Abstract
We performed a large, long-term cohort study to evaluate the association of renin-angiotensin-aldosterone system gene polymorphisms and baseline phenotypes to all-cause mortality among patients with angiographically confirmed coronary atherosclerosis. The study included 1075 subjects who underwent coronary angiography. Patients were genotyped for eight polymorphisms (rs4343, rs5186, rs5182, rs5049, rs5051, rs699, rs4762 and rs1799998) and their baseline plasma angiotensin II and aldosterone levels were measured. The interval between baseline and follow-up time-points ranged from 6.39 to 9.59 years. The results of multivariate regression analysis further indicated that high baseline angiotensin II levels (1.226 (1.024–1.468), p = 0.027) were independently associated with all-cause death. Therefore, we found that an increased baseline plasma angiotensin II level was associated with higher long-term all-cause mortality, even after correcting for established cardiovascular risk factors.
Similar content being viewed by others
Introduction
As a complex, multifactorial disease that is influenced by multiple pathophysiologic, genetic and environmental factors, atherosclerotic cardiovascular disease (CVD) is a major health burden worldwide1,2,3. In addition to other well-recognized risk factors, the renin-angiotensin-aldosterone system (RAAS) has been implicated in the development of atherosclerosis and coronary heart disease4. The RAAS regulates blood pressure, the sodium and water balance and cardiovascular and renal homeostasis5.
More than a century of research on the RAAS has uncovered the widespread involvement of angiotensin II (Ang II) in the pathophysiology of CVDs. As the major effector peptide of the RAAS, Ang II crucially mediates the initiation and perpetuation of inflammatory diseases, most notably in atherogenesis6. Under pathophysiologic conditions, RAAS contributes to atherosclerotic development through both direct and indirect means (e.g., through the actions of the RAAS on other systems). RAAS genes have been extensively studied as candidate genes for atherosclerosis and coronary artery disease (CAD)7,8,9,10. In a study in New Zealand, genetic variation within the RAAS was associated with cardiovascular risk factors and poorer survival11.
We previously showed that the RAAS gene load and interactions between gene polymorphisms and environment risk factors were associated with an increased risk of CAD12. However, to date, the association of RAAS gene polymorphisms, phenotypes and long-term mortality in subjects with CAD has not been reported. Therefore, we performed a prospective analysis to evaluate the impact of RAAS gene polymorphisms and phenotypes on the risk of all-cause mortality in a large cohort of Chinese patients referred for coronary angiography.
Results
Baseline characteristics
Table 1 shows the baseline demographic and clinical characteristics of the 1075 subjects (803 males) enrolled in the study. The median age (quartile range) was 63.00 (55.00–70.00) years. There were significant differences between male and female subjects for age (p = 0.048), smoking status (p = 0.048), drinking status (p < 0.001), systolic blood pressure (SBP, p = 0.001), total cholesterol (TCH, p < 0.001), triglyceride (TG, p = 0.009), fasting high-density lipoprotein cholesterol (HDL-c, p < 0.001), fasting low-density lipoprotein cholesterol (LDL-c, p < 0.001) and Gensini's Score (p < 0.001), but not for body mass index (BMI, p = 0.456), diastolic blood pressure (DBP, p = 0.467), fasting blood glucose (FBG, p = 0.709), angiotensin II (p = 0.496), aldosterone (p = 0.304), or the genotype of the eight tested SNPs.
Tables 2 and 3 show the baseline characteristics of subjects grouped by their angiotensin II or aldosterone level, respectively (with quartile values used as cutoff points). Significant differences in FBG (p = 0.001) and Gensini's scores (p = 0.002) were observed among subjects grouped by their angiotensin II level. The distribution of the rs5051 genotype differed between the angiotensin II groups (p = 0.026); however, this finding was not statistically significant after Bonferroni correction for multiple testing. HDL-c (p = 0.019) and angiotensin II (p = 0.018) distributions were significantly different among subjects grouped by aldosterone level. This finding was not statistically significant after Bonferroni correction for multiple testing.
Association of RAAS SNPs with angiotensin II and aldosterone levels
Table 4 displays the median (quartile range) values of angiotensin II and aldosterone per genotype of each SNP. A difference in angiotensin II level was observed among rs5051 genotype carriers in the additive genetic model (CC vs. TC vs. TT, p = 0.021). However, this finding was not statistically significant after Bonferroni correction for multiple testing. No other significant association of RAAS SNPs with angiotensin II and aldosterone levels was found.
Univariate and multivariate Cox proportional hazard analyses for all-cause mortality
The interval between baseline and follow-up ranged from 6.39 to 9.59 years. The median follow-up time was 7.74 years. Among the 1075 subjects, 117 subjects died during follow-up.
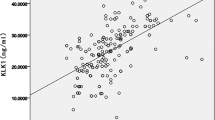
Table 5 presents the univariate Cox proportional HRs (95% CIs) for all-cause mortality, according to the baseline characteristics of subjects. Patients in the high baseline age (4.089 (3.038–5.504), p < 0.001), SBP (1.193 (1.029–1.384), p = 0.019), Gensini's score (1.356 (1.145–1.607), p < 0.001) and angiotensin II (1.299 (1.095–1.541), p = 0.003) categories had increased risks of all-cause death compared to patients in the corresponding low baseline categories. A protective effect for all-cause mortality was observed for baseline DBP (0.839 (0.713–0.987), p = 0.034), TG (0.830 (0.703–0.979), p = 0.027) and rs5049 (CC vs. TC + TT) (0.590 (0.374–0.931), p = 0.023). However, the protective effect of rs5049 (CC vs. TC + TT) for all-cause mortality was not statistically significant after Bonferroni correction for multiple testing.
To explore which of these baseline variables were independent predictors of all-cause mortality, forward-conditional multivariate regression analyses were performed, with age, gender, smoking and drinking status, BMI, SBP, DBP, TCH, TG, FBG, HDL-c, LDL-c, Gensini's score, angiotensin II level, aldosterone level and the genotype of 8 SNPs as covariates. The results of the multivariate regression analyses indicated that high baseline age (4.174 (3.024–5.763), p < 0.001), drinking status (1.681 (1.087–2.600), p = 0.020) and angiotensin II levels (1.226 (1.024–1.468), p = 0.027) were independently associated with all-cause death during follow-up (Table 6). A 25% increase in angiotensin II level was related to a 23% higher risk of death during follow up, indicating that lower angiotensin II level was related to higher survival probability.
Discussion
We performed a hospital-based cohort study of consecutive adult Chinese subjects with angiographically confirmed coronary atherosclerosis. We found that an increased baseline plasma angiotensin II level was associated with higher long-term all-cause mortality, even after correcting for established cardiovascular risk factors. However, we did not find any significant association of RAAS gene polymorphisms with long-term all-cause mortality.
Clinical studies have demonstrated that the RAAS plays an important role in atherogenesis, associated with long-term mortality13. In the Intermountain Heart Collaborative study of 1165 patients with CAD (≥70% stenosis on coronary angiogram), elevated baseline plasma renin activity was associated with cardiac morbidity and mortality in patients with CAD but normal left ventricular function and no previous myocardial infarction (MI) or heart failure14. Other studies found that the baseline plasma renin activity had a significant, independent, specific and direct long-term association with CVD mortality in subjects with hypertension15 and in patients referred for coronary angiography16. Plasma aldosterone levels have been associated with all-cause and cardiovascular mortality in high-risk cardiovascular populations. For example, in the SMART study, the plasma aldosterone level was independently associated with risks of major vascular events, vascular mortality and atherosclerotic burden in patients with stable CAD17.
To the best of our knowledge, no published report has assessed the association of RAAS gene polymorphisms and phenotypes with long-term mortality in CAD subjects. In the present study, we observed a significant association of the baseline plasma angiotensin II level with long-term all-cause mortality in adult Chinese subjects with CAD, which was maintained after we had adjusted for established cardiovascular risk factors and RAAS gene polymorphisms. We did not find any significant association of RAAS gene polymorphisms with long-term all-cause mortality. In a 9-year follow-up study of Italian subjects who had experienced acute MI at a young age, polymorphisms in RAAS genes (ACE and CYP11B2) were found to be important in the onset of a first acute MI, but not in the long-term disease progression18. Our results are consistent with the results of that previous study, although larger collaborative studies are needed to confirm these findings. In addition, as the downstream product of Ang II, the plasma aldosterone concentration was not correlated with the plasma Ang II concentration or all-cause mortality in the present study. Thus, the mechanism underlying the phenomenon will require further study in the future.
Angiotensins are peptide hormones that are derived from the protein precursor angiotensinogen by the sequential actions of proteolytic enzymes. Angiotensin II critically affects the function of virtually all organs, including the heart, kidney, vasculature and brain, possessing both beneficial and pathological effects. Acute stimulation with angiotensin II regulates salt/water homeostasis and vasoconstriction, modulating blood pressure, whereas chronic stimulation promotes hyperplasia and hypertrophy of the vascular smooth muscle cells. In addition, long-term exposure to angiotensin II plays a vital role in cardiac hypertrophy and remodeling, in-stent restenosis, reduced fibrinolysis and renal fibrosis19. However, the exact biomolecular mechanisms that underlie the association of the angiotensin II level with long-term mortality in the present study remain unknown and will require further analysis.
The exploratory study discussed in this paper had some limitations. First, although the estimated statistical power based on the sample size was adequate, the sample size of the cohort study was limited. Prospective studies with larger sample sizes are needed to confirm our findings. Second, the status of patient treatment with angiotensin-converting enzyme inhibitor or angiotensin receptor blockers was not considered, although the angiotensin II and aldosterone levels can be reduced due to drug treatment. Finally, although the study was a prospective one and vital status information for the subjects was continuously obtained from local person registries, the classification of death from CVD and non-CVD causes was not conducted.
The results of the present study show, for what we believe is the first time, that the baseline plasma angiotensin II level is associated with long-term all-cause mortality in Chinese subjects referred for coronary angiography, even after correcting for traditional cardiovascular risk factors and RAAS gene SNPs.
Methods
Study subjects
From 2004 to 2006, a total of 1089 consecutive subjects who underwent coronary angiography for suspected or known coronary atherosclerosis at the First Affiliated Hospital of Nanjing Medical University in China were enrolled in the study. The exclusion criteria for subjects have been described elsewhere20. In brief, subjects with spastic angina pectoris, infectious processes within the last 2 weeks, heart failure, adrenal dysfunction, or thyroid dysfunction were excluded. The study was approved by the ethics committee of the First Affiliated Hospital of Nanjing Medical University. All subjects gave their written informed consent before participation. And, the experiments in the study were performed in accordance with the approved guidelines and regulations.
For follow-up, information on vital status was continuously obtained from local person registries. Among the 1089 subjects, 14 subjects failed to have complete clinical follow-up data. Therefore, 1075 subjects formed the study cohort. The follow-up of the final cohort was completed in October, 2012.
Coronary angiography
Coronary arteries were cannulated by the Judkins technique21 with 6F catheters. Angiography was recorded at 30 frames/s. The presence of stenosis of the coronary arteries was evaluated after the direct intracoronary injection of isosorbide dinitrate (ISDN; 2.5 mg/5 mL solution over 20 s). One minute after ISDN was injected through the Judkins catheter, coronary angiography was performed from several projections. The severity of coronary atherosclerosis was defined by Gensini's score system, which assumes that the severity of coronary heart disease is a consequence of the functional significance of the vascular narrowing and the extent of the area perfused by the involved vessel(s). In this scoring system, a greater reduction of the lumen diameter is assigned a higher score than a distal lesion22.
Cigarette smoking and alcohol intake
The subjects' cigarette smoking and alcohol intake statuses were assessed with a standardized questionnaire. They were classified as “never” (smoking/drinking) or “smoking/drinking”. The latter group included both former and current smokers or drinkers. Smoking was defined as smoking at least 1 cigarette per day within the last month. Drinking was defined as consuming at least 50 g/week of alcohol.
Anthropometric and laboratory measurements
Anthropometric measurements were performed after the patients had removed their shoes and upper garments and donned an examining gown. Each measurement was performed twice and the average was used in the analysis. Height was measured to the nearest 0.1 cm with a wall-mounted stadiometer. Weight was measured to the nearest 0.1 kg with a hospital balance beam scale. Body mass index (BMI) was calculated as the weight (kg) divided by the square of height (m2). Blood pressure was measured in the right arm with the participant seated and the arm bared. Three readings were recorded for each individual and the average was recorded. The total cholesterol (TCH, mmol/L), triglyceride (TG, mmol/L), fasting blood glucose (FBG, mmol/L) and fasting high- and low-density lipoprotein cholesterol (HDL-c and LDL-c, respectively; mmol/L) levels were determined by enzymatic procedures on an automated autoanalyzer (AU 2700 Olympus, 1st Chemical Ltd, Japan).
DNA genotyping
Eight single-nucleotide polymorphisms (SNPs) were selected for analysis, based on previous reports of their potential functionality, validated allele frequency and sequence-proven allelic variation. Genomic DNA was extracted from blood by the saturated sodium chloride method23,24. DNA fragments were amplified by polymerase chain reaction. The selection criterion used for the eight final SNPs was that these polymorphisms had been associated with cardiovascular disease in previous studies. Eight polymorphisms in four genes involved in the RAAS were selected as candidate loci: namely, G2350A (rs4343) in exon 17 of the angiotensin converting enzyme (ACE) gene25; 1166A → C (rs5186) in the angiotensin II type 1 receptor (AGTR1) gene26; 573C/T (rs5182) in the angiotensin II type 1 receptor (AGTR1) gene27; G-217A (rs5049), G-6A (rs5051), M235T (rs699; T4072C) and T174M (rs4762; C3889T) of the angiotensinogen (AGT) gene28; and -344C → T (rs1799998) in the aldosterone synthase (CYP11B2) gene29. TaqMan-MGB predesigned SNP assays (ABI, Applied Biosystems, Foster City, CA), were used to genotype the candidate loci. The genotyping procedure has been described in detail elsewhere12.
Measurement of angiotensin II and aldosterone
After an overnight fast, venous blood was sampled in the morning before coronary angiography, with the participants in the supine position for 5 to 10 min before phlebotomy. The plasma angiotensin II concentration was determined by a colorimetric immunoassay kit, which provides results in 3.5 hours (Enzo Life Sciences, Inc., Exeter, UK; cross reactivities: angiotensin II 100%, sensitivity: 4.6 pg/ml, range: 0.1–500,000 pg/mL). The plasma aldosterone concentration was determined by a colorimetric competitive enzyme immunoassay kit, which provides results approximately overnight (Enzo Life Sciences, Inc.; low reactivity with other steroids, sensitivity: 4.7 pg/mL, range: 3.9–250 pg/mL).
Power and statistical analyses
Prior to association analysis, power analyses were performed with the Power and Sample Size Calculation program (http://biostat.mc.vanderbilt.edu/wiki/Main/PowerSampleSize)30,31. A Cox regression of the log hazard ratio on a covariate with a standard deviation (SD) of 1.5000 based on a sample of 117 observations achieves 84% power at a 0.05000 significance level to detect a regression coefficient equal to 0.1823.
For association studies, data were analyzed with the Statistics Package for Social Sciences (ver. 16.0; SPSS Incorporated, Chicago, IL, USA). Subjects were classified into four groups according to their angiotensin II and aldosterone levels. Quartile values were used as cutoff points, such that each group included an approximately equal number of patients. This approach was used to minimize any bias that may have been produced in the statistical analysis.
Normally distributed data, such as BMI, were presented as the mean ± SD and compared with the independent-samples t-test or one-way analysis of variance (ANOVA). Skewed data, including age, systolic and diastolic blood pressures (SBP and DBP, respectively; mmHg), TCH, TG, FBG, fasting HDL-c and LDL-c, Gensini's Score and angiotensin II and aldosterone levels were expressed as the median (quartile range) and compared by the Mann-Whitney U or Kruskal-Wallis H test. Categorical variables, including gender, smoking and drinking statuses and genotype of the SNPs, were compared among groups of patients by chi-squared analysis. Hazard ratios (HRs) and 95% confidence intervals (CIs) for all-cause mortality were calculated with Cox proportional hazard analyses to estimate the relative risk of all-cause mortality by baseline, demographic and clinical characteristics. Continuous variables, including age, SBP, DBP, TCH, TG, FBG, fasting HDL-c and LDL-c, Gensini's Score and angiotensin II and aldosterone levels, were grouped by quartile values for the Cox regression analysis. The dominant genetic model was chosen for the RAAS pathway based on previous studies. Differences were considered to be significant if the null hypothesis could be rejected with >95% confidence. All p-values are two-tailed. The overall, intra-group and inter-group genetic diversity levels were calculated with a Bonferroni correction for all significance levels.
References
Roger, V. L. et al. Executive summary: heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 125, 188–197 (2012).
Murray, C. J. & Lopez, A. D. Global mortality, disability and the contribution of risk factors: Global Burden of Disease Study. Lancet. 349, 1436–1442 (1997).
McPherson, R. et al. A common allele on chromosome 9 associated with coronary heart disease. Science. 316, 1488–91 (2007).
Schmieder, R. E., Hilgers, K. F., Schlaich, M. P. & Schmidt, B. M. Renin–angiotensin system and cardiovascular risk. Lancet. 369, 1208–1219 (2007).
Roscioni, S. S., Heerspink, H. J. & de Zeeuw, D. The effect of RAAS blockade on the progression of diabetic nephropathy. Nat Rev Nephrol. 2013 Dec 3. 10.1038/nrneph.2013.251. [Epub ahead of print].
Ferrario, C. M. Role of angiotensin II in cardiovascular disease therapeutic implications of more than a century of research. J Renin Angiotensin Aldosterone Syst. 7, 3–14 (2006).
Ferrario, C. M. & Strawn, W. B. Role of the renin-angiotensin-aldosterone system and proinflammatory mediators in cardiovascular disease. Am J Cardiol. 98, 121–8 (2006).
Kretowski, A. et al. Polymorphisms of the renin-angiotensin system genes predict progression of subclinical coronary atherosclerosis. Diabetes. 56, 863–71 (2007).
Gluba, A., Banach, M., Mikhailidis, D. P. & Rysz, J. Genetic determinants of cardiovascular disease: the renin-angiotensin-aldosterone system, paraoxonases, endothelin-1, nitric oxide synthase and adrenergic receptors. In Vivo. 23, 797–812 (2009).
Durante, A. et al. Role of the renin-angiotensin-aldosterone system in the pathogenesis of atherosclerosis. Curr Pharm Des. 18, 981–1004 (2012).
Ellis, K. L. et al. Genetic variation in the renin-angiotensin-aldosterone system is associated with cardiovascular risk factors and early mortality in established coronary heart disease. J Hum Hypertens. 27, 237–44 (2013).
Jia, E. Z. et al. Renin-angiotensin-aldosterone system gene polymorphisms and coronary artery disease: detection of gene-gene and gene-environment interactions. Cell Physiol Biochem. 29, 443–52 (2012).
Fukui, K., Yamada, H. & Matsubara, H. Pathophysiological role of tissue renin-angiotensin-aldosterone system (RAAS) in human atherosclerosis. Nihon Rinsho. 70, 1556–1561 (2012).
Muhlestein, J. B. et al. Relation of elevated plasma renin activity at baseline to cardiac events in patients with angiographically proven coronary artery disease. Am J Cardiol. 106, 764–769 (2010).
Gonzalez, M. C., Cohen, H. W., Sealey, J. E., Laragh, J. H. & Alderman, M. H. Enduring direct association of baseline plasma renin activity with all-cause and cardiovascular mortality in hypertensive patients. Am J Hypertens. 24, 1181–1186 (2011).
Tomaschitz, A. et al. Associations of plasma renin with 10-year cardiovascular mortality, sudden cardiac death and death due to heart failure. Eur Heart J. 32, 2642–2649 (2011).
Hillaert, M. A. et al. Aldosterone, atherosclerosis and vascular events in patients with stable coronary artery disease. Int J Cardiol. [Epub ahead of print] (2012).
Franco, E. et al. Renin-angiotensin-aldosterone system polymorphisms: a role or a hole in occurrence and long-term prognosis of acute myocardial infarction at young age. BMC Med Genet. 22, 27 (2007).
Patel, B. M. & Mehta, A. A. Aldosterone and angiotensin: Role in diabetes and cardiovascular diseases. Eur J Pharmacol. [Epub ahead of print] (2012).
Jia, E. Z. et al. Relationship between leukocyte count and angiographical characteristics of coronary atherosclerosis. Acta Pharmacol Sin. 26, 1057–1062 (2005).
Judkins, M. P. A percutaneous transfemoral technique. Radiology. 89, 815–821 (1967).
Gensini, G. G. A more meaningful scoring system for determinating the severity of coronary heart disease. Am J Cardiol. 51, 606 (1983).
Nasiri, H., Forouzandeh, M., Rasaee, M. J. & Rahbarizadeh, F. Modified salting-out method: high-yield, high-quality genomic DNA extraction from whole blood using laundry detergent. J Clin Lab Anal. 19, 229–232 (2005).
Lahiri, D. K., Bye, S., Nurnberger, J. I., Jr, Hodes, M. E. & Crisp, M. A non-organic and nonenzymatic extraction method gives higher yields of genomic DNA from whole-blood samples than do nine other methods tested. J Biochem Biophys Methods. 25, 193–205 (1992).
Lynch, A. I. et al. Gene panels to help identify subgroups at high and low risk of coronary heart disease among those randomized to antihypertensive treatment: the GenHAT study. Pharmacogenet Genomics. 22, 355–66 (2012).
Zhang, K., Zhou, B. & Zhang, L. Association study of angiotensin II type 1 receptor: A1166C (rs5186) polymorphism with coronary heart disease using systematic meta-analysis. J Renin Angiotensin Aldosterone Syst. 14, 181–8 (2013).
Martínez-Rodríguez, N. et al. Association of angiotensin II type 1-receptor gene polymorphisms with the risk of developing hypertension in Mexican individuals. J Renin Angiotensin Aldosterone Syst. 13, 133–40 (2012).
Wu, C. K. et al. A propensity score-based case-control study of renin-angiotensin system gene polymorphisms and diastolic heart failure. Atherosclerosis. 205, 497–502 (2009).
Mishra, A., Srivastava, A., Mittal, T., Garg, N. & Mittal, B. Impact of renin-angiotensin-aldosterone system gene polymorphisms on left ventricular dysfunction in coronary artery disease patients. Dis Markers. 32, 33–41 (2012).
Hsieh, F. Y. & Lavori, P. W. Sample-Size Calculations for the Cox Proportional Hazards Regression Model with Nonbinary Covariate. Controlled Clinical Trials. 21, 552–560 (2000).
Schoenfeld David, A. Sample-Size Formula for the Proportional-Hazards Regression Mode. Biometrics. 39, 499–503 (1983).
Acknowledgements
Supported by the National Natural Science Foundation of China, No. 30400173 and 30971257. A project funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions.
Author information
Authors and Affiliations
Contributions
J.E. and L.L. wrote the main manuscript text; G.C., G.Y., C.Z., A.F., L.L., L.Z. and L.Z. performed the experiment; W.L., L.C., K.X., M.W., Z.T. and Y.Z. done the data collected. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. The images in this article are included in the article's Creative Commons license, unless indicated otherwise in the image credit; if the image is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the image. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Jia, EZ., Chen, ZH., An, FH. et al. Relationship of renin-angiotensin-aldosterone system polymorphisms and phenotypes to mortality in Chinese coronary atherosclerosis patients. Sci Rep 4, 4600 (2014). https://doi.org/10.1038/srep04600
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep04600
This article is cited by
-
Influence of microvascular dysfunction on regional myocardial deformation post-acute myocardial infarction: insights from a novel angiographic index for assessing myocardial tissue-level reperfusion
The International Journal of Cardiovascular Imaging (2016)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.