Key Points
-
Reviews evidence with regard to anaesthetic selection in common medical conditions.
-
Indicates current practice within the dental population.
-
Emphasises the need for evidence-based practice.
Abstract
Objective The aim of this study was to identify which local anaesthetic solutions were used by general dental practitioners in the United Kingdom and to determine selection criteria. In addition, differences in anaesthetic choice between recent graduates (≤5 years) and more experienced practitioners were investigated.
Material and methods Five hundred and six general dental practitioners attending postgraduate courses on pain control in dentistry completed a questionnaire. Participants were asked to indicate year and place of qualification, anaesthetic solutions available in their surgeries and criteria used in the choice of anaesthetic. In addition, the respondents were asked to indicate choice of local anaesthetic in a number of common medical conditions. Questionnaires were distributed and collected immediately prior to the start of the course presentation and participants were not asked to indicate whether the selection decisions were teaching, experience or evidence based. Data were analysed by using the Chi-square test.
Results Lidocaine with epinephrine was the most widely available solution among this group of practitioners (94%), the second most common solution was prilocaine with felypressin (74%). The majority of practitioners had two or more solutions available. Practitioners who qualified within the last five years (14%) were more likely to have articaine available, the most recently introduced local anaesthetic into the UK (p = 0.04, one degree of freedom). Common medical conditions lead to a modification in anaesthetic selection: the use of prilocaine/felypressin increases in the majority of circumstances, although it is avoided in pregnant females by recent graduates.
Conclusions Lidocaine/epinephrine continues to be the most common anaesthetic solution used by this group of UK general practitioners. The primary criterion for selection of an anaesthetic agent was perceived efficacy. Prilocaine/felypressin is commonly selected as an alternative solution in the presence of common medical conditions.
Similar content being viewed by others
Introduction
A number of local anaesthetic solutions are available in dental cartridges for use in dental practice in the UK. These are lidocaine, prilocaine, mepivacaine and articaine. Articaine is the latest agent available in cartridges in the UK and was introduced into dental practice in 1998. Solutions may be plain or in combination with a vasoconstrictor, such as epinephrine (adrenaline) or felypressin. The objective of this study was to determine the local anaesthetic solutions commonly used by dentists in the UK and dentists' reasons for selection, using a questionnaire based survey. In addition, the influence of common medical conditions on anaesthetic selection was investigated. Practitioners were not asked to indicate whether their anaesthetic choice was based on previous teaching, experience or current evidence. However, to determine if practice changes with experience, results were also analysed on the basis of time from qualification, comparing recent graduates, qualified five years or less, with 'experienced' practitioners, qualified more than five years.
Material and methods
All delegates attending postgraduate courses on pain control given by one of the authors between 2002 and 2003, throughout mainland UK, were asked to complete and immediately return an 'anonymous' questionnaire relating to the use of local anaesthesia immediately prior to the start of the course presentation. Only responses from general dental practitioners were included in this study. The questionnaire requested information on year and place of qualification and which anaesthetic solutions were available in the practitioner's surgery. In addition, a list of criteria used in anaesthetic choice was given, from which any number could be selected (Table 1). The respondents were also presented with a list of common medical conditions for which they were asked to indicate their anaesthetic choice for dental treatment (Table 2).
Results
Six hundred and ten participants attended the courses, all of whom were given and who returned a questionnaire prior to the course presentation. Five hundred and eighteen of the participants were general dental practitioners (85%); the remainder indicating specialist, community, hospital or mixed practice. A total of 506 questionnaires were analysed, 12 questionnaires being incomplete for information including year of graduation and therefore excluded. The range of length of practice was one to 45 years, with a mean of 17 years (Fig. 1). Ninety-seven per cent of respondents were UK graduates and all British dental schools were represented. Gender distribution was not considered within this survey.
Anaesthetic solutions
The anaesthetic solutions reported to be available for use are shown in Figure 2. Ninety-four per cent of respondents reported having lidocaine with epinephrine; the second most common solution was prilocaine with felypressin, 74%. The vast majority of practitioners had two or more solutions available for use (Fig. 3). Seventy per cent of respondents had at least lidocaine/epinephrine and prilocaine/felypressin solutions available. Among those practitioners not using lidocaine/epinephrine, the majority (65%) had prilocaine/felypressin, 42% in combination with articaine/epinephrine.
When comparing practitioners qualified five years or less to those qualified more than five years, the newer graduates were more likely to have articaine/epinephrine available (x2 = 4.17; p = 0.04, one degree of freedom [df]). No other significant difference in availability between the practitioner groups was found.
Selection criteria
Selection criteria responses are shown in Figure 4. The most common reason for selection of anaesthetic in both groups was efficacy (74%). Significantly more 'experienced' practitioners selected efficacy (x2 = 11.19; p = 0.0008, 1 df). Only price demonstrated a similar disparity, again with a higher number of experienced practitioners selecting this criterion (x2 = 9.92; p = 0.002, 1 df).
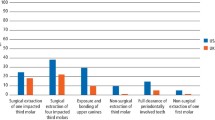
Medical conditions
When asked to indicate their first choice anaesthetic agent for a 'healthy' patient, 81% of practitioners selected lidocaine/epinephrine, 10% articaine/epinephrine and 4% prilocaine/felypressin. Ninety-two per cent of practitioners selected an epinephrine containing solution. When considering use on patients at the extremes of age, lidocaine/epinephrine was still the most common anaesthetic agent. Seventy-two per cent of practitioners employed the solution in the elderly and 80% in children. More experienced practitioners were more likely to use prilocaine/felypressin in these patients than their newly qualified counterparts (elderly, x2 = 4.45; p = 0.035: children, x2 = 3.86; p = 0.049, 1 df). Seventy-seven per cent of practitioners reported that they would use lidocaine/epinephrine and 9% prilocaine/felypressin for pregnant patients. Lidocaine/epinephrine was more commonly used by newly qualified practitioners for pregnant patients, none of whom used prilocaine/felypressin (x2 = 8.11; p = 0.0044, 1 df).
The use of epinephrine-free solutions increased when dealing with patients with cardiac conditions. Prilocaine/felypressin was most commonly selected for patients with a history of hypertension, 43%, compared with lidocaine/epinephrine 40%. When comparing experience, newer graduates were more likely to use lidocaine/epinephrine in hypertensive patients (x2 = 5.18, p = 0.023, 1 df). No significant difference was noted between practitioners in selection of anaesthesia for patients with a recent history of a myocardial infarction, 57% choosing prilocaine/felypressin and a further 20% choosing a solution containing no vasoconstrictor. The popularity of lidocaine/epinephrine returned when time from a myocardial infarction is greater than six months; 46% of respondents using this combination compared to 38% who would administer prilocaine/felypressin. There was a significant change from epinephrine-free to epinephrine-containing solutions when time from myocardial infarction exceeded six months (x2 = 115.60; p < 0.0001, 1 df).
In the management of asthmatic patients, three-quarters of practitioners reported using lidocaine/epinephrine. A significantly greater number of experienced practitioners indicated the use of prilocaine/felypressin compared to more recent graduates (x2 = 4.98; p = 0.026, 1 df).
There was a significant difference noted in the use of solutions between controlled and uncontrolled diabetic patients. An epinephrine-free solution was more likely to be chosen when treating uncontrolled patients (x2 = 90.14; p < 0.0001, 1df). As with asthmatics, experienced practitioners were more likely to select prilocaine/felypressin in the uncontrolled diabetic patient than recent graduates (x2 = 8.04; p = 0.0046, 1 df). Overall the presence of a medical condition (including extremes of age) influenced anaesthetic choice, with a significant move to epinephrine-free solutions (x2 = 1039.01; p = 0, 8 df). This effect was maintained when age was excluded as a 'medical condition' (x2 = 819.93; p < 0.0001, 6 df).
Discussion
The result of this study must be interpreted with caution given that the participants had all chosen to attend a pain control course and could be presumed to have an interest in the subject of anaesthesia. In addition, it is not suggested that the selection criteria of dentists taking part in the survey was evidence-based. The criteria by which individual dentists make an anaesthetic selection may be based on previous education, experience or indeed current evidence and the survey related to experience, in terms of time from qualification, only.
The most commonly available local anaesthetic solution to this group of UK general dental practitioners was lidocaine with epinephrine. This was apparently selected on the basis of efficacy, a reason that appears more important to experienced practitioners. Experienced practitioners also indicated price as a selection criteria significantly more often than recently qualified colleagues. This might reflect the possibility that there may be a greater number of practice principals with financial responsibility in this group.
Most practitioners have two or more solutions available, in particular lidocaine/epinephrine and prilocaine/felypressin; prilocaine/felypressin appears to be primarily used in patients with a medical condition. The most recently introduced anaesthetic solution – articaine – was more commonly available to recent graduates, which may relate to their introduction to the solution in dental school. Few practitioners in this survey reported the use of mepivacaine.
In the 'healthy' patient, the solution most commonly injected was lidocaine/epinephrine. In the young and elderly, lidocaine/epinephrine was similarly seen as acceptable. Age, therefore, would not appear to be perceived as a significant factor in anaesthetic choice. Experienced practitioners, however, were more likely to consider prilocaine/felypressin in these patients than their less experienced colleagues, possibly reflecting an element of caution.
Unlike age, 'true' medical conditions appear to alter anaesthetic selection, with a significant increase in the use of epinephrine-free solutions. In the case of pregnancy, 10% of more experienced practitioners indicated prilocaine/felypressin as a suitable anaesthetic solution. No recent graduates selected this solution. The reluctance to use prilocaine/felypressin may reflect newer graduates' knowledge of a theoretical risk of felypressin inducing labour and that prilocaine may cause foetal methaemoglobinaemia.1,2 These complications, however, are unlikely to occur at dental doses.3 Whether such knowledge is forgotten with time, or experience makes the practitioner more capable of independent risk assessment is not inferred.
The choice of prilocaine/felypressin increased markedly when treating patients with cardio-vascular disease. The majority of practitioners selected this solution or an epinephrine-free solution for patients who had a myocardial infarction in the previous six months. Avoidance of epinephrine would appear to be a sensible precaution due to the possible cardiac chronotropic, inotropic and arrhythmogenic properties, effects which may be exaggerated in some patients, such as cardiac transplant recipients.4,5 However, it has also been suggested that felypressin at high concentrations may produce coronary vasoconstriction/ischaemia and its use in such cardiac conditions could also be contraindicated.1,6 A plain solution, such as 4% prilocaine, is possibly more appropriate in such patients, although selected by only 7% of practitioners – 14% selecting lidocaine. Experienced practitioners more commonly selected plain solutions than recent graduates. When time from myocardial infarction exceeded six months, selection of epinephrine-containing solutions increased significantly and was the most popular selection. In comparison, prilocaine/felypressin was the most commonly selected solution in patients with hypertension. The effect of epinephrine-containing solutions in the hypertensive patient is still open to debate: changes in systolic and diastolic blood pressures are thought to be insignificant; however, interactions with anti-hypertensive medication should be considered.7,8 Avoidance of epinephrine in uncontrolled hypertension may be an option, although such an intervention would require blood pressure measurement of all patients, a practice which is currently not routinely performed in the UK.
When selecting an anaesthetic solution for use in asthmatic patients, lidocaine/epinephrine was again most commonly selected. Experienced practitioners were more likely to select prilocaine/felypressin as an alternative anaesthetic. Neither lidocaine nor epinephrine is contra-indicated in asthmatics, however, allergy to sodium metabisulphite used as a preservative in lidocaine/epinephrine solution has been reported.9 Evidence of hypersensitivity is equivocal and appears to involve a sub-set of severe, steroid-controlled asthmatics; avoidance in this small population has been recommended.10
A significant move to epinephrine-free solutions in patients with uncontrolled diabetes compared to controlled diabetes was noted, predominantly in the experienced practitioner group. Epinephrine-containing dental local anaesthetic solutions have been shown to produce an increase in blood glucose levels of dental patients.11 The mechanism of hyperglycaemia appears complex, involving inhibition of insulin release, glycogenolysis and gluconeogenesis.12,13,14 Given that the effect is not insulin mediated, rise in blood glucose should be of similar small magnitude in both non-diabetic and diabetic patients and would be unlikely to be hazardous to a well-controlled diabetic.11,15 The cumulative effect in an uncontrolled diabetic with pre-existing elevated glucose levels is similarly unlikely to be significant in relative terms. Given the paucity of data relating to this phenomenon in the uncontrolled diabetic, caution in administration of epinephrine by general practitioners is not unreasonable.
Unlike this current report, a similar study of 133 dentists in Brazil reported prilocaine as the most commonly used anaesthetic (86%), selected similarly on the basis of efficacy.16 Lidocaine was only preferred for use in pregnant women. In an earlier questionnaire survey of 911 German dentists, recording 2,731 patient episodes, articaine/epinephrine was the predominant solution, administered in 91% of procedures compared with lidocaine/epinephrine in 2%.17 Plain mepivicaine use increased with increasing patient 'risk factors', plain lidocaine use conversely decreased; the use of prilocaine was not recorded. Forty-six per cent of patients had one or more medical conditions, 20% of patients having cardiovascular disease. The study concluded that 'differentiated anaesthesia' tailored to patient risk factors should be employed. The results of the present investigation suggest that such differentiation was apparent among this group of dental practitioners in the UK.
Conclusions
In conclusion, lidocaine, with the vasoconstrictor epinephrine, was found to be the most commonly available anaesthetic solution in this group of UK general dental practitioners. The solution was selected most frequently on its effectiveness. Lidocaine has been used in dentistry for over 50 years and has been available in dental cartridges longer than any other agent used in the UK. The results of the present study suggest that at least some dentists in the UK still consider it to be the 'gold standard' dental local anaesthetic. Prilocaine with felypressin was available to most practitioners, its use being predominantly in patients with known medical conditions, including cardiovascular disease, asthma and diabetes, despite a lack of contra-indication to lidocaine/epinephrine in the majority of patients with the latter two conditions. More experienced practitioners appear more cautious in their anaesthetic selection, choosing prilocaine/felypressin significantly more often. Recent graduates may modify their selection on the basis of theoretical risk in the case pregnancy.
The disparity in anaesthetic selection between groups may represent variation in education or personal experience and indicates the need for review and evidence-based practice.
References
Roberts DH, Sowray JH . Local analgesia in dentistry. 2nd ed. pp 33–34. Bristol: Wright, 1979.
Rood JP . Local analgesia during pregnancy. Dent Update 1981; 8: 483–485.
Watson AK . Local anaesthetics in pregnancy. Br Dent J 1988; 165: 278–279.
Perusse R, Goulet J-P, Turcotte, J-Y . Contraindications to vasoconstrictors in dentistry: Part I. Oral Surg Oral Med Oral Pathol 1992; 74: 679–686.
Meechan JG, Parry G, Rattray DT, Thomason JM . Effects of dental local anaesthetics in cardiac transplant recipients. Br Dent J 2002; 192: 161–163.
Sunada K, Nakamura K, Yamashiro M, et al. Clinically safe dosage of felypressin for patients with essential hypertension. Anesth Prog 1996; 43: 108–115.
Meechan JG . Plasma potassium changes in hypertensive patients undergoing oral surgery with local anaesthetics containing epinephrine. Anesth Prog 1997; 44: 106–109.
Bader JD, Bonito AJ, Sugars DA . A systematic review of cardiovascular effects of epinephrine on hypertensive dental patients. Oral Surg Oral Med Oral Path Oral Radiol Endod 2002; 93: 647–653.
Blackmore JW . Local anesthetic and sulfite sensitivity. Can Dent Assoc J 1988; 54: 249–252.
Perusse R, Goulet J-P, Turcotte, J-Y . Contraindications to vasoconstrictors in dentistry: Part II. Oral Surg Oral Med Oral Pathol 1992; 74: 687–691.
Meechan JG . The effects of dental local anaesthetics on blood glucose concentration in healthy volunteers and in patients having third molar surgery. Br Dent J 1991; 170: 373–376.
Rosa RM, Silva P, Young JB, et al. Adrenergic modulation of extrarenal potassium disposal. New Eng J Med 1980; 302: 431–434.
Whyte KF, Addis GJ, Whitesmith R, Reid JL . Adrenergic control of plasma magnesium in man. Clin Sci 1987; 72: 135–138.
Exton JH, Robison GA, Sutherland EW, Park CR . Studies on the role of adenosine 3′, 5′-monophosphate in the hepatic actions of glucagons and catecholamines. Biol Chem 1971.
Esmerino LA, Ranali J, Rodrigues AL . Blood glucose determination in normal and alloxan-diabetic rats after administration of local anesthetics containing vasoconstrictors. Braz Dent J 1998; 9: 33–37.
Ramacciato JC, Ranali J, Volpato MC, Groppo FC, Flório FM, Soares PCO . Local anesthetics use by dentists profile. J Dent Res 2002; 81(Spec Iss B): 491.
Daubländer M, Muller R, Lipp MDW . The incidence of complications associated with local anesthesia in dentistry. Anesth Prog 1997; 44: 132–141.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Corbett, I., Ramacciato, J., Groppo, F. et al. A survey of local anaesthetic use among general dental practitioners in the UK attending postgraduate courses on pain control. Br Dent J 199, 784–787 (2005). https://doi.org/10.1038/sj.bdj.4813028
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4813028
This article is cited by
-
Inferior alveolar nerve block: is articaine better than lidocaine?
British Dental Journal (2021)
-
Articaine buccal infiltration vs lidocaine inferior dental block – a review of the literature
British Dental Journal (2016)
-
Drug interactions in general dental practice – considerations for the dental practitioner
British Dental Journal (2014)
-
The efficacy of infiltration anaesthesia for adult mandibular incisors: a randomised double-blind cross-over trial comparing articaine and lidocaine buccal and buccal plus lingual infiltrations
British Dental Journal (2010)
-
Shortages of LA
British Dental Journal (2006)