Abstract
Axial length (AL) is a significant indicator of eyeball development, but reports on the overall status of axial development in congenital cataract (CC) patients and its relationship with patient demographics, such as age, sex, and laterality, are rare. We prospectively investigated the AL of 1,586 patients ≤18 years old and undergoing cataract surgery in China from January 2005 to December 2014. Of these 3,172 eyes, a logarithmic correlation between AL and age in CC patients was calculated, and an age of approximately 2 years was found to be a turning point in the growth rate of AL. A considerable variation was observed in CC patients of the same age. Furthermore, 2–6 years old boys had longer AL than girls. The AL of affected eye in unilateral patients was longer than that of the contralateral eye in 2–6 years age group and longer than that of eye in bilateral CC patients in all age groups. These findings indicate that the development of the length of eyeballs in CC patients is influenced by multiple factors in addition to age. A full understanding of the distribution of AL may provide a useful reference for judging the timing of surgery in CC patients.
Similar content being viewed by others
Introduction
Axial length (AL) is a significant indicator of eyeball development and correlates with heredity1, development2,3, nutrition, and other environmental factors. Congenital cataract (CC) is a primary cause of pediatric cataract that also affects eyeball development, and the mechanisms that underlie the pathological changes to AL include defocusing4,5,6,7 and form deprivation8,9. Previous studies have revealed that the AL in pediatric CC patients is different from AL in healthy children10, and varies with different types and duration of cataract. However, reports on the overall status of axial development in CC patients and its relationship with patient demographics, such as age, sex, and laterality, are rare. Furthermore, the AL of CC patients is not only a crucial indicator of eyeball development and treatment prognosis, but also a vital contributor to intraocular lens (IOL) power calculation11. To reduce the effect of developmental opacity of the lens and vitreous on the accurate measurement of AL, contact A-scans, which show relatively good accuracy and maneuverability, are currently the most frequently used method for AL measurement before surgery in pediatric CC patients12,13. Most of the previous studies related to CC in clinical practice have proposed a treatment plan solely according to the age of the patient14, regardless of the actual development of AL, which may result in better and more precise treatment. Indeed, this approach has resulted in significant variability in the treatment effects observed in pediatric CC patients. Data on the overall distribution of AL before cataract surgery is critical for judging the timing of surgery and for improving the accuracy of postoperative IOL power in CC patients.
To our knowledge, few investigations have examined patient demographics and the distribution of AL before cataract surgery in a large cohort of Chinese pediatric patients with CC. In this prospective, large sample study, we aimed to investigate the overall status of axial development in CC patients younger than 18 years old and the relationship between AL development and patient demographics, including age, sex, and laterality, and our results provide a useful reference for the accurate timing of IOL implantation and CC treatment.
Results
Patient demographics
Complete AL data were collected for both eyes from a total of 1,586 pediatric CC patients (3,172 eyes) who were enrolled from January 2005 to December 2014. Most of these patients were confirmed residents from south China. Bilateral cataract patients represented a fairly large proportion (68.85%, 1092/1586) of the study population, and the remaining 31.15% (494/1586) of the subjects were unilateral patients. The ratio of boys to girls was 1.41 (928: 658), and the mean age of these subjects was 68.86 ± 54.90 months (95%CI 66.16–71.57). The constitution of all analyzed subjects in different ages was shown in Fig. 1, and the patients aged 0–6 years old constituted the highest patient proportions. The right eye was arbitrarily selected to represent the AL of bilateral individuals, because no difference of AL of two eyes in bilateral CC patients were found by paired T-test (t = 1.353, P = 0.176).
Among all of the analyzed CC patients, 82.16% (1303/1586) of them were undergoing cataract extraction and IOL implantation, with a mean age of 81.05 ± 52.27 months old, and the remaining 17.84% (283/1586) were undergoing cataract extraction and had a mean age of 12.74 ± 21.87 months old. The AL of the patients treated with the different surgical procedures mentioned above were significantly distinct: 22.90 ± 1.99 mm vs. 19.81 ± 2.01 mm, respectively.
Relationships between AL and age, gender, laterality
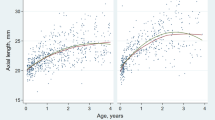
The logarithmic correlation of AL to age in CC patients ≤18 years old was presented in Fig. 2. The AL elongated more significantly in younger patients: a trend of faster growing before age 2 years with a plateau thereafter can be hypothesized.
Although AL measurements were age dependent and plateau in children >2 years old, considerable variation was observed in those CC patients of the same age (Fig. 3). The quartile deviations (differences between the 75th and 25th percentiles) of the 6 age subgroups were, from youngest to oldest, 2.05 mm, 2.59 mm, 2.27 mm, 1.66 mm, 2.47 mm and 3.03 mm, respectively.
Table 1 showed that the AL of boys aged of 2–6 years was statistically longer than that of girls of the same age in both bilateral and unilateral cataract group.
The AL of affected eyes in unilateral CC patients was longer than that in bilateral CC patients, as shown in Table 2. Table 3 showed that the longer AL in the affected eye than in the contralateral eye of unilateral CC patients was mainly distributed in patients 2–6 years old.
Discussion
AL is not only a crucial indicator of eyeball development but also a vital contributor to calculating IOL power in pediatric CC patients. Data on the overall distribution of AL before cataract surgery is critical for judging the timing of surgery and improving the accuracy of postoperative IOL power. However, published reports of axial development in pediatric CC patients are limited to studies with small sample sizes15,16 or studies of specific aspects, such as age or laterality. To the best of our knowledge, this is the largest study to provide information on the overall status of axial development and its relationship with patient demographics, including age, sex, and laterality, in a large cohort of Chinese pediatric CC patients (3,172 eyes of 1,586 CC patients) before cataract surgery. The Zhongshan Ophthalmic Center (ZOC) is one of the best, largest, and oldest eye hospitals that uses representative, current CC treatment methods in China17,18. All of the participants were confirmed to be from south China and this group of people represented the demographics and distribution of AL in CC patients in this region. Similar to what has been seen in other studies, pediatric patients presenting for CC surgery in this study were predominantly male and had bilateral cataracts19,20, which may be attributed to the traditional preference for sons in China or to gender-related genetic mechanisms that have previously been described21. The mean age of the CC patients presenting for the surgery in this study was 68.86 ± 54.90 months. However, most CC patients can be identified and treated within 100 days of birth in many developed countries because of national screening procedures22, indicating that delayed presentation to the hospital and late surgical treatment are very common in China. The ALs of patients treated with different surgical procedures (cataract extraction with/without IOL implantation) were distinct, which may be largely due to differences in age at the time of surgery (81.05 ± 52.27 months vs. 12.74 ± 21.87 months).
AL is known to increase with age, and the eye changes in size early in life and during childhood in healthy children, concomitant with height and overall development2,23. A logarithmic correlation between AL and age was also found in CC patients in the first 42 months of life in a retrospective study15. In this prospective study, similar findings were obtained in 1,586 CC patients who were less than 18 years old, likely resulting from the sharing of common biological pathways during overall growth and AL growth2. Furthermore, a remarkable rise in the AL of CC patients ≤2 years old was observed, which plateaued in older children, and this finding is partially consistent with a previous study showing that AL changes rapidly in the first 18 months of life in the non-cataractous eyes of unilateral CC patients24. In addition, AL is of vital importance for IOL power calculations in CC patients. The long-term results for CC after primary IOL implantation remains controversial in children less than 2 years of age, who experience rapid elongation in AL. Many researchers oppose primary IOL implantation in very young children, complaining a combination of greater prediction error25, future myopic shift26, unmatched IOL size16, and a higher frequency of postoperative complications27. Infant Aphakia Treatment Study Group (IATS) have proposed that delaying IOL implantation until later years after most of the growth in AL has occurred benefits for selecting a more appropriate IOL power for implantation28. The rapid growth rate of AL in CC patients less than 2 years old observed in this study provides a useful reference, with exact data, in terms of AL, for objections to implanting IOL in very young CC children. While some small case series have reported relatively good visual outcomes following unilateral IOL implantation during infancy29,30, more recently, well-controlled myopic shift and reasonably good visual acuity after primary IOL implantation were reported in a retrospective study in India of children who underwent surgery for CC when they were less than 2 years old16. However, this clinic-based study was likely not representative because it involved only 13 participants and showed severe selection bias. Thus, determining long-term results following primary IOL implantation in CC patients who are less than 2 years old will require additional large-scale investigations31.
A positive correlation between AL and age is generally accepted, but there is very little published information that specifically describes the distribution of AL in CC patients of the same age. Although placing an IOL in patients more than 2 years old is a relatively better option according to the growth rate of AL, considerable variations of AL observed in CC patients (2–18 years old) of the same age in the present study should also be taken into account. The quartile deviations of AL of patients of the same age were 1.66–2.59 mm in patients aged of 2–6 years, and likely resulted in 7.77 diopters (D) of refractive error (3 D per millimeter), at most. Most previous studies related to CC clinical practices have supported a treatment plan based solely on the age of the patient14; however, an accurate measurement of AL should be taken into consideration to achieve better and more precise results, even in patients of the same age.
The increase in AL follows the overall growth and development of body size, which is regulated largely by the sex steroids (androgens and estrogens). Indeed, sex-linked differences in the AL of infants and children have been reported in the literature. Isenberg et al.32 found that the eyes of male infants grow faster than those of female infants, and Larsen et al.33 and Trivedi et al.34 noted shorter mean AL in girls than in boys in both non-cataractous eyes and cataractous eyes. However, Capozzi et al.15 reported no difference in AL according to sex. In the present study, we found that the AL in boys was significantly longer than that in girls in 2–6 years old age subgroup. One possible explanation for this difference is the close correlation between AL and head size, which has been previously reported35,36; for example, boys have a larger head circumference than girls before 5 years of age, according to the data published on the website of the World Health Organization (WHO).
The impact of cataracts on the development of the eye is not related only to the age and sex of the patient but also depends largely on laterality. A shorter AL was previously noted in young pediatric bilateral CC patients (≤42 months old) compared to the affected eyes of patients with unilateral CC involvement15. Similar findings were also revealed in the present study. However, Trivedi et al.34, in contrast to our results, reported that cases of bilateral cataracts had a longer AL than those with a unilateral cataract in patients younger than 60 months of age, but a shorter AL than the eyes with a unilateral cataract in patients older than 60 months of age. One possible explanation for these differences is the race of the participants (Caucasian or African-American vs. Chinese), which may contribute to distinct outcomes because race is known to influence biometry results in children. Differences in the study type, grouping situation and analysis of sample size could also account for these discrepancies. In patients with unilateral cataract, the cataractous eye was reported to have a significantly shorter AL than the contralateral normal eye in CC patients who were less than 7 months old9. Capozz et al.15 reported no difference in AL among unilateral CC patients who were less than 42 months old. However, results of the present study show that cataractous eyes have longer AL than non-cataractous eyes in patients with a unilateral cataract in different age subgroups, and this is partially in line with the finding of Trivedi and associates34. Together, these findings indicate that the AL of unilateral CC patients is likely age-dependent and related to the duration of form deprivation. The exact relationship between the AL of eyes in CC patients with differences in laterality is affected by numerous factors and remains to be further studied.
The results of this study must be assessed within the context of its limitations. First, the contact A-scan measurements used in this study likely yielded shorter AL measurements than those from immersion A-scans in pediatric eyes12. However, this deviation was minimized by using the same apparatus for all subjects; moreover, contact A-scans remains the most appropriate tool for CC patients who are unable to cooperate for long periods, and these scans are an easier tool for examiners with large workloads to use. Second, the data do not provide a complete representation of the population and only relate to surgical patients for whom we gathered complete data regarding AL in the best eye center in south China, which receives admissions that are biased toward patients who are unsuitable for surgery and who present with complicated or serious diseases. Despite these limitations, the results of this study describe the overall distribution of AL before cataract surgery in Chinese pediatric patients because of its large sample size (3,172 eyes of 1,586 patients) and the representativeness of its population in south China.
In conclusion, pediatric patients who presented for surgery and were included in this study were predominantly male and had bilateral cataracts. The AL of CC patients with different ages, genders and laterality was distinct, indicating that the development of the length of eyeballs in CC patients is influenced by multiple factors in addition to age. A full understanding of the distribution of AL and accurate measurements of AL will likely provide a useful reference for judging the timing of surgery and improving the accuracy of postoperative IOL power achieved in CC patients.
Methods
Subjects
This study was a prospective large cohort research, which was included as one of our series ongoing studies of the Childhood Cataract Program of the Chinese Ministry of Health (CCPMOH). Patients with CC who were undergoing cataract extraction with/without IOL implantation were consecutively recruited during pre-operation screening at the ZOC, Guangdong, China, from 1 January 2005 to 31 December 2014. The medical history and systematic history of each of the patients were carefully learned. The CC in this study was defined as a cataract caused by heredity or developmental disorders. All patients were examined and confirmed as a CC victim by at least three experienced ophthalmologists before the cataract surgical procedure, which included a detailed slit-lamp examination and thorough ophthalmoscopy through dilated pupils. Recruited CC patients were no more than 18 years old and were undergoing cataract extraction with/without IOL implantation. Patients with congenital intrauterine infection cataract (such as rubella cataract), complicated cataract (such as uveitis cataract), metabolic cataract (such as tetany cataract), and traumatic cataract were excluded. Patients with severe ocular disease, infection, cough, or other systemic diseases likely to affect the AL examination and surgical procedure were also excluded. To obtain a better analysis, patients were divided into several groups according to age, sex and laterality, when necessary.
A-scan examination
A contact A-scan (B-SCAN-Vplus/BIOVISION, Quantel Medical, France) was used to obtain the AL measurements before surgery. The A-scan unit was equipped with a 10 MHz transducer probe, and the velocities were set as follows: 1,641 m/s for the cornea and lens and 1,532 m/s for the aqueous and vitreous. All patients were tested by the same examiner, and some of the patients who were unable to actively cooperate were sedated using 10% chloral hydrate (0.8 ml/kg, oral or rectal administration). Applanation ultrasound was performed after instillation of one drop of topical anesthetic (0.5% Alcaine, Alcon, USA) to the lower conjunctiva. Each eye was measured 10 times, and the mean measurements were used. This study was approved by the Human Research Ethics Committee of the ZOC at Sun Yat-sen University. All procedures adhered to the tenets of the Declaration of Helsinki, and written informed consent was obtained from at least one parent of each patient.
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS ver. 19.0, Chicago, IL, USA). Absolute frequency (n) and relative frequency (%) were used to describe qualitative variables; mean and standard deviation (mean ± SD) were used for age, AL, and other quantitative variables of CC patients. The Kolmogorov-Smirnov test was used to evaluate the normality of the distribution for all variables. The T-test for independent samples was used to analyze the difference of AL between patients with different age, gender and laterality, and the paired T-test was used to evaluate the difference of AL between the affected eye and the fellow eye in unilateral CC patients. A P value < 0.05 was considered statistically significant.
Additional Information
How to cite this article: Lin, H. et al. Distribution of Axial Length before Cataract Surgery in Chinese Pediatric Patients. Sci. Rep. 6, 23862; doi: 10.1038/srep23862 (2016).
References
Zhang, J. et al. Shared genetic determinants of axial length and height in children: the Guangzhou twin eye study. Archives of ophthalmology (Chicago, Ill: 1960) 129, 63–68, doi: 10.1001/archophthalmol.2010.323 (2011).
Wang, D., Ding, X., Liu, B., Zhang, J. & He, M. Longitudinal changes of axial length and height are associated and concomitant in children. Investigative ophthalmology & visual science 52, 7949–7953, doi: 10.1167/iovs.11-7684 (2011).
Wong, T. Y., Foster, P. J., Johnson, G. J., Klein, B. E. & Seah, S. K. The relationship between ocular dimensions and refraction with adult stature: the Tanjong Pagar Survey. Investigative ophthalmology & visual science 42, 1237–1242 (2001).
Zhu, X., Park, T. W., Winawer, J. & Wallman, J. In a matter of minutes, the eye can know which way to grow. Investigative ophthalmology & visual science 46, 2238–2241, doi: 10.1167/iovs.04-0956 (2005).
Graham, B. & Judge, S. J. The effects of spectacle wear in infancy on eye growth and refractive error in the marmoset (Callithrix jacchus). Vision research 39, 189–206 (1999).
Wallman, J. et al. Moving the retina: choroidal modulation of refractive state. Vision research 35, 37–50 (1995).
Read, S. A., Collins, M. J. & Sander, B. P. Human optical axial length and defocus. Investigative ophthalmology & visual science 51, 6262–6269, doi: 10.1167/iovs.10-5457 (2010).
Bremond-Gignac, D., Copin, H., Lapillonne, A. & Milazzo, S. Visual development in infants: physiological and pathological mechanisms. Current opinion in ophthalmology 22 Suppl, S1–8, doi: 10.1097/01.icu.0000397180.37316.5d (2011).
Lambert, S. R. et al. The infant aphakia treatment study: design and clinical measures at enrollment. Archives of ophthalmology (Chicago, Ill: 1960) 128, 21–27, doi: 10.1001/archophthalmol.2009.350 (2010).
Zhan, J., Lin, H., Zhang, X., Chen, W. & Liu, Y. Significance of axial length monitoring in children with congenital cataract and update of measurement methods. Eye science 28, 95–102 (2013).
Vanderveen, D. K. et al. Predictability of intraocular lens power calculation formulae in infantile eyes with unilateral congenital cataract: results from the Infant Aphakia Treatment Study. Am J Ophthalmol 156, 1252–1260 e1252, doi: 10.1016/j.ajo.2013.07.014 (2013).
Trivedi, R. H. & Wilson, M. E. Axial length measurements by contact and immersion techniques in pediatric eyes with cataract. Ophthalmology 118, 498–502, doi: 10.1016/j.ophtha.2010.06.042 (2011).
Wilson, M. E. & Trivedi, R. H. Axial length measurement techniques in pediatric eyes with cataract. Saudi journal of ophthalmology: official journal of the Saudi Ophthalmological Society 26, 13–17, doi: 10.1016/j.sjopt.2011.11.002 (2012).
Wilson, M. E. Jr. et al. ASCRS white paper. Hydrophobic acrylic intraocular lenses in children. Journal of cataract and refractive surgery 33, 1966–1973, doi: 10.1016/j.jcrs.2007.06.047 (2007).
Capozzi, P., Morini, C., Piga, S., Cuttini, M. & Vadala, P. Corneal curvature and axial length values in children with congenital/infantile cataract in the first 42 months of life. Investigative ophthalmology & visual science 49, 4774–4778, doi: 10.1167/iovs.07-1564 (2008).
Sukhija, J., Ram, J., Gupta, N., Sawhney, A. & Kaur, S. Long-term results after primary intraocular lens implantation in children operated less than 2 years of age for congenital cataract. Indian journal of ophthalmology 62, 1132–1135, doi: 10.4103/0301-4738.149131 (2014).
Lin, H. T., Luo, L. X., Chen, W. R. & Liu, Y. Z. Eye health is everyone’s responsibility: China’s first Western-style eye hospital improves in the prevention of blindness. Int J Ophthalmol 5, 638–640, doi: 10.3980/j.issn.2222-3959.2012.05.19 (2012).
Lin, H. et al. Effectiveness of a short message reminder in increasing compliance with pediatric cataract treatment: a randomized trial. Ophthalmology 119, 2463–2470, doi: 10.1016/j.ophtha.2012.06.046 (2012).
Katibeh, M., Eskandari, A., Yaseri, M., Hosseini, S. & Ziaei, H. The gender issue in congenital and developmental cataract surgery. Journal of ophthalmic & vision research 8, 308–313 (2013).
Lin, H. et al. Congenital cataract: prevalence and surgery age at Zhongshan Ophthalmic Center (ZOC). PloS one 9, e101781, doi: 10.1371/journal.pone.0101781 (2014).
Chen, W. et al. A missense mutation in CRYBB2 leads to progressive congenital membranous cataract by impacting the solubility and function of betaB2-crystallin. Plos One 8, e81290, doi: 10.1371/journal.pone.0081290 (2013).
Haargaard, B., Nystrom, A., Rosensvard, A., Tornqvist, K. & Magnusson, G. The Pediatric Cataract Register (PECARE): analysis of age at detection of congenital cataract. Acta Ophthalmol 93, 24–26, doi: 10.1111/aos.12445 (2015).
Ojaimi, E. et al. Effect of stature and other anthropometric parameters on eye size and refraction in a population-based study of Australian children. Investigative ophthalmology & visual science 46, 4424–4429, doi: 10.1167/iovs.05-0077 (2005).
Hussain, R. N., Shahid, F. & Woodruff, G. Axial length in apparently normal pediatric eyes. European journal of ophthalmology 24, 120–123, doi: 10.5301/ejo.5000328 (2014).
Kekunnaya, R. et al. Accuracy of intraocular lens power calculation formulae in children less than two years. American journal of ophthalmology 154, 13–19.e12, doi: 10.1016/j.ajo.2011.11.031 (2012).
Hoevenaars, N. E., Polling, J. R. & Wolfs, R. C. Prediction error and myopic shift after intraocular lens implantation in paediatric cataract patients. The British journal of ophthalmology 95, 1082–1085, doi: 10.1136/bjo.2010.183566 (2011).
Solebo, A. L., Russell-Eggitt, I., Cumberland, P. M. & Rahi, J. S. Risks and outcomes associated with primary intraocular lens implantation in children under 2 years of age: the IoLunder2 cohort study. The British journal of ophthalmology, doi: 10.1136/bjophthalmol-2014-306394 (2015).
Plager, D. A., Lynn, M. J., Buckley, E. G., Wilson, M. E. & Lambert, S. R. Complications in the first 5 years following cataract surgery in infants with and without intraocular lens implantation in the Infant Aphakia Treatment Study. American journal of ophthalmology 158, 892–898, doi: 10.1016/j.ajo.2014.07.031 (2014).
Autrata, R., Rehurek, J. & Vodickova, K. Visual results after primary intraocular lens implantation or contact lens correction for aphakia in the first year of age. Ophthalmologica . Journal international d’ophtalmologie. International journal of ophthalmology. Zeitschrift fur Augenheilkunde 219, 72–79, doi: 10.1159/000083264 (2005).
Lambert, S. R. et al. A comparison of grating visual acuity, strabismus, and reoperation outcomes among children with aphakia and pseudophakia after unilateral cataract surgery during the first six months of life. Journal of AAPOS: the official publication of the American Association for Pediatric Ophthalmology and Strabismus/American Association for Pediatric Ophthalmology and Strabismus 5, 70–75, doi: 10.1067/mpa.2001.111015 (2001).
Lambert, S. R. et al. Comparison of contact lens and intraocular lens correction of monocular aphakia during infancy: a randomized clinical trial of HOTV optotype acuity at age 4.5 years and clinical findings at age 5 years. JAMA ophthalmology 132, 676–682, doi: 10.1001/jamaophthalmol.2014.531 (2014).
Isenberg, S. J. et al. Growth of the internal and external eye in term and preterm infants. Ophthalmology 102, 827–830 (1995).
Larsen, J. S. The sagittal growth of the eye. 3. Ultrasonic measurement of the posterior segment (axial length of the vitreous) from birth to puberty. Acta Ophthalmol (Copenh) 49, 441–453 (1971).
Trivedi, R. H. & Wilson, M. E. Biometry data from caucasian and african-american cataractous pediatric eyes. Investigative ophthalmology & visual science 48, 4671–4678, doi: 10.1167/iovs.07-0267 (2007).
Saw, S. M. et al. The relation between birth size and the results of refractive error and biometry measurements in children. The British journal of ophthalmology 88, 538–542 (2004).
Ojaimi, E. et al. Impact of birth parameters on eye size in a population-based study of 6-year-old Australian children. American journal of ophthalmology 140, 535–537, doi: 10.1016/j.ajo.2005.02.048 (2005).
Acknowledgements
This clinical study was supported by the Ministry of Science and Technology of China Grants (973 program, 2015CB964600), the Key Projects for Hospital Clinical Disciplines of the Ministry of Health of China in 2010–2012 (Project No. 175 in Document 439 of the Planning and Finance Secretary of the Ministry of Health), the Pearl River Science and Technology New Star (Grant No. 2014J2200060) Project of Guangzhou City, the Guangdong Provincial Natural Science Foundation for Distinguished Young Scholars of China (Grant No. 2014A030306030), Youth Science and Technology Innovation Talents Funds in the Special Support Plan for High Level Talents in Guangdong Province (Grant No. 2014TQ01R573), the Outstanding Young Teacher Cultivation Projects in Guangdong Province(No. YQ2015006), the Science and Technology Program of Guangdong Province (Grant No. 2013B020400003) and the Intensive Cultivation Projects (2015ykzd11) for Young Teaching Staff of Sun Yat-sen University, from the Fundamental Research Funds for the Central Universities and the Fundamental Research Funds of State Key Laboratory of Ophthalmology (Grant No. 2015QN01). The sponsors of the study played no role in the study protocol design, data collection, data analysis, data interpretation, manuscript preparation, or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
H.T.L., D.R.L., W.R.C. and Y.Z.L. were involved in the study’s conception, design, and funding; H.T.L., D.R.L., J.J.C., W.R.C. and Y.Z.L. conducted the study; H.T.L., D.R.L., J.J.C., Z.L.L., X.Y.L., B.Z., H.C., W.C. and L.Z. collected the data; H.T.L., D.R.L., J.J.C., J.C.L. and W.R.C. analyzed the data; H.T.L. and D.R.L. wrote the manuscript; H.T.L., D.R.L., J.J.C., L.X.L., Z.L.L., X.H.W., E.P.L., W.R.C. and Y.Z.L. reviewed the manuscript; and all authors gave final approval of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Lin, H., Lin, D., Chen, J. et al. Distribution of Axial Length before Cataract Surgery in Chinese Pediatric Patients. Sci Rep 6, 23862 (2016). https://doi.org/10.1038/srep23862
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep23862
This article is cited by
-
Factors associated with progressive anisometropia after bilateral intraocular lens implantation in patients with pediatric cataract
Eye (2024)
-
Higher HbA1c may reduce axial length elongation in myopic children: a comparison cohort study
Acta Diabetologica (2021)
-
Prediction of postoperative complications of pediatric cataract patients using data mining
Journal of Translational Medicine (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.