death, major adverse cardiovascular events and hospitalization among patients with CKD. In our study, we additionally studied effects of CVD status on the association between serum K and in-hospital mortality among CKD patients. Our study is the first to show the risk of in-hospital mortality among CKD patients with various admission serum K levels stratified by their CVD status. Although hyperkalemia was associated with the highest in-hospital mortality in CKD patients without CVD, hypokalemia was associated with the highest in-hospital mortality in CKD patients with CVD. These findings may aid risk stratification, future studies on modeling and risk prediction for mortality, and decision-making in hospitalized CKD patients with various admission potassium levels.
There are some limitations of this study that bear mention. (i) This is a single-center, retrospective study and (ii) the study patient population is predominantly Caucasian. Further studies with a more heterogeneous population are desirable to validate the clinical effects of admission serum K on in-hospital mortality. (iii) Although this is a large cohort study, a causal relationship cannot be inferred. Since serum K levels are tightly linked to the acid-base status of patients, admission potassium abnormalities may represent an epiphenomenon of metabolic disorders such as diabetes, dehydration or renal tubular dysfunction. If admission hypokalemia and hyperkalemia cause increased mortality (e.g. via the development of arrhythmias), clinical treatment may be beneficial to improve patient outcomes, especially with the higher risk hypokalemic CVD patients (regardless of CKD status) and hyperkalemic CKD patients (without CVD). Correction of K derangements is often prescribed by K supplementation, changes in dietary K, or K-altering medications.41–46 Whether these interventions improve in-hospital mortality in hyperkalemic or hypokalemic patients at hospital admission requires future study, optimally with a randomized controlled trial.
In summary, we demonstrate that hospitalized patients with admission serum K < 4.0 and >5.0 mEq/l were associated with an increased risk of in-hospital mortality. The mortality risk among patients with various admission potassium levels was affected by CKD and/or CVD status.
Supplementary material
Supplementary material is available at QJMED online.
Conflict of interest: None declared.