Abstract
Purpose
To evaluate the long-term outcome of combined penetrating keratoplasty (PKP) and vitreoretinal surgery using temporary keratoprosthesis (TKP).
Methods
A retrospective study of 107 eyes with coexisting corneal and vitreoretinal diseases that underwent combined PKP and vitreoretinal surgery using TKP. Corneal graft clarity, intraocular pressure, and anatomical reattachment of retina were followed.
Results
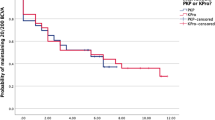
The mean follow-up time was 25 months, the longest being 8 years. Successful surgical outcome was defined as maintenance of clear graft, anatomic reattachment of retina, and controlled intraocular pressure. A total of 78 eyes (72.9%) fulfilled these criteria. Surgical intervention within 1 month of ocular injury was associated with higher success rate (81.9%) than intervention at 1 month or more after injury (54.3%). Success rate for reattachment of retina was 95.8% when preoperative proliferative vitreoretinal retinopathy (PVR) was absent compared with 83.1% when preoperative PVR was present. Unsatisfactory postoperative visual acuity was due to graft failure, recurrent PVR, or secondary glaucoma.
Conclusion
Combined PKP and vitreoretinal surgery is best performed within 1 month of ocular injury for best surgical outcome. Careful selection of cases plays an important role in reducing the risks of complications. TKP is a useful adjunct in the surgery.
Similar content being viewed by others
Introduction
In patients with coexisting corneal and vitreoretinal pathology, it is sometimes necessary to perform combined penetrating keratoplasty (PKP) with vitreoretinal surgery for purpose of restoring their visual function to their best potential. Several retrospective studies have reported on the use of temporary keratoprosthesis (TKP) in combined PKP and vitreoretinal surgery with favourable outcomes.1, 2, 3, 4 The largest series was reported by Garcia-Valenzuela et al,4 which included 31 eyes. However, study sample size for this kind of surgery is usually small, and reports on the long-term outcome are lacking. Long-term follow-up of combined PKP with vitreoretinal surgery is important because these eyes often sustain severe damages and complications can arise at a later date. In this study, we included 107 traumatic cases with combined PKP and vitreoretinal surgery using TKP performed at our hospital between 1994 and 2002. The longest follow-up was 8 years. Our results are reported herein.
Patients and methods
This study was performed with approval from the ethics committee of our hospital. A review of medical records identified 119 nonconsecutive cases of combined PKP and vitreoretinal surgery using TKP performed at the Shandong Eye Institute and Hospital between 1994 and 2002. A total of 12 patients were lost to follow-up and excluded from the study. Of the 107 eyes studied, 86 eyes were from male patients and 21 from female patients. The mean patient age was 32.3 years (6–78 years). All eyes were trauma-related with a wide spectrum of corneal and vitreoretinal pathology sustained (Table 1). Each eye had some degree of lens damage, such as cataract, lens rupture, or extrusion of lens. Three eyes had cataract extraction with intraocular lens implantation prior to combined PKP with vitreoretinal surgery. Among the 107 eyes, 11 eyes were monocular.
Surgical technique
After adequate anaesthesia was obtained with a Van Lint and a retrobulbar injection, both using a 50 : 50 mixture of 2% lidocaine and 0.75% bupivicaine, with 75 U of wydase, a lid speculum was inserted. A 360° peritomy was performed. Tenon's fascia was dissected, and all four recti muscles were identified and sutured with traction sutures. An infusion port was inserted at the pars plana and sutured to the sclera. Two more ports were prepared at the pars plana with an MVR blade and temporarily closed with metal plugs. The diseased portion of the cornea was excised with a corneal trephine (Storz, St Louis, MO, USA) of diameter 7.25 or 8.25 mm depending on the size of the diseased portion. A Landers third-generation TKP (Ocular Instruments, Bellevue, WA, USA) of 7.2 or 8.2 mm in diameter, which was 0.05 mm less than the diameter of the chosen corneal trephine, was sutured onto the recipient cornea with six interrupted 9-0 nylon sutures. Standard three-port pars plana vitrectomy was then performed. Cataract was removed by pars plana lensectomy; intraocular lens (three eyes) was removed because they were decentred and distorted the view of the posterior segment. Depending on the retinal pathology, vitreoretinal surgery was performed. Retinal reattachment surgery consisted of the combination of gas/fluid exchange, endolaser, cryotherapy, retinal pneumopexy, sclera buckling, retinoctomy, or retinectomy as needed (Table 2). After additional retrobulbar anaesthesia was given, a flieringa ring was sutured onto the sclera with 8-0 silk sutures. The TKP was then removed and replaced with donor corneal button (7.5 or 8.5 mm) with diameter 0.25 mm larger than the trephine. The donor cornea was sutured onto the recipient cornea with 16 interrupted 10-0 nylon sutures. During PKP, intraocular pressure was adjusted by regulating the flow through the infusion port. All corneal suture knots were buried. Intraocular pressure was slowly brought to normal. Silicon oil would be injected at this stage if indicated. After closure of the sclerostomy site and peritomy, 20 000 U of gentamicin and 2.5 mg of dexamethasone were injected subconjunctivally. The surgery was performed with general anaesthesia in patients ≤14 years.
Postoperative management
The patients received 240 000 U of tobramycin and 100 mg of hydrocortisone intravenously for 3 days. Topical dexamethasone and chloramphenicol were given three times a day for 1 month. In order to prevent graft rejection, 0.5% topical cyclosporine three times a day and 2% cyclosporine ointment at night were introduced on day 15 after the cornea re-epithelialized and continued till the sutures were removed 1 year later. If graft rejection occurred despite treatment, concentration of topical cyclosporine would be increased to 1%, and oral prednisone (1–1.5 mg/kg) would be added and tapered after 1 week.
The patients with silicon oil or C2F6 tamponade were suggested face-down position till the silicon oil was removed or the gas was absorbed.
Follow-up
If everything appeared stable after surgery, the patient would be discharged home and asked to return for follow-up in 2 weeks. Visual acuity, intraocular pressure, graft clarity, and anatomical status of retina were evaluated. If corneal clarity precluded visualization of retina, B-scan ultrasonography was performed. The patients were scheduled to return at 1, 3, 6 and 12 months and then every 3–6 months thereafter. The follow-up ranged from 6 months to 8 years with a mean of 25 months.
Statistical analysis
Comparisons were performed using χ2-test (SPSS 10.0 for Windows; SPSS Inc., Chicago, IL, USA). P<0.05 was considered statistically significant.
Results
Best-corrected visual acuity (BCVA) before combined corneal and retinal surgery ranged from hand motion to light perception. The majority of patients (86 eyes) had final BCVA between 20/200 to hand motion. Spectacles were accepted only for the monocular.
Successful surgical outcome was defined as maintenance of clear graft, anatomic reattachment of retina, and controlled intraocular pressure. Surgical outcome was summarized in Table 3. The success rate for surgical intervention within 1 month of ocular injury was 81.9%, in contrast with 54.3% when surgical intervention occurred at 1 month or more after injury. In total, 78 eyes (72.9%) met our criteria of successful surgical outcome.
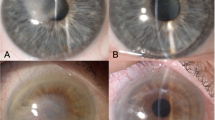
Graft cloudiness was mainly the result of graft rejection. Corneal graft rejection occurred in 34 eyes (31.8%), among which 18 eyes could be controlled medically and two eyes eventually required repeat PKP for graft failure. The other 14 grafts were left cloudy with no repeat PKP at the request of patients. Graft infection occurred in one eye with subsequent uncontrolled endophthalmitis, and therefore the eye was enucleated. Consequently, clear corneal graft was maintained in 80 eyes (74.8%) and two additional eyes acquired clear grafts after repeat PKP. The mean endothelial cell densities of the clear grafts were 2858 cells/mm2 preoperatively and 1818 cells/mm2 at last visit, with 36.4% of endothelial cell loss.
Reattachment of retina occurred in 95.8% of eyes when preoperative PVR was not present, compared with 83.1% when preoperative PVR was present. This difference was statistically significant (χ2=3.90, P<0.05). Phthisis bulbi developed in 13 eyes (12.2%) as a result of PVR but maintained visual acuity between hand motion to light perception. Retina redetached in 11 eyes (10.3%), but eight of them could be reattached after multiple surgeries. One eye was inoperable due to complicated coexisting ocular problems, the other two patients decided not to reoperate.
Secondary glaucoma was also a potential problem after surgery. In all, 15 eyes (14.0%) developed secondary glaucoma, of which 14 eyes could be controlled either medically or surgically. One eye developed absolute glaucoma and had to be enucleated because of intractable pain. It was likely that glaucoma was trauma-related because most of these eyes had extensive intraocular injury at the time of surgery.
Discussion
Totally, 107 eyes with combined PKP and vitreoretinal surgery using TKP were followed up for 6 months to 8 years in this study. 92 eyes (86.0%) could be salvaged, of which 78 eyes (72.9%) maintained corneal clarity with anatomical reattachment of retina and controlled intraocular pressure. One thing worth mentioning was that 11 patients were monocular because the fellow eye was severely damaged during the explosion. All 11 eyes were salvaged and regained useful visual function. Among them, eight eyes achieved BCVA of 20/200 or better. In contrast, Garcia-Valenzuela et al4 reported 31 cases and only 41.9% of cases maintained clear corneal graft and 22.6% of eyes became phthisical. In this study, only 12.2% of eyes (13 eyes) became phthisical.
Intraoperative factors play an important role in surgical outcome. If hypotony occurs during the open-sky situation, this may result in suprachoroidal haemorrhage. It can also affect the tension of the sutures of PKP, which can be avoided by adjusting the flow through the infusion port if the eye is filled with balanced salt solution. However, if the eye is filled with air after air-fluid exchange, this can be achieved by slowly lowering the intraocular pressure to 0 mmHg before the TKP is removed. Then slowly raise the intraocular pressure to 8 mmHg after the donor graft is secured with four cardinal sutures at 12, 3, 6, and 9 o’clock, respectively. Another precaution during surgery is to inject viscoelastics into the anterior chamber angle just prior to suturing the donor cornea to ensure that there is no peripheral anterior synaechia, which can result in chronic angle closure glaucoma.
To evaluate the success rate of combined corneal and vitreoretinal surgery, this can be viewed from two major aspects, namely, the status of corneal graft and anatomic reattachment of retina. Although the overall visual outcome of combined surgery did not appear to be affected by the presence of preoperative PVR, when the clarity of the graft was accounted for, the success rate for vitreoretinal surgery per se was significantly affected by the presence of preoperative PVR. The 13 eyes that became phthisical all had severe preoperative PVR due to delayed or improper immediate management, including two eyes complicated by subretinal haemorrhage with choroidal detachment or haemorrhage, three with coexisting retinal incarceration and two with recurrent PVR. This shows that presence of PVR is one of the risk factors contributing to surgical failure. In this study, the surgical success rate for eyes with PVR was higher if the eyes could be operated within 1 month of ocular injury. This also applied to recurrent PVR, which usually occurred within the first 2 months after surgery. Consequently, we strongly recommend early intervention in traumatic cases. Living in remote rural areas lacking modern medical facilities resulted in the delay of surgery for more than 1 month in some patients before their referral to our hospital. Moreover, the extent of the injury also plays an important role in the ultimate outcome.
The presence of preoperative corneal neovascularization accounted for the high graft-rejection rate (31.8%) in this study. The complexity of the surgery undoubtedly also increased the risk of rejection as a result of severe postoperative inflammation. We noted that most graft rejection occurred within the first year after surgery, which resembled the situation seen with routine corneal transplantation.5 This indicated that follow-up care within the first year of surgery is of paramount importance. Early detection of graft rejection and prompt treatment help to preserve the graft. Apart from graft rejection, noncompliance with treatment and follow-up was another major factor leading to the endothelial cell loss rate as high as 36.4% in eyes with clear graft after a mean follow-up of 32 months, which was way above the reported rate of 4.66% seen at 12 months after routine corneal transplantation.5 In order to minimize the amount of endothelial cell loss, apt surgical skill, choosing corneal buttons with high endothelial cell density, and patients’ education, all help to prolong the longevity of the graft.
Secondary glaucoma can result from trabecular meshwork damage, obstruction by inflammatory cells or neovascularization. Consequently, one should be aware of the potential risk of elevated intraocular pressure and instigate aggressive antiglaucoma treatment if necessary.
In addition to the above-mentioned factors, corneal astigmatism, disabling glare from iris defects, aphakia, and extensive retinal damage despite anatomic reattachment can also limit the postoperative visual rehabilitation. The monocular patients used spectacles for refractive correction. No further refractive care was taken into account, which is a major shortcoming of this study. In recent years, we have included intraocular lens implantation in the surgery, which had a significant impact on restoration of visual function. Long-term study on these patients is underway. Another shortcoming of this study is the lack of nontraumatic cases, and thus the long-term outcome of such cases warrants another study.
Although using TKP for combined PKP and vitreoretinal surgery is not without complications, it is a valuable tool in the management of complicated ocular injury, without which, many eyes cannot be salvaged. The extent of injury, the timing of operation, the likelihood of graft rejection, and the risk of retinal redetachment are all important factors that have to be considered in order to obtain the best visual outcome.
References
Gallemore RP, Bokosky JE . Penetrating keratoplasty with vitreoretinal surgery using the Eckardt temporary keratoprosthesis: modified technique allowing use of large corneal graft. Cornea 1995; 14: 33–38.
Pesko K, Stmen P . Perforation keratoplasty after pars plana vitrectomy and use of temporary keratoprosthesis. Cesk Slov Oftalmol 1998; 54: 148–153.
Chen J, Yang B, Liu Z, Wang Z, Chen L, Tang S . Temporary keratoprosthesis for surgery of severe injuries of ocular anterior and posterior segments. Chin J Ophthalmol 1998; 34: 434–437.
Garcia-Valenzuela E, Blair NP, Shapiro MJ, Gieser JP, Resnick KI, Solomon MJ et al. Outcome of vitreoretinal surgery and penetrating keratoplasty using temporary keratoprosthesis. Retina 1999; 19: 424–429.
Xie L . Corneal Transplantation. People's Medical Publishing House: Beijing, 2000, pp 141–182.
Acknowledgements
We thank Ms Ping Lin for her editorial and secretarial assistance. This study was supported in part by a grant (02KGYSH-01) from the Qingdao Municipal Science and Technology Bureau, Qingdao, China.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dong, X., Wang, W., Xie, L. et al. Long-term outcome of combined penetrating keratoplasty and vitreoretinal surgery using temporary keratoprosthesis. Eye 20, 59–63 (2006). https://doi.org/10.1038/sj.eye.6701794
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701794
Keywords
This article is cited by
-
Modified deep anterior lamellar dissection for corneal opacity during vitrectomy: case reports
BMC Ophthalmology (2020)
-
Comparative study of penetrating keratoplasty and vitreoretinal surgery with Eckardt temporary keratoprosthesis in ocular trauma versus non-trauma patients
Graefe's Archive for Clinical and Experimental Ophthalmology (2019)
-
Pars plana vitrectomy through the Boston Keratoprosthesis type 1
Eye (2013)
-
Chorioretinectomy for perforating or severe intraocular foreign body injuries
Graefe's Archive for Clinical and Experimental Ophthalmology (2010)
-
Combined anterior and posterior segment injuries in children: a review
Graefe's Archive for Clinical and Experimental Ophthalmology (2010)