Abstract
Study design:
Clinical controlled trial.
Objectives:
To evaluate the effectiveness of an occupational therapy (OT) program combined with neuromotor rehabilitation, by assessing the degree of functional independence reached by patients with spinal cord injuries at first hospitalization.
Settings:
Subjects selected from the Spinal Cord Unit of the Rehabilitation Institute of Montecatone (Imola, Italy).
Participants:
Thirty-six male patients below age 60, with complete paraplegia (ASIA-A) in thoracic-lumbar level, at first hospitalization.
Methods:
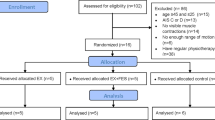
Patients were divided into experimental and control groups. Subjects in the experimental group underwent neuromotor rehabilitation coupled with an OT program, whereas those in the control group followed neuromotor rehabilitation only. Increase in functional independence at discharge was evaluated by the Valutazione Funzionale Mielolesi (VFM) assessment scale.
Results:
Patients in the experimental group showed a significant increase in the total VFM score, and in domains concerning transfers and wheelchair use. A significant improvement was observed in unmarried patients as compared to married ones.
Conclusion:
An OT service within a Spinal Cord Unit allows us to achieve a higher level of functional independence.
Similar content being viewed by others
Introduction
Occupational therapy (OT) is skilled treatment that helps individuals achieve independence in all facets of their lives. OT assists people in developing the ‘skills for the job of living’ necessary for independent and satisfying lives.1 The role of OT in spinal cord injury (SCI) rehabilitation comprises the adaptation of social, living and other kinds of environment for the disabled2 and to assist the client in regaining abilities and roles that are important and meaningful,3 whereas individual aims are specific and related to a certain patient.2 A major consequence of spinal injury disability is a general reduction in personal independence and social participation. The International Classification of Functioning, Disability and Health (ICF) defines activity limitations as the difficulties an individual affected by SCI may encounter in executing tasks such as washing the upper body, walking or using a wheelchair.4 As reported in the literature, individuals with activity limitations experience participation restrictions in daily life.5, 6, 7, 8, 9 In the ICF, participation is defined as ‘involvement in life situations’, including, for example, work and school, housekeeping, social relationships and involvement with community organizations. Participation restrictions are the problems an individual may have involving life situations.4 The patient with SCI may become discouraged with his/her therapy when observable gains are few and far between. Thus, a variety of purposeful activities are also used and modified to promote self-esteem by highlighting functional skills and emphasizing the tangible development of a client's physical, social, emotional, sensory and cognitive abilities.10 OT's unique contribution to occupational performance lies in its use of purposeful activities to promote psychological and physical health and maximum functional independence.11 As a part of complex rehabilitation, it is applied in solving the problems of occupation (self-care, work and leisure) of patients.12 It is emphasized that early OT, started immediately after stabilization of patient's functional state, is of great importance.13 The purpose of OT in early treatment of SCI is to evaluate a person's ability and level of functioning in his/her home, at work, and while engaging in leisure activities and hobbies; to provide individualized therapy to retrain people to perform daily living skills using adaptative techniques; to facilitate coping skills that could help a person overcome the effects of SCI; to implement exercises and routines that strengthen muscles that may have been affected and are necessary in daily activities; to determine the type of assistive devices that could help a person become more independent with daily living skills.1 To our knowledge, the literature contains no randomized controlled trials evaluating the effectiveness of an OT unit for patients with SCI. Moreover, although OT is standard therapy for the rehabilitation of SCI patients in many countries, publications on this topic are still few. The aim of this study is to evaluate the effectiveness of an OT program coupled with neuromotor rehabilitation, by assessing the level of functional independence reached by patients with SCI at first hospitalization.
Materials and methods
Settings and Subjects
This study was conducted in 2004–2006 in the Spinal Cord Unit of the Rehabilitation Institute of Montecatone (Imola, Italy). The study population consisted of 36 male subjects below age 60, with complete paraplegia (ASIA-A) in thoracic-lumbar level, at first hospitalization. Prerequisites for inclusion in the study were in a sitting position for at least 3 h, resolved spinal shock and/or stable clinic conditions; cooperating patient. After admission in the Spinal Cord Unit, all the patients received early neuromotor rehabilitation by the rehabilitative team. The neuromotor rehabilitation program included reflexes inhibiting postures, mobilizations and ‘proprioceptive neuromuscular facilitation’,14 exercises of the trunk and lower limbs. The basic principles of this approach are stretch reflex as a starter of movement, proprioceptive scheme with diagonal and spiral patterns and verbal command by the physical therapist during the range of motion. All the physical therapists involved in the trial were experts in this rehabilitative methodology. Five weeks before discharge, the study population was divided into two groups. The experimental group was composed of 24 patients, and underwent neuromotor rehabilitation coupled with a series of OT sessions. The 12 patients of the control group, after being offered to follow an integrated program, freely chose to continue only with neuromotor rehabilitation under the supervision of their physical therapists. Among possible reasons for this choice were the difficulty in beginning a therapeutic relationship with a new health professional, the need to move to a different environment in which to perform activities different from the usual ones and a lack of awareness of the intervention effectiveness, or rather, a greater consideration attributed by these patients to neuromotor rehabilitation with their physical therapist. The weekly rehabilitation program for the experimental group included eight neuromotor rehabilitation sessions and two OT sessions, whereas the control group program consisted of 10 neuromotor rehabilitation sessions. Both neuromotor and OT sessions had a duration of 60 min and took place twice a day, 5 days a week. OT sessions were carried out in dedicated rooms under the supervision of occupational therapists specifically trained in SCI rehabilitation. The OT rooms are to a large extent inspired by the structure of a standard flat with kitchen, bedroom and bathroom. To solve each patient's access problems, the kitchen is designed so that the elements can be modified and arranged in different positions depending on the user's needs. The worktop is suspended and can be adjusted at the desired height to allow wheelchair access. Wall units, normally installed at 45/50 cm from the worktop surface and adjustable in height, are equipped with shelving that can be manually lowered, making objects, even those on the top shelves, accessible. The bedroom is wide and furnished with a 60-cm high double bed used for training in transfers from and to wheelchair. The bathroom consists of wall mount basin with a 80 cm front space to allow front access, WC installed at about 50 cm from the floor, fixed wall bars and sufficient side space to allow wheelchair transfer, wheel-in shower with fold-down seat and bathtub with seat.15 The OT setting also includes an equipped area in which patients are trained to daily activities and to wheelchair independence (for example techniques for getting from wheelchair to floor and vice versa and for climbing a step). Finally, the OT program includes a specific training for transfers from wheelchair to car and training on effective strategies to stow the wheelchair in the vehicle's interior.
Procedure
The degree of functional independence was assessed for the two groups both at admission in the study and at discharge by the Valutazione Funzionale Mielolesi (VFM) scale. VFM is a validated scale that can be used confidently in the rehabilitation setting for patients with SCI to screen for functional problems and monitor changes in patient's functional status and impact of rehabilitation. VFM's main potential use is to monitor individual patients over time, document changes and assess treatment effectiveness.16 The VFM is divided into nine domains, each including a number of tasks: bed mobility (5 tasks), eating (6 tasks), transfers (12 tasks), wheelchair use (15 tasks), grooming/bathing (7 tasks), dressing (8 tasks), social skill (9 tasks), standing (4 tasks) and walking (8 tasks). After direct observation of patient's performance, each task is assigned a score ranging from 0 to 4, where 0 indicates complete dependence and 4 indicates complete independence. Standing and walking domains were not considered, because they were not included in the rehabilitative targets of this phase. Because all the participants examined were paraplegic, values concerning the eating domain were not included, reaching the highest score both at admission and at discharge. VFM was administered by two non-resident physical therapists, expert in OT. During data analysis, we considered the difference between discharge and admission scores for each domain from 1 to 7 and for the total sum score of domains from 1 to 7.
Statistical Analysis
Continuous data were expressed as mean±SD. A skewness-kurtosis test was used to test the normal distribution of values. In cases of normal distribution, continuous variables were tested with Student's t-test, otherwise a two-sample Wilcoxon rank-sum test was used. Categorical variables were assessed using the χ2 test. To evaluate the effectiveness of OT, a multiple linear regression model was performed. A comparison of total VFM score was performed between married and unmarried patients and between the two groups (that is treated and untreated) by using one-way analysis of variance with Scheffé multiple comparison test. The level of significance was set at P<0.05. Stata 8.0 SE software (Stata Corporation, Texas, TX, USA) was used for all analyses.
Results
Experimental and control groups were comparable both for region of residence, profession, marital status and age, and for days of hospitalization (Table 1). In particular, subjects' mean age was 32 (experimental group, 31.96; control group, 32.5) and the mean number of days of hospitalization was 167 (experimental group, 174.96; control group, 158.42). Table 2 compares the outcomes of VFM assessment at admission in the study and at discharge in the two groups, with respect to total VFM score and to single domain scores. A statistically significant increase was found for total score (P=0.007), transfers score (P<0.0001) and wheelchair use score (P=0.005) in the experimental group as compared to controls. An increase was found, albeit not statistically significant, in the experimental group, for domains concerning grooming/bathing (P=0.071) and social skill (P=0.089). Table 3 reports results of multiple regression analysis performed on patients of both groups. Patients in the experimental group showed a significant improvement, also considering age, marital status, job title, days of hospitalization and area of residence. In particular, the increase in the total score was statistically significant for unmarried patients with respect to married ones (P=0.026). Notably, the increase for unmarried patients in the experimental group (53.07±16.18) and for married patients in the control group (11.75±12.87) resulted statistically significant (Scheffé test, P<0.005).
Discussion
Our results point to the importance of an OT program associated with neuromotor rehabilitation, as opposed to neuromotor rehabilitation alone in increasing independence in patients with SCI in thoracic-lumbar level. We obtained a statistically significant increase in functional independence, assessed by the VFM scale, both for the total score and for the scores concerning transfers and wheelchair use (Table 2). These results could be due to the fact that patients immediately understand the relevance of these functions in reaching higher independence and a full social participation; it should be then taken into consideration that most activities carried out in the OT service are specifically aimed at training in wheelchair use and transfers. Similar results were obtained by Mingaila and Krisciunas12 in a study to assess the effectiveness of OT dependent on the level and completeness of SCI. The greatest improvements, evaluated by Functional Independence Measure (FIM), were obtained in case of complete SCI (ASIA-A) in thoracic-lumbar level, in using wheelchair and in transfers from bed to wheelchair. In our study, we also found that the increase in functional independence at discharge was higher in unmarried patients than in married ones, irrespective of age (Table 3). A possible explanation for our findings could be the low mean age of subjects (experimental group, 31.96±8.29; control group, 32.50±12.58), presumably related to a short marriage experience. In some of these cases, the young and strongly motivated spouse might take her husband's activities upon herself, thus preventing him from training and consequently from increasing functional independence. This might also indirectly result in a reduced motivation to intensely activate neuromuscular resources and in delegating part or all of the activities connected with functional independence. To our knowledge, only one study has previously evaluated functional independence and quality of life achieved after first hospitalization in relation to marital status demonstrating that, in the long run, independence and satisfaction are positively influenced by marriage.17 Quantitative research among people with all levels of SCI has then demonstrated positive correlations between marital status and quality of life/life satisfaction.18, 19, 20 On the basis of the above-mentioned elements, the following scenario could be hypothesized for married patients with SCI: although during first hospitalization the presence of the partner could be a limiting factor in the recovery of functional independence, in the long run it appears to positively affect quality of life and, as a consequence, independence itself. One limiting factor of our study is the lack of randomization of the two groups of patients; moreover, during first hospitalization, the presence of a partner adds to nurses' intervention, making it difficult to correlate patients' marital status with the level of functional independence achieved at discharge. Nevertheless, the statistical significance of results concerning this variable suggests the opportunity to further investigate the role of marriage partners as part of initial rehabilitation.
Conclusion
Although our study included only two weekly OT sessions and is therefore to be considered a ‘pilot study’, our results showed that the presence of an OT service within a Spinal Cord Unit allows paraplegic patients to reach a higher degree of independence. Notably, the results obtained showed that increase in functional independence was higher in unmarried patients than in married ones. On the basis of these data, we assume that the presence of a partner may be a limiting factor in the patient's functional rehabilitation during first hospitalization. Finally, we think the trial should be repeated including a higher number of OT sessions and extended to tetraplegic patients and paraplegics with incomplete injuries (ASIA-B/C/D). Furthermore, another interesting aspect deserving further investigation is the relationship between increase in functional independence and factors such as return to work, independent living and fitness.
References
American Occupational Therapy Association. www.aota.org.
Bjorklund A . Focus on occupational therapists' paradigms. Scand J Caring Sci 1999; 13: 165–170.
Lee B, Nantais T . Use of electronic music as an occupational therapy modality in spinal cord injury rehabilitation: an occupational performance model. Am J Occup Ther 1996; 50: 362–369.
WHO. International Classification of Functioning, Disability and Health. World Health Organization: Geneva, 2001.
Blake K . The social isolation of young men with quadriplegia. Rehabil Nurs 1995; 20: 17–22.
Pentland W, Harvey AS, Smith T, Walker J . The impact of spinal cord injury on men's time use. Spinal Cord 1999; 37: 786–792.
Law M . Participation in the occupations of everyday life. Am J Occup Ther 2002; 56: 640–649.
Hart KA, Rintala DH . Long-term outcomes following spinal cord injury. NeuroRehabilitation 1995; 5: 57–73.
Noreau L, Shephard RJ . Spinal cord injury, exercise and quality of life. Sports Med 1995; 20: 226–250.
MacRae A . Should music be used therapeutically in occupational therapy? Am J Occup Ther 1992; 46: 275–277.
Department of National Health and Welfare and the Canadian Association of Occupational Therapists. Guidelines for the client-centred practice of occupational therapy (H39–33/1983E). Department of National Health and Welfare: Ottawa, ON, 1983.
Mingaila S, Krisciunas A . Occupational therapy for patients with spinal cord injury in early rehabilitation. Medicina (Kaunas) 2005; 41: 649–654.
Outcomes Following Traumatic Spinal Cord Injury: Clinical Practice Guidelines for Health-Care Professionals. Consortium for Spinal Cord Medicine Clinical Practice Guidelines. Paralyzed Veterans of America: Washington, DC, 1999.
Voss DE . Introduction. In: Voss DE, Ionta MK, Myers BJ (eds), Proprioceptive Neuromuscular Facilitation. 3rd edn Harper & Row, Publishers: Philadelphia, 1985, pp XIII–XXI.
Vannini R . La Terapia Occupazionale. In: Bonavita J, Menarini M, Pillastrini P (ed), La Riabilitazione nelle Mielolesioni. Masson: Milano, 2004, pp 325–352.
Taricco M, Apolone G, Colombo C, Filardo G, Telaro E, Liberati A . Functional status in patients with spinal cord injury: a new standardized measurement scale. Arch Phys Med Rehab 2000; 81: 1173–1180.
McColl MA, Stirling P, Walker J, Corey P, Wilkins R . Expectations of independence and life satisfaction among ageing spinal cord injured adults. Disabil Rehabil 1999; 21: 231–240.
Dijkers M . Correlates of life satisfaction among persons with spinal cord injury. Arch Phys Med Rehabil 1999; 80: 867–876.
Lin K-H, Chuang C-C, Kao M-J, Tsauo J-Y . Quality of life of spinal cord injured patients in Taiwan: a subgroup study. Spinal Cord 1997; 35: 841–849.
Anderson CJ, Vogel LC . Domain-specific satisfaction in adults with pediatric-onset spinal cord injuries. Spinal Cord 2003; 41: 684–691.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pillastrini, P., Mugnai, R., Bonfiglioli, R. et al. Evaluation of an occupational therapy program for patients with spinal cord injury. Spinal Cord 46, 78–81 (2008). https://doi.org/10.1038/sj.sc.3102072
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102072