Abstract
Objective: To investigate the pathogenesis of the rare radiogenic lower motor neurone disease (LMND) on the basis of a meta-analysis of the published case histories.
Materials and methods: The authors reviewed 47 well-documented radiogenic LMND cases from the English literature.
Results: The disease typically occurs following the irradiation of radiosensitive cancers situated near the spinal cord. It arises predominantly (46 cases) in the lower extremities; only one case involved the upper extremities. There is a male predominance (male:female ratio 7.8:1), and the patients are characteristically young (13–40 years, with four exceptions). An overdose does not seem to be a particular risk factor for the development of the disease, as total dose, fraction size and biologically effective dose are typically below 50 Gy, 2 Gy and 128 Gy2, respectively, which are regarded as safe doses. Other risk factors (chemotherapy, operations, etc) have been identifed only rarely. Radiogenic LMND is manifested in an apparently random manner, 4–312 (mean 48.7) months after the completion of radiotherapy.
Discussion: The complete lack of a dose–effect relationship argues strongly against a pure radiogenic nature of the pathological process. The latency period is typically several years and it varies extremely, which excludes a direct and complete causal relationship between radiotherapy and LMND. As the interaction of ionizing radiation with living tissues is highly unspecific, thus a selective motor injury due to irradiation alone, without comparable effects on the sensory and vegetative fibers, seems improbable.
Conclusions: On analogy with the viral motor neurone diseases, we suppose that radiogenic LMND may be preceded by viral (enterovirus/poliovirus) infection. Based on the meta-analysis, it is suggested that irradiation may be only a single component of the set of factors jointly resulting in the clinical state regarded as radiogenic LMND.
Similar content being viewed by others
Introduction
Radiation myelopathy is a rare complication of radiotherapy that may affect both the white and the gray matter.1,2,3,4,5,6,7 The clinical picture of the less frequently documented gray matter injury comprises radiogenic lower motor neurone disease (LMND), that is, flaccid paresis due to damage to the motor neurones situated in the anterior horn of the spinal cord. It may also accompany a predominant radiogenic white matter injury (demyelinization and/or ischemic vascular injury) with spastic motor, sensory and vegetative losses. In these cases, the gray matter injuries are manifested primarily in the arms.1,2,3,4,8,9 In most cases of radiogenic LMND, however, the only clinical sign of the radiation injury10,11,12,13,14,15,16,17,18,19,20, 21,22,23,24,25,26,27,28,29 is the flaccid paresis. The disease involves basically the legs, exhibiting a chronic, progressive and irreversible clinical course.
Materials and methods
The authors reviewed English literature data on the rare LMND. To exclude cases other than exclusively flaccid paresis, a complete neurological case history was a prerequisite for inclusion: only 47 such well-documented radiogenic LMND cases (Table 1) were found.10,11,12,13,14,15,16,17,18,19,20, 21,22,23,24,25,26,27,28,29 Successive publications often included previous case reports; accordingly, only the latest publications are listed.
Results
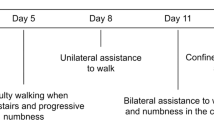
Radiogenic LMND (Table 1) typically occurs following the irradiation of radiosensitive cancers situated near the spinal cord (eg testicular cancers or malignant lymphomas). It arises predominantly (46 cases) in the lower extremities; only one case29 involved the upper extremities. There is a male predominance (male:female ratio 7.8:1), and the patients are characteristically young (13–40 years, with four exceptions). An overdose does not seem to be a particular risk factor for the development of the disease, and other risk factors (chemotherapy, operations, etc) have been identifed only rarely. Radiogenic LMND is manifested in an apparently random manner, 4–312 (mean 48.7) months after the completion of radiotherapy.
Radiogenic LMND is considered an independent clinical entity, but many of its features are reminiscent of those of classical radiogenic myelopathy (CRM), acute viral (poliovirus, enterovirus 70 or 71, or coxsackievirus A7 or A9) or late viral LMNDs (postpolio syndrome (PPS)). PPS develops many years after acute, paralytic poliomyelitis, and presents as a new onset of weakness, fatigue, fasciculation and pain, with additional atrophy of muscle groups involved or not during the initial paralytic disease.30,31,32 The two types of radiogenic myelopathy undoubtedly have a number of common features, but at the same time an appreciably higher number of dissimilarities, as will be shown below (Table 2).
One of the most interesting peculiarities of radiogenic LMND is the surprisingly low dose involved (Table 1) as compared with those leading to CRM. A majority of the former patients were treated in a single irradiation series with the total dose, fraction size and biologically effective dose typically below 50 Gy,7 2 Gy7 and 128 Gy2,33 respectively, which are regarded as safe doses. LMND has even been observed with a total dose as low as 24 Gy.28 In the four reirradiated patients, the initial doses were 46, 36, 30 and 25 Gy, respectively, the reirradiation courses took place 2 or more years later and the cumulative doses were 80, 68.4, 55 and 55 Gy, respectively.17,20,27,28 These doses are not high in light of retreatment tolerance data on the monkey spinal cord: following an initial dose of 44 Gy and an elapsed time of 3 years, the recovery is 61–100% of the initial dose with respect to a 5% probability of the occurrence of radiation injury.34
An additional striking finding of the meta-analysis of the published data is the complete lack of a dose–effect relationship in radiogenic LMND (Table 1), in marked contrast with CRM. Radiogenic LMND seems to be the only radiation-induced phenomenon without a definite dose–effect inter-relationship. This argues strongly against a pure radiogenic nature, although irradiation definitely can promote the development of this disease.
Radiogenic LMND and the two types of virus-related LMND express exclusively motor symptoms, with flaccid paresis interpreted as a consequence of gray matter injury only (Table 2). In the four autopsied cases of radiogenic LMND,10,11,27 the characteristic pathological feature was lower motor neurone degeneration. A low extent of demyelinization in the anterior and posterior column10,27 and cauda equina10 (without consecutive clinical symptoms) was also observed. The acute and late viral LMNDs also involve injured motor neurones and subtle demyelinization,30,35 but the related autopsy did not reveal sensory neurone injuries. CRM expresses extensive demyelinization of all axon types, but neuronal sequelae seldom occur in this disease,1,2,3,6,7 which accords with the known lower radiosensitivity of the gray matter as compared with that of the white matter.1,2,3
The lack of sensory and vegetative signs in radiogenic LMND is similar to the finding in both types of viral LMND. The almost exclusive motor neurone damage requires an explanation, as the interaction of ionizing radiation with living tissues is highly unspecific, and a selective motor injury due to irradiation alone, without comparable effects on the sensory and vegetative fibers, seems improbable. Irradiation of the monkey spinal cord caused radiation-induced damage within the whole irradiated segment, as expected.34,36 No radiogenic LMND cases have been published on laboratory animals and no animal model exists for radiation-induced motor signs only.
Radiogenic LMND displays a lumbar predominance (Table 1), whereas CRM is observed mainly in a cervical and/or thoracic location,1,3,4,5,6,7,37 the latter explained by the more frequent radiotherapy indication in this location. The outlined dissimilarity suggests that factors different from the radiation dose may additionally contribute to the development of radiogenic LMND. It is worthy of interest that acute viral LMND is also characterized by a lumbar predominance, with a suggested argument that provocation by frequent and intensive muscle work plays a decisive role in the development of the disease.30 It might be speculated that this too may be a factor contributing to the typical lower extremity manifestation of radiogenic LMND.
Radiogenic LMND occurs more frequently in males (Table 1), in contrast with CRM and viral LMNDs, which display a 1:1 female:male ratio. The male dominance in radiogenic LMND relates to testicular tumor being the main indication of abdominal para-aortal irradiation. Excluding testicular cancer cases, the male/female ratio for the published cases of radiogenic LMND is 1:1 (Table 1).
The age of the patients varies appreciably but those with CRM are generally older (probably because of the increasing incidence of malignant tumors with age), whereas for radiogenic (Table 1) and viral LMNDs young and middle-aged subjects predominate. The time between irradiation and CRM onset is around 12 months (range 3–48 months).1,3,5,6,7,37 The latency period in radiogenic LMND is typically several years (mean 48.7 months), and it varies extremely (Table 1), which excludes a direct and complete causal relation between radiotherapy and LMND.
The central and peripheral motor conduction velocities (Table 2), as measured within the involved regions, may be normal in different phases of radiogenic LMNDs,11,13,15,17,19,20,21,23,25,27,28,29 acute poliomyelitis30 and PPS.38 In contrast, the central and peripheral conduction velocities are both diminished in CRM.39,40 The functional deficit in the latter disease is always assigned to the irradiated segment. In radiogenic LMND11,23,29 and PPS,31,35,38 however, special functional deficits may also develop, which relate to asymptomatic regions previously.
CRM is very different from the other three diseases in often being fatal, whereas radiogenic and viral LMNDs usually display a benign, stable character (Table 2). Steroid therapy (Table 2) is contraindicated in acute poliomyelitis,8 and ineffective in radiogenic LMND10,20,22,27 and PPS,41 but it may have a favorable effect in the acute phase of CRM.7 These findings accord with immunosuppression by the steroids (a significant handicap during an acute viral infection), and the lack of acute inflammation in radiogenic LMND10,11,27 and PPS.30,35 The three LMNDs all behave similarly in not displaying any ischemic vascular lesion10,27,30,35 (Bowen observed extensive vasculopathy in an autopsied radiogenic LMND case, but this was probably related to the widespread artherosclerosis11), whereas CRM often exhibits these pathological features.1,2,3,6,7
Discussion
Although PPS is thought to be related to the progressive dysfunction and loss of motor neurones,38 but the role of a histopathologically proven persisting virus32,42,43,44,45 or an immune-mediated phenomenon32 within the spinal cord are also possibilities. Interplay of these possible mechanisms cannot be discounted, as enterovirus/poliovirus RNA sequences have been identified by PCR in muscle biopsy42 and CSF samples42,43,44,45 from PPS patients, and immune reaction products too have been detected.32
On analogy with these assumed mechanisms, we suppose that radiogenic LMND may be preceded by viral infection. We suggest that special conditions comprising persisting enterovirus/poliovirus and additional disturbing/provocative factors may lead to the development of the disease. This suggestion may be supported by the following arguments. Similar to irradiation, chemotherapy can conduce to a clinical picture identical to that of radiogenic LMND. It has been described in Hodgkin's disease patients after chemotherapeutic regimens,27,46,47,48 and in a non-Hodgkin's lymphoma patient vaccinated with poliovirus just before chemotherapy.49
The number of publications on radiogenic LMND has been decreasing for some time, and no newly diagnosed case has been communicated for 10 years. From this aspect, the dose reduction of the para-aortal radiotherapy during the past decade, the recent substitution of irradiaton by chemotherapy or a ‘watch-and-wait’ protocol in seminoma does not seem a convincing explanation. However, it is of great significance that the incidence of acute poliomyelitis (and consequently that of PPS) has also fallen dramatically since the early 1960s (paralysis due to the wild-type poliovirus was last documented in the Western Hemisphere in 1991), and its eradication is planned by the WHO by 2005.30 A similar decreasing trend cannot be observed with CMR, which appears with low frequency, but regularly, in large-scale clinical studies on the radiotherapy of lung, head and neck or esophageal cancer. Indeed, the clinical data indicate an increasing incidence of CRM, explained by the less effective radiation protection by the bone at the higher energies of the modern photon sources than at the lower energies of the earlier widely used orthovoltage irradiation, resulting in higher radiation dose absorption by the spinal cord.4
In susceptible mice, Theiler's murine encephalomyelitis virus (TMEV) infection causes immune-mediated demyelination similar to that in human demyelinating disorders.50,51 The disease has an unusual biphasic character, with early viral replication in the neurones, followed by chronic demyelination. The virus persists within the central nervous system throughout the chronic demyelinating disease. Experimental data support the hypothesis that the specificity of the primary white matter destruction in the TMEV model depends on immune-sensitized cells. Immunosuppression with γ-irradiation renders normally resistant mice susceptible to TMEV-induced demyelination and allows increased viral replication.52 In contrast, immunosuppression of normally susceptible mice results in acute disease and a high mortality, accompanied by large-scale neurone destruction. This study indicates an important active role of the immune system in limiting the viral infection during disease induction in nonimmunosuppressed mice.
The hypothesis of the viral origin of radiogenic LMND may be consistent with the lack of proven viral infection in the related case histories, as infections may be subclinical, but they nevertheless serve as viral prehistory. PPS can also develop without clinical manifestations of preceding acute paralytic poliomyelitis53 or in individuals exposed to children with acute poliomyelitis or children who have recently received the trivalent poliovaccine.32,38 A viral hypothesis likewise accords with epidemiological observations: the first epidemic aggregation18 was detected among soldiers exhibiting case cluster formations in the worst poliomyelitis epidemic years (1945–1946) in the USA.53
The comparisons indicate the possibility that radiogenic LMND is related to a previous viral infection, as its second stage. Its manifestation is triggered by the development of immunosuppression, brought about essentially by exposure of the lower motor neurones (in which the virus persists many years after the primary stage of the infection) to ionizing radiation. Verification of this suggestion requires further clinical investigations.
References
Jellinger K, Sturm KW . Delayed radiation myelopathy in man. Report of twelve necropsy cases. J Neurol Sci 1971; 14: 389–408.
Kristensson K, Molin B, Sourander P . Delayed radiation lesions of the human spinal cord. Report of five cases. Acta Neuropathol 1967; 9: 34–44.
Palmer JJ . Radiation myelopathy. Brain 1972; 95: 109–122.
Reagan TJ, Thomas JE, Colby Jr MY . Chronic progressive radiation myelopathy. Its clinical aspects and differential diagnosis. JAMA 1968; 203: 128–132.
Schultheiss TE, Higgins EM, El-Mahdi AM . The latent period in clinical radiation myelopathy. Int J Radiat Oncol Biol Phys 1984; 10: 1109–1115.
Schultheiss TE, Stephens LC, Maor MH . Analysis of the histopathology of radiation myelopathy. Int J Radiat Oncol Biol Phys 1988; 14: 27–32.
Schultheiss TE et al. Radiation response of the central nervous system. Int J Radiat Oncol Biol Phys 1995; 31: 1093–1112.
Ésik O et al. Radiation myelopathy with partial functional recovery: PET evidence of long-term increased metabolic activity of the spinal cord. J Neurol Sci 1999; 163: 39–43.
Sanyal B et al. Radiation myelopathy. J Neurol Neurosurg Psychol 1979; 42: 413–418.
Berlit P, Schwechheimer K . Neuropathological findings in radiation myelopathy of the lumbosacral cord. Eur Neurol 1987; 27: 29–34.
Bowen J et al. The post-irradiation lower motor neuron syndrome. Neuronopathy or radiculopathy? Brain 1996; 119: 1429–1439.
de Carolis P et al. Isolated lower motoneuron involvement following radiotherapy. J Neurol Neurosurg Psychol 1986; 49: 718–719.
de Greve JLP et al. Lower motor neuron disease in a patient with Hodgkin's disease treated with radiotherapy. Clin Neurol Neurosurg 1984; 86: 43–46.
É sik O et al. A PET study on the characterization of partially reversible radiogenic lower motor neurone disease. Spinal Cord 2002; 40: 468–473.
Feistner H et al. Post-irradiation lesions of the caudal roots. Acta Neurol Scand 1989; 80: 277–281.
Friedman M . Calculated risks of radiation injury of normal tissue in the treatment of cancer of the testis. In: Proceedings of the Second National Cancer Conference, American Cancer Society, Vol. 1. New York 1954, pp 390–400.
Gállego J et al. Delayed postirradiation lower motor neuron syndrome. Ann Neurol 1986; 19: 308–309.
Greenfield MM, Stark FM . Post-irradiation neuropathy. Am J Roentgenol 1948; 60: 617–622.
Grünewald RA et al. Late onset radiation-induced motor neuron syndrome. J Neurol Neurosurg Psychol 1992; 55: 741–742.
Horowitz SL, Stewart JD . Lower motor neuron syndrome following radiotherapy. Can J Neurol Sci 1983; 10: 56–58.
Katirji MB . Delayed postirradiation focal motor neuron syndrome. Muscle Nerve 1990; 13: 1185–1186.
Kristensen O, Melgard B, Schiødt AV . Radiation myelopathy of the lumbo-sacral spinal cord. Acta Neurol Scand 1977; 56: 217–222.
Lamy C et al. Postradiation lower motor neuron syndrome presenting as monomelic amyotrophy. J Neurol Neurosurg Psychol 1991; 54: 648–649.
Maier JG et al. Radiation myelitis of the dorsolumbar spinal cord. Radiology 1969; 93: 153–160.
Sadowsky CH, Sachs Jr E, Ochoa J . Postradiation motor neuron syndrome. Arch Neurol 1976; 33: 786–787.
Schiødt AV, Kristensen O . Neurologic complications after irradiation of malignant tumors of the testis. Acta Radiol Oncol 1978; 17: 369–378.
Schold SC et al. Subacute motor neuropathy: a remote effect of lymphoma. Ann Neurol 1979; 5: 271–287.
Tallaksen CME, Jetne V, Fosså S . Postradiation lower motor neuron syndrome. A case report and brief literature review. Acta Oncol 1997; 36: 345–347.
Tan SV, Pye IF . Postradiation motor neuron syndrome of the upper cervical region – a manifestation of the combined effect of cranial irradiation and intrathecal chemotherapy? J Neurol Neurosurg Psychol 1991; 54: 469–470.
Cohen JI . Enteroviruses and reoviruses. In: Fauci et al (eds): Harrison's: Principles of Internal Medicine, 14th edn. McGraw-Hill: New York 1998, pp 1118–1123.
Halstead LS, Rossi C . Post-polio syndrome: clinical experience with 132 consecutive outpatients. In: Halstead LS, Wiechers DO (eds): Research and Clinical Aspects of Late Effects of Poliomyelitis Birth Defects, March of Dimes, White Plains, NY, Original Article Series, Vol. 23. 1987, pp 13–26.
Sharief MK, Hentges R, Ciardi M . Intrathecal immune response in patients with post-polio syndrome. N Eng J Med 1991; 325: 749–755.
Wong CS, van Dyk J, Milosevic M, Laperriere NJ . Radiation myelopathy following single courses of radiotherapy and retreatment. Int J Radiat Oncol Biol Phys 1994; 30: 575–581.
Ang KK et al. Extent and kinetics of recovery of occult spinal cord injury. Int J Radiat Oncol Biol Phys 2001; 50: 1013–1020.
Miller DC . Post-polio syndrome spinal cord pathology. Case report with immunopathology. Ann NY Acad Sci 1995; 753: 186–193.
Ang KK et al. The tolerance of primate spinal cord to reirradiation. Int J Radiat Oncol Biol Phys 1993; 25: 459–464.
Abbatucci JS et al. Radiation myelopathy of the cervical spinal cord: time, dose and volume factors. Int J Radiat Oncol Biol Phys 1978; 4: 239–248.
Campbell AMG, Williams ER, Pearce J . Late motor neuron degeneration following poliomyelitis. Neurology 1969; 19: 1101–1106.
de Scisciolo G et al. Long-term nervous system damage from radiation of the spinal cord: an electrophysiological study. J Neurol 1991; 238: 9–15.
Snooks SJ, Swash M . Motor conduction velocity in the human spinal cord: slowed conduction in multiple sclerosis and radiation myelopathy. J Neurol Neurosurg Psychol 1985; 48: 1135–1139.
Dinsmore S, Dambrosia J, Dalakas MC . A double-blind, placebo-controlled trials of high-dose prednisone for the treatment of post-poliomyelitis syndrome. Ann NY Acad Sci 1995; 753: 303–313.
Dalakas MC . Pathogenetic mechanisms of post-polio syndrome: morphological, electrophysiological, virological, and immunological correlations. Ann NY Acad Sci 1995; 753: 167–185.
Julien J et al. Postpolio syndrome: poliovirus persistence is involved in the pathogenesis. J Neurol 1999; 246: 472–476.
Leparc-Goffart I et al. Evidence of presence of poliovirus genomic sequences in cerebrospinal fluid from patients with postpolio syndrome. J Clin Microbiol 1996; 34: 2023–2026.
Muir P et al. Evidence for persistent enterovirus infection of the central nervous system in patients with previous paralytic poliomyelitis. Ann NY Acad Sci 1995; 753: 219–232.
Recine U et al. An unusually severe subacute motor neuronopathy in Hodgkin's disease. Acta Haematol 1984; 71: 135–138.
Rowland LP, Schneck SA . Neuromuscular disorders associated with malignant neoplastic disease. J Chron Dis 1963; 16: 777–795.
Walton JN, Tomlinson BE, Pearce GN . Subacute ‘poliomyelitis’ and Hodgkin's disease. J Neurol Sci 1968; 6: 435–445.
Löffel M et al. Impfpoliomyelitis bei einem Erwachsenen unter Chemotherapie wegen Non-Hodgkin-lymphoms (Vaccine poliomyelitis in an adult undergoing chemotherapy for non-Hodgkin lymphoma). Schweiz Med Wochenschr 1982; 12: 419–421.
Rodriguez M, Oleszak E, Leibowitz J . Theiler's murine encephalomyelitis: a model of demyelination and persistence of virus. Crit Rev Immunol 1987; 7: 325–365.
Rodriguez M, Patick AK, Pease LR . Abrogation of resistance to Theiler's virus-induced demyelination in C57BL mice by total body irradiation. J Neuroimmunol 1990; 26: 189–199.
Murray PD et al. Biphasic and regionally-restricted chemokine expression in the central nervous system in the Theiler's virus model of multiple sclerosis. J Neurovirol 2000;(Suppl 1):S44–S52.
Bruno RL . Paralytic vs ‘nonparalytic’ polio: distinction without a difference? Am J Phys Med Rehabil 2000; 79: 4–12.
Acknowledgements
This work was supported in part by Hungarian Research Fund Grants (OTKA T-025827, T-032499 and T-046128) and a Ministry of Education Grant ‘Széchenyi’ (OM 1/008/2001).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ésik, O., Vönöczky, K., Lengyel, Z. et al. Characteristics of radiogenic lower motor neurone disease, a possible link with a preceding viral infection. Spinal Cord 42, 99–105 (2004). https://doi.org/10.1038/sj.sc.3101552
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101552