Abstract
Study design:
Case-controlled preliminary observational study.
Objective:
Melatonin is usually secreted only at night and may influence sleep. We previously found that complete cervical spinal cord injury (SCI) interrupts the neural pathway required for melatonin secretion. Thus, we investigated whether the absence of night time melatonin in cervical SCI leads to sleep disturbances.
Setting:
General Clinical Research Center, Brigham & Women's Hospital, Boston, USA.
Methods:
In an ancillary analysis of data collected in a prior study, we assessed the sleep patterns of three subjects with cervical SCI plus absence of nocturnal melatonin (SCI levels: C4A, C6A, C6/7A) and two control patients with thoracic SCI plus normal melatonin rhythms (SCI levels: T4A, T5A). We also compared those results to the sleep patterns of 10 healthy control subjects.
Results:
The subjects with cervical SCI had significantly lower sleep efficiency (median 83%) than the control subjects with thoracic SCI (93%). The sleep efficiency of subjects with thoracic SCI was not different from that of healthy control subjects (94%). There was no difference in the proportion of the different sleep stages, although there was a significantly increased REM-onset latency in subjects with cervical SCI (220 min) as compared to subjects with thoracic SCI (34 min). The diminished sleep in cervical SCI was not associated with sleep apnea or medication use.
Conclusion:
We found that cervical SCI is associated with decreased sleep quality. A larger study is required to confirm these findings. If confirmed, the absence of night time melatonin in cervical SCI may help explain their sleep disturbances, raising the possibility that melatonin replacement therapy could help normalize sleep in this group.
Sponsorship:
This work was supported by the NIH (GCRC Grant M01-RR-02635 and Grant HL-64815). Dr Ayas is supported by the BCLA, CIHR, and MSFHR.
Similar content being viewed by others
Introduction
Patients with cervical spinal cord injury (SCI) commonly have excessive daytime sleepiness and disturbed sleep, including reduced REM sleep, which cannot be explained solely by disruptions in breathing during sleep.1, 2, 3 We previously found that patients with complete lesions of their cervical spinal cords have an absence of the normal endogenous melatonin secretion at night. This demonstrates that the neural pathway for the endogenous production of melatonin passes through the cervical spinal cord.4 Since exogenous melatonin can shorten sleep onset, improve sleep maintenance, and increase REM sleep,5, 6, 7 we hypothesized that the absence of endogenous night time melatonin in subjects with cervical SCI would lead to prolonged sleep onset latency, reduced sleep efficiency, and reduced REM sleep.
Methods
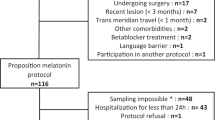
In an ancillary analysis of the data set collected in a prior study,4 we compared the sleep patterns of three subjects with neurologically complete (Frankel A) cervical SCI and absence of night time melatonin with the sleep patterns of two control groups with conserved night time melatonin: two patients with neurologically complete (Frankel A) thoracic SCI and 10 healthy controls without SCI (Table 1). The five SCI subjects were male, nonobese, had a mean age of 32 years (range 27–42), and had chronic SCI for an average of 7.7 years (range 4.7–18.5). These SCI subjects were otherwise healthy as established by medical history and physical and psychological examination. Furthermore, all SCI subjects had evidence of normal hypothalamic circadian function.4 Of the 10 healthy control subjects, eight were male and their mean age was 28 years (20–44).
All subjects gave written informed consent and the protocol was approved by local Human Research Committee. During the week prior to the study, all subjects maintained a regular 8-h sleep schedule as verified by self-report and wrist actigraphy (Actiwatch, Minimitter, Bend, OR, USA). Except as noted in Table 1, all subjects were free of medication, and of caffeine, nicotine, and alcohol for the week prior and at the time of study. Subjects were admitted to an individual suite in a sleep laboratory approximately 8 h before the sleep recording to aid relaxation and adjustment to the laboratory equipment and environment. Rooms were free of time cues and illuminated with ordinary room light (∼150 lux). Subjects went to bed at their usual time and were scheduled for 8 h in darkness (<1 lux). Sleep patterns, breathing, and leg movements were assessed using standard clinical polysomnography incorporating electroencephalography, electro-oculography, submental electromyography, electrocardiography, nasal/oral airflow (thermistor), snoring (throat microphone), thoracic and abdominal breathing motion (inductance plethysmography), arterial oxygen saturation (pulse oximetry), and leg movements (anterior tibialis EMG on both legs). Sleep stages were scored in 30-s epochs, according to standard criteria,8 with scorers blinded to condition. Respiratory events were scored using the American Academy of Sleep Medicine Task Force criteria.9 Sleep efficiency was calculated as the total duration of sleep divided by the time between first sleep onset and last awakening.
Mann–Whitney U tests were used to test all hypotheses (two-tailed tests, or one-tailed tests for a priori hypotheses stated above, as appropriate). We considered a P-value <0.05 as significant. The planned comparisons were between cervical SCI and thoracic SCI (any differences attributable to melatonin) and between thoracic SCI and healthy controls (any differences attributable to SCI).
Results
As previously reported in these subjects, melatonin was absent in cervical SCI, whereas subjects with thoracic SCI had conserved melatonin rhythms (Figure 1).4 Total sleep duration and sleep efficiency were significantly lower in subjects with cervical SCI (median 390 (IQR 388–394) min and 83 (83–86)%, respectively) compared to subjects with thoracic SCI (428 (419–437) min and 93 (92–94)%; P=0.04 and 0.04), but did not differ between subjects with thoracic SCI and healthy controls (422 (402–443) min and 94 (92–96)%) (Figure 1). The sleep efficiencies translate into more than a doubling of the duration of wakefulness after sleep onset in patients with cervical SCI (81 (66–81) min) when compared to both patients with thoracic SCI (33 (28–39) min) and healthy controls (28 (19–38) min). REM sleep latency was also prolonged in subjects with cervical SCI (220 (162–277) min) compared to subjects with thoracic SCI (34 (25–43) min; P=0.04) (Figure 1). REM sleep latency in patients with thoracic SCI was not significantly different from that in healthy controls (88 (68–120) min). There were no statistical differences in sleep onset latency or proportions of the different sleep stages between groups. None of the SCI subjects had any periodic limb movements during sleep. One subject in each SCI group had mild sleep apnea (AHI between 10 and 20: Table 1).
The 24 h average melatonin plasma concentration and sleep variables compared between healthy controls, patients with thoracic SCI and a clear night time melatonin surge, and patients with cervical SCI and no night time melatonin surge. For the healthy controls (C), the box indicates the IQR and the horizontal line within the box indicates the median. Subject codes are indicated for cross-reference4
Conclusion
The results of the present study indicate that compromised sleep in patients with cervical SCI may in part be due to the complete absence of the nocturnal melatonin surge. Importantly, in the patients with a thoracic SCI who were otherwise healthy, sleep efficiency was not different from that in healthy controls. Daytime melatonin administration at physiological dosages increases sleep propensity.10 Furthermore, acute suppression of the night time melatonin surge – either by light or beta-blockers – compromises sleep quality, which can be reversed by melatonin supplementation.5, 6 However, whether the chronic absence of night time melatonin secretion leads to compromised sleep is unclear. The results of the present study suggest that the absence of night time melatonin secretion results in chronically reduced sleep quality. Thus, the absence of night time melatonin secretion may explain part of the excessive daytime sleepiness and disturbed sleep observed in patients with cervical SCI.1, 2, 3 Furthermore, the increased latency to REM sleep in subjects with cervical SCI suggests that the absence of night time melatonin may partially underlie the previously observed reduction in REM sleep propensity.2 Melatonin has been proposed to facilitate sleep by inhibiting the circadian drive for waking that emanates from the SCN,11, 12, 13 by binding to the high-affinity melatonin receptors in the human SCN14 (for a review, see Scheer et al7). Also, sleep propensity, sleepiness, and REM sleep expression are mainly under circadian control.15 Whether the sleep-promoting effect of melatonin is related to its effects directly on the circadian pacemaker is not known. Alternatively or additionally melatonin might have a sleep-promoting effect by increasing peripheral skin temperature and/or decreasing core temperature, changes known to be involved in the sleep/wake rhythm.5, 16
While we studied a small number of SCI subjects, this SCI group was otherwise healthy, had documented complete absence of endogenous melatonin (cervical SCI), had documented normal hypothalamic endogenous circadian rhythmicity (all SCI subjects, as detected by profiles of cortisol and thyroid stimulating hormone4), and underwent sleep recordings under standardized laboratory conditions at each individual's habitual sleep time. These points plus the fact that the limited medication use in this group, including valium in two cervical SCI subjects (Table 1), ought to have biased towards the null hypothesis, suggest that the findings of poor sleep in the cervical SCI group are robust. However, a larger study is required to confirm or refute the findings.
If the results of the present study are confirmed, this would suggest that sleep disturbances of patients with cervical SCI may be related to the absence of night time melatonin. These results would suggest a role of endogenous melatonin in normal sleep maintenance in humans. Furthermore, these data would imply that melatonin supplementation might help restore normal sleep in patients with cervical SCI.
References
Adey WR, Bors E, Porter RW . EEG sleep patterns after high cervical lesions in man. Arch Neurol 1968; 19: 377–383.
McEvoy RD et al. Sleep apnoea in patients with quadriplegia. Thorax 1995; 50: 613–619.
Biering-Sorensen F, Biering-Sorensen M . Sleep disturances in the spinal cord injured: an epidemiological questionnaire investigation, including a normal population. Spinal Cord 2001; 39: 505–513.
Zeitzer JM, Ayas NT, Shea SA, Brown R, Czeisler CA . Absence of detectable melatonin, preservation of cortisol, thyrotropin rhythms in tetraplegia. J Clin Endocrinol Metab 2000; 85: 2189–2196.
VanDen Heuvel CJ, Reid KJ, Dawson D . Effect of atenolol on nocturnal sleep and temperature in young men: reversal by pharmacological doses of melatonin. Physiol Behav 1997; 61: 795–802.
Cajochen C, Kräuchi K, Danilenko KV, Wirz-Justice A . Evening adminstration of melatonin and bright light: interactions on the EEG during sleep and wakefulness. J Sleep Res 1998; 7: 145–157.
Scheer FA, Cajochen C, Turek FW, Czeisler CA . Melatonin in the regulation of sleep and circadian rhythms. In: Kryger MH, Roth T, Dement WC (eds). Principles and Practice of Sleep Medicine. 4th edn. WB Saunders: Philadelphia 2005, pp 395–404.
Rechtschaffen A, Kales A . A Manual of Standardized Terminology, Techniques and Scoring System for Sleep Stages of Human Subjects. US Government Printing Office: Washington, DC 1968.
Flemons WW et al. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The report of an American Academy of Sleep Medicine task force. Sleep 1999; 22: 667–689.
Zhdanova lV, Wurtman RJ, Morabito C, Piotrovska VR, Lynch HJ . Effects of low oral doses of melatonin, given 2–4 h before habitual bedtime, on sleep in normal young humans. Sleep 1996; 19: 423–431.
Lavie P . Melatonin: Role in gating nocturnal rise in sleep propensity. J Biol Rhythms 1997; 12: 657–665.
Sack RL, Hughes RJ, Edgar DM, Lewy AJ . Sleep-promoting effects of melatonin: at what dose, in whom, under what conditions, and by what mechanisms? Sleep 1997; 20: 908–915.
Barinaga M . How jet-lag hormone does double duty in the brain. Science 1998; 277: 480.
Reppert SM, Weaver DR, Rivkees SA, Stopa EG . Putative melatonin receptors in a human biological clock. Science 1988; 242: 78–81.
Dijk DJ, Czeisler CA . Contribution of the circadian pacemaker and the sleep homeostat to sleep propensity, sleep structure, electroencephalographic slow waves, and sleep spindle activity in humans. J Neurosci 1995; 15: 3526–3538.
Kräuchi K, Cajochen C, Wirz-Justice A . A relationship between heat loss and sleepiness: effects of postural change and melatonin administration. J Appl Physiol 1997; 83: 134–139.
Acknowledgements
FAJL Scheer did the data analysis and prepared the draft manuscript. JM Zeitzer contributed to the experimental design and conduct of the study, and edited the manuscript. NT Ayas participated in the design of the study and data collection, and edited the manuscript. R Brown participated in the design of the study and edited the manuscript. CA Czeisler participated in the design of the study. SA Shea contributed to experimental design, data analysis, and edited the manuscript. The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, writing of the report, or decision to submit the paper for publication. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Author information
Authors and Affiliations
Additional information
Conflict of interest: We declare that we have no conflict of interest.
Rights and permissions
About this article
Cite this article
Scheer, F., Zeitzer, J., Ayas, N. et al. Reduced sleep efficiency in cervical spinal cord injury; association with abolished night time melatonin secretion. Spinal Cord 44, 78–81 (2006). https://doi.org/10.1038/sj.sc.3101784
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101784
Keywords
This article is cited by
-
Melatonin secretion and sleep disorders in patients with spinal cord injuries
Spinal Cord (2024)
-
Sleep apnea and unilateral upper and lower extremity allodynia as a result of a large thoracic disc herniation: a case report
Sleep Science and Practice (2021)
-
Circadian and state-dependent core body temperature in people with spinal cord injury
Spinal Cord (2021)
-
Efficacy of melatonin for sleep disturbance following traumatic brain injury: a randomised controlled trial
BMC Medicine (2018)
-
Normalization of disrupted clock gene expression in males with tetraplegia: a crossover randomized placebo-controlled trial of melatonin supplementation
Spinal Cord (2018)