Abstract
Purpose To ascertain the causes of vitreous hemorrhage and to determine the accuracy of ultrasound (U/S) in these cases, based on the degree of agreement between ultrasound and clinical findings.
Methods A chart review of 96 consecutive patients (106 eyes) with dense vitreous hemorrhage who underwent A- and B-scan U/S by one examiner between June 1996 and June 1999. U/S records were evaluated to determine the presence and exact distribution of areas of retinal detachment and the presence of posterior vitreous detachment, retinal tear, intraocular foreign body, or choroidal detachment. Clinical information was obtained from the medical records after the vitreous hemorrhage was reabsorbed or following vitreous surgery. Clinical and U/S findings were compared. False-positive and False-negative rates for U/S were calculated based on clinical findings.
Results In 37 eyes (35%) the vitreous hemorrhage was because of proliferative diabetic retinopathy and in 33 eyes (31%) because of ocular trauma. The false-positive rate for retinal detachment (retinal detachment by U/S without clinical confirmation) was 18.9% (seven of 37 eyes). Retinal tears were diagnosed and localized accurately in only four of nine eyes (44%).
Conclusions The most common cause of vitreous hemorrhage was proliferative diabetic retinopathy, followed by ocular trauma. U/S correctly diagnosed all cases of retinal detachment, but less than 50% of retinal tears. A total of 18.9% of the eyes were falsely diagnosed as having retinal detachment. U/S is an effective diagnostic tool in patients with vitreous hemorrhage.
Similar content being viewed by others
Introduction
The incidence of spontaneous vitreous hemorrhage (V-HEMO) is approximately seven cases per 100 000 of the population. Proliferative diabetic retinopathy (PDR), posterior vitreous detachment with or without retinal tear or retinal detachment (RD) and ocular trauma are the most common causes of V–HEMO. The relative prevalence of these and other underlying conditions has varied in previous reports.1,2,3,4,5 Despite recent improvements in ophthalmologic examination techniques, evaluation of vitreoretinal diseases with V–HEMO often presents a diagnostic challenge even when using the standard methods of A- and B-scan ultrasound (U/S). We conducted a retrospective study of the underlying causes of dense V-HEMO. All patients were examined by a trained U/S ophthalmologist (RY). We also assessed the rate of agreement between ultrasound and clinical findings. To our knowledge, a comprehensive study of this type has not been reported to date.
Materials and methods
We conducted a chart review of 96 consecutive patients (106 eyes) with V–HEMO who underwent A- and B-scan U/S by one examiner (RY) at the Soroka University Medical Center between June 1996 and June 1999. All patients had dense V-HEMO, which prevented visualization of the retina.
The study population included 36 women (38 eyes) and 60 men (68 eyes). The mean age for women was 63.4 years (range 12–82) and for men 50 years (range 1 month–92 years). In 10 cases, bilateral involvement was observed.
The U/S reports were evaluated to determine the underlying pathology of V–HEMO. The presence and the exact distribution of areas of RD and the presence of posterior vitreous detachment, retinal tear, intraocular foreign body, and choroidal detachment were recorded. The A- and B-scan U/S procedure for evaluating patients with V–HEMO began with the instillation of topical anesthetic drops into the eye. This was followed by the application of methylcellulose to the face of the B-scan probe to facilitate penetration of sound into the eye. Examinations were performed with patients in a supine position on the surface of the globe, to maximize sound penetration and to promote adequate patient fixation. The vitreous cavity was evaluated for hemorrhage density and mobility and other pathologies. Vitreoretinal adhesions and retinal elevations were noted by carefully screening the globe in all four quadrants. All U/S procedures were performed with the Ophthascan-S, Biophysic (ALCON SA, Clement-Fernand Cedex, France). The A-scan was used at the tissue sensitivity gain setting to assess reflectivity of the suspected pathology.
The clinical findings were determined after the V–HEMO was resorbed or following vitreous surgery, and were compared with the U/S findings. False-positive cases were defined if the U/S was positive in the absence of clinical findings. False-negative cases were defined if the U/S was negative in the presence of positive clinical findings.
Results
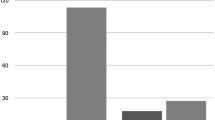
In 37 eyes (35%) the V-HEMO was because of PDR, in 33 eyes (31%) ocular trauma, in 21 eyes (20%) penetrating trauma and in 12 eyes (11.3%) blunt trauma. Post intraocular surgery was the cause in 14 eyes (13%). All the underlying causes are listed in Table 1.
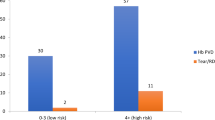
A total of 51 eyes (48%) underwent posterior vitrectomy for unabsorbed V-HEMO. Spontaneous resorption of the V-HEMO was seen in 55 eyes (52%). The mean interval between U/S and posterior vitrectomy was less than 4 weeks. Table 2 presents the accuracy of diagnostic U/S in detecting clinical findings before surgery or absorption of the hemorrhage. RD was diagnosed by U/S in 37 eyes, of which only 30 had clinical RD. Thus, all patients with clinical evidence of RD were identified correctly by U/S, but the examination gave a false-positive result in seven eyes (18.9%). In two of these patients hemorrhagic posterior vitreous detachment was mistaken for RD, and in three other patients with traction RD the ultrasonic localization of the RD was not in the exact area of the detachment.
Of the seven patients with false-positive U/S findings, six underwent a posterior vitrectomy and spontaneous resorption occurred in one. The cause of V-HEMO in these patients was PDR in five, intraocular surgery in one, and penetrating trauma in one.
There was clinical evidence of choroidal detachment, together with other pathologies, in 12 eyes (11%). Of these, 11 were correctly identified on preoperative U/S and one was not. In the undiagnosed eye (post-trauma), U/S was carried out 2 days before surgery. It is conceivable that the choroidal detachment in this eye may have occurred in the interim.
Retinal tears were detected in nine of 106 eyes (8.4%). U/S diagnosed and accurately localized these findings in four eyes (44%). Three of the four correctly diagnosed tears were in patients with spontaneous posterior vitreous detachment (two with localized RD) and one tear with localized RD followed laser therapy. Three eyes were falsely diagnosed as having retinal tears. In two eyes (one after blunt trauma and one after penetrating trauma), the tears were not accompanied by a retinal detachment; therefore, the management was based on close follow-up only until absorption occurred. The third eye with a presumed retinal tear was in a patient with PDR. The indication for surgery in this patient was for unabsorbed V-HEMO with traction RD, and not only for the presence of a retinal tear.
A false-negative result occurred in five eyes. These five tears included one following penetrating trauma with a closed funnel-shaped RD, two after spontaneous vitreous detachment with localized RD, and two in diabetic patients (one with traction RD and the other with localized RD).
Intraocular foreign bodies (all metallic) were detected in three of 106 eyes (3%). All three foreign bodies were identified on U/S, but there was a false-positive result in one eye. A posterior exit wound that was observed in one eye with a double perforation was diagnosed correctly.
Discussion
In the present study, PDR (35%) and ocular trauma (33%) were the most common causes of V-HEMO. This finding contrasts with the reports of Lindgren et al4 and Lean and Gregor,3 who reported that vitreous detachment and traction of a retinal vessel (41%) was the most common cause of hemorrhage. In our study these causes accounted for only 6.6% of the cases. One explanation for this difference in findings could be that only dense vitreous hemorrhages, which prevented visualization of the retina, were included in our study, whereas only 22% of the patients in Lindgren et al's study had this degree of dense V-HEMO. Another explanation could be that our study included traumatic as well as spontaneous V-HEMO.
Novak and Welch6 suggested that men have a four-fold risk of developing retinal tear after vitreous detachment compared to women. Interestingly, in our study, only men (five patients) had hemorrhagic posterior vitreous detachment combined with a retinal tear.
The role of U/S in the detection of RD in eyes with opaque media has been established clearly in the past.7 At present, there is no other method to reliably ascertain the anatomic position of the retina when direct examination is impossible. The demonstration of RD profoundly changes the management of the case. Thus, distinguishing dense vitreous membranes from RD is essential. In the current study, U/S correctly identified the anatomic position of the retina in 99 of 106 eyes (93.3%), with seven false positives (6.6%). There was no false-negative U/S result regarding RD (Table 2). This is in agreement with Jack et al,8 Jalkh et al,9 and Kumar et al,10 who found that the preoperative U/S correctly identified the anatomic position of the retina in 84–89% of the eyes with V-HEMO, with 8.6–12% false positives and 4–5.7% false negatives. We must emphasize that in two of our false-positive eyes, which had a suspicion of RD by U/S and underwent vitrectomy for unabsorbed hemorrhage, the management in retrospect could have been on follow-up basis only. In four other eyes, the presence of RD by U/S was not the only indication for surgery; therefore, these eyes were not operated on unnecessarily.
Some important potential sources of discrepancy between U/S and clinical findings should be taken into account. The first one stems from the dynamic nature of the surgical procedure. During membrane peeling under high infusion, for example, when areas of traction detachment become flattened at the end of the procedure, the traction detachment can be missed when the retina is finally visualized. This can lead to a ‘false’ false-positive finding in that the US result, which is, in fact, accurate, is interpreted as inaccurate because of surgically generated distortion of the clinical picture. On the other hand, traction RD can occur during surgery as a result of insertion of infusion beneath the retina or because of positive retraction of the retina itself. This can result in a ‘false’ false-negative finding. The second source of discrepancy stems from the fact that hemorrhagic PVD can be mistaken for RD since it shows 100% reflectivity by standardized A scan. The recommendation is to follow the membrane upward with an A scan and to look for a decrease in reflectivity. However, at times, since reflectivity remains at 100%, it is impossible to distinguish between the two pathologies.
Three studies of spontaneous V-HEMO11,12,13 concluded that retinal tears need to be large or giant-size in order to be detected by U/S. Nischal et al14 reported the findings of a prospective study of eight nondiabetic patients with spontaneous V-HEMO. Four were thought to have a small to moderate retinal tear on initial U/S. This was later confirmed when the hemorrhage cleared. DiBerardo et al15 published a retrospective study of the diagnosis of new retinal tears in 11 of 42 patients (26%) with spontaneous V-HEMO (excluding trauma and diabetes). The tears were small to moderate in size. They were correctly diagnosed in 10 of 11 cases (91%). In this study, one retinal tear was not diagnosed and one neo-vascular frond was mistaken for a tear. None of the patients had multiple tears or RD.
In the current study, only four out of nine tears (44%) were diagnosed correctly. All the undiagnosed tears were small and associated with a well-diagnosed RD. In most cases of rhegmatogenous RD, U/S is incapable of detecting the actual retinal tear,7 but Blumenkranz and Byrne7 showed that the retinal tear is usually present within two clock hours of the area of the greatest retinal elevation. Thus, U/S may provide indirect support for the location of retinal tear by determining the site where the detachment is most elevated. We concur with the findings of Blumenkranz and Byrne that it is very difficult to detect small tears in rhegmatogenous RD.
Diagnostic techniques such as computed tomography (CT) and plain-film radiography are standard methods for identifying intraocular foreign bodies. In the present study, diagnostic U/S correctly identified the presence of radio dense foreign bodies. Despite the high degree of sensitivity (100%) and specificity (99%) of U/S in this study, it should be considered only as an adjunct to the standard imaging techniques (CT scan) when an intraocular foreign body is suspected in post-traumatic eyes.
Our findings indicate that the combination of contact B-scan and standardized A-scan U/S provides a highly reliable method for the detection and characterization of RD and associated vitreous abnormalities. In V-HEMO, the detection of retinal tears is less accurate. Reliance on these techniques for the assessment and surgical management of patients with V-HEMO appears to be mandatory.
References
Butner RW, McPherson AR . Spontaneous vitreous hemorrhage. Ann Ophthalmol 1982; 14: 268–270.
Dana MR, Werner MS, Viana MA, Shapiro MJ . Spontaneous and traumatic vitreous hemorrhage. Ophthalmology 1993; 100: 1377–1383.
Lean JS, Gregor Z . The acute vitreous hemorrhage. Br J Ophthalmol 1980; 64: 469–471.
Lindgren G, Sjodell L, Lindblom B . A prospective study of dense spontaneous vitreous hemorrhage. Am J Ophthalmol 1995; 119: 458–465.
Spraul CW, Grossniklaus HE . Vitreous hemorrhage. Surv Ophthalmol 1997; 42: 3–39.
Novak MA, Welch RB . Complications of acute symptomatic posterior vitreous detachment. Am J Ophthalmol 1984; 97: 308–314.
Blumenkranz MS, Byrne SF . Standardized echography (ultrasonography) for the detection and characterization of retinal detachment. Ophthalmology 1982; 89: 821–831.
Jack RL, Hutton WL, Machemer R . Ultrasonography and vitrectomy. Am J Ophthalmol 1974; 78: 265–274.
Jalkh AE, Avila MP, El-Markabi H, Trempe CL, Schepens CL . Immersion A- and B-scan ultrasonography. Arch Ophthalmol 1984; 102: 686–690.
Kumar A, Verma L, Jha SN, Tewari HG, Khosla PK . Ultrasonic errors in analysis of vitreous haemorrhage. Indian J Ophthalmol 1990; 38: 162–163.
Hasenfrantz G . [Acute vitreous hemorrhage-possibilities for differential diagnostic, echographic assessment]. Fortschr Ophthalmol 1990; 87: 641–645 (German).
Jalkh AE, Jabbour N, Avila MP, Trempe CL, Schepens CL . Ultrasonographic findings in eyes with giant retinal tears and opaque media. Retina 1983; 3: 154–158.
Katsumi O, Hirose T, Kruger-Leite E, Kozlowski I, Tanino T . Diagnosis and management of massive vitreous hemorrhage caused by retinal tear. Jpn J Ophthalmol 1989; 33: 177–184.
Nischal KK, James JN, McAllister J . The use of dynamic ultrasound B-scan to detect retinal tears in spontaneous vitreous haemorrhage. Eye 1995; 9(Part 4): 502–506.
DiBernardo C, Blodi B, Byrne SF . Echographic evaluation of retinal tears in patients with spontaneous vitreous hemorrhage. Arch Ophthalmol 1992; 110: 511–514.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rabinowitz, R., Yagev, R., Shoham, A. et al. Comparison between clinical and ultrasound findings in patients with vitreous hemorrhage. Eye 18, 253–256 (2004). https://doi.org/10.1038/sj.eye.6700632
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700632
Keywords
This article is cited by
-
The BElfast Retinal Tear and detachment Score (BERT Score) in vitreous haemorrhage
Eye (2024)
-
Safety profile and surgical outcomes of early vitrectomy in eyes with unexplained fundus-obscuring vitreous haemorrhage
Eye (2023)
-
Early vitrectomy is indicated for both diffuse and dense vitreous haemorrhages of unknown aetiology
Irish Journal of Medical Science (1971 -) (2023)
-
Controversies in ocular trauma classification and management: review
International Ophthalmology (2013)
-
Predictive factors for final outcome of severely traumatized eyes with no light perception
BMC Ophthalmology (2012)