Abstract
Study design:
Prospective randomized single blind study.
Objectives:
To find out the incidence of deep vein thrombosis (DVT) in Indian acute spinal cord injury (ASCI) subjects with and without pharmacological prophylaxis.
Setting:
Indian Spinal Injuries Centre.
Methods:
Seventy four ASCI subjects were randomly divided into two groups with 37 subjects each: group I received no antithrombotic prophylaxis, and only physical measures like compression stockings were employed for prophylaxis, whereas group II received antithrombotic prophylaxis with low-molecular weight heparin (LMWH) along with physical measures as in group I. DVT was monitored through daily clinical assessment and doppler venous ultrasonography at 2 weeks.
Results:
Out of 37 subjects in each group, eight (21.6%) developed DVT in group I and two (5.4%) in group II. The difference was significant (P-value=0.041). Six out of eight subjects who developed DVT in group I were asymptomatic. There was no incidence of significant DVT-related complications including pulmonary embolism in any of the subjects.
Conclusions:
There is a significant incidence of DVT in Indian subjects with ASCI but definitely less than what has been reported in western literature. Pharmacological prophylaxis (LMWH in this study) significantly (P=0.041) decreases the incidence of DVT in subjects with ASCI. As there was no difference in the incidence of symptomatic DVT or related complications, a larger study would be required to conclude definitely on the role of pharmacological prophylaxis in the Indian population.
Similar content being viewed by others
Introduction
Deep vein thrombosis (DVT) and its sequel, pulmonary embolism (PE), are the leading causes of preventable in-hospital mortality throughout the world.1, 2 The exact incidence of DVT in acute spinal cord injury (ASCI) is unknown because most studies are limited by the inherent inaccuracy of clinical diagnosis.3, 4 In hospitalized patients, the incidence of venous thrombosis is considerably higher and varies from 20 to 70% and PE ranges from 0.5 to 3%.5, 6 Amongst the various groups of hospitalized patients, those with spinal cord injury (SCI) have one of the highest incidences of DVT (60–80%)5, 6 and PE (3–5%)7, 8 compared with any other hospitalized medical or surgical patient group.
The above reported incidence of DVT is based on various studies in European and American populations. In Asian population, it has not been well highlighted and ranges from 6–75%.9, 10, 11 Majority of these studies are focussed on arthroplasty patients and only a few on patients with ASCI.12, 13, 14 The risk of DVT is highest in the first 3 months following SCI and declines after 3 months,8 maximum (80%) being in the first 2 weeks.15 Because of the inaccuracy of the clinical diagnosis of venous thrombosis,3, 4 it is essential that reliable objective diagnostic methods be used. Techniques include doppler ultrasonography of the lower limbs, impedance plethysmography and ascending venography. Among various modalities, doppler ultrasonography has the advantage of being non-invasive, cost effective, replicable, safe with no side effects, and matches venography in sensitivity and specificity.16, 17
The need for systemic thromboprophylaxis, especially in SCI patients, is based on the high prevalence of DVT and PE.6, 18 There are various guidelines and recommendations worldwide for prophylaxis of DVT in ASCI.19 Guidelines developers recommend that thromboprophylaxis be provided to all patients with ASCI. They recommend against the use of low-density unfractionated heparin, graduated compression stockings or intermittent pneumatic compression as single prophylaxis modalities. In patients with ASCI, the guidelines recommend prophylaxis with low-molecular weight heparin.
However, thromboprophylaxis in patients with ASCI in India is not routinely practiced and is generally reserved for high-risk cases. The reason for this low emphasis on thromboprophylaxis may be because of the perception that the incidence of venous thromboembolism is lower than that in the western world; however, there are not enough studies and trials to substantiate or negate this perception in patients with ASCI. Critics suggest that the low-reported incidence may be because of lack of reporting of all diagnosed cases, suboptimal follow-up of SCI patients and also the fact that majority of thromboembolic events are clinically silent and may be often missed.
The purpose of this study was to find out the incidence of DVT in subjects with ASCI and also to find out whether routine prophylaxis with low-molecular weight heparin is required or not.
Materials and methods
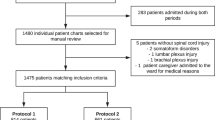
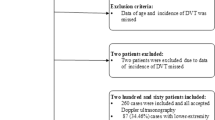
After approval from the Institutional ethics committee, a prospective randomized single blind study was conducted at Indian Spinal Injuries Centre on 74 subjects with ASCI between December 2006 and December 2010. Only subjects with ASCI (⩽5 days) were included in the study.
Subjects with known risk factors of DVT, that is, those with previous history of DVT, chronic venous insufficiency, associated injuries, stroke, varicose veins, large malignancy, renal insufficiency, recent myocardial infarction, heart failure, those taking oral contraceptive pills or steroids or hormonal drugs or anticoagulant drugs, were excluded from the study.
A simple blocked randomization was performed before the initiation of the study. The randomization allocation was concealed. Subjects were randomized and divided into two groups, each having 37 subjects as under:
-
✓ Group I received no antithrombotic prophylaxis and only physical measures like compression stockings were employed for prophylaxis.
-
✓ Group II received antithrombotic prophylaxis with low-molecular weight heparin along with physical measures as in group I.
Enoxaparin (40 mg) was given subcutaneously once a day, starting on the day of admission and was continued for 8 weeks. It was omitted on the morning of surgery and was restarted the next day. Assessment/screening for DVT was done through color doppler venous ultrasonography in all subjects at the end of 2 weeks following injury +/−2 days and earlier or later if symptoms suggestive of DVT were noted. All the doppler examinations were performed by the same radiologist who was blinded to randomization allocation and subjects were assessed for flow, visualized thrombus, compressibility and augmentation.
Assessment included examination of bilateral superficial femoral, femoral, popliteal, anterior tibial and posterior tibial veins. A diagnosis of DVT was made when there was visualization of thrombus, absence of flow, lack of compressibility and augmentation. Subjects were also assessed clinically on daily basis for signs and symptoms of DVT and PE. Apart from demographic data like age and sex, variables that could influence the incidence of DVT such as the level of injury, duration of injury, degree of deficit (American Spinal Injury Association (ASIA) Impairment Scale (AIS) ), surgical approach used, interval between injury and surgery, time duration of surgery as well as interval between injury and wheelchair mobilization were recorded.
Subjects were also monitored for symptomatic DVT. A subject was suspected to have symptomatic DVT when they had one of the following criteria:
-
A significant increase (>3 cm) in the circumference of the thigh or calf (unilateral edema)
-
An increase in the venous pattern of collateral veins in the affected extremity
-
A low-grade fever of unknown origin
With documented DVT, mobilization and exercise of the affected extremity were withheld for 72 h followed by gradual mobilization. Enoxaparin was given in a dose of 1 mg kg−1 subcutaneously 12 hourly for another 3 months.
The χ2-test was applied to analyze the difference between two categorical variables and independent t-test for continuous variables. P-value <0.05 was considered statistically significant.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human subjects were followed during the course of this research.
Results
There were a total of 74 subjects with 37 in each group. The groups were homogenous and there was no statistically significant difference on intergroup analysis for various variables (Table 1) except for gender distribution (P-value 0.003).
Out of 37 subjects in each group, eight (21.6%) developed DVT in the non-prophylactic group, and two (5.4%) developed DVT in the prophylactic group. The difference was found to be statistically significant (P-value 0.041).
Subgroup analysis revealed a statistically significant difference in incidence of DVT between the two groups (Table 2) for various variables like paraplegia (P-value 0.05), completeness of injury (P-value 0.03), posterior approach for surgery (P-value 0.03) and absence of clinical signs and symptoms (P-value 0.02).
DVT was symptomatic only in two subjects in each group. However, there were a significant number of subjects in group I who had no symptoms but were confirmed to have DVT on doppler venous ultrasonography, whereas in group II there were no such subjects. This difference between groups was statistically significant. There was no difference in the incidence of DVT-related complications.
Discussion
The two groups were homogenous except for gender distribution, which may not be of significance as gender does not influence incidence of DVT.
Several studies based on various groups of patients state a low incidence of DVT in Asian population.9, 10 However, studies by Parakh et al.11 stated that the incidence is comparable to that in the western literature. Studies that are done from India are mainly based on arthroplasty and hip surgery patients. Published data on the risk of DVT in ASCI in Indian/Asian population is sparse and studies by Rathore et al. in 2008, Saraf et al. in 2007 and, Agarwal et al.12, 13, 14 in 2009 reported an incidence of 4.8%, 10% and 3%, respectively.
The incidence of DVT in this study was found to be 21.6% in those subjects with SCI in whom no pharmacological prophylaxis was used and only physical measures were employed, and an incidence of 5.4% in those in whom prophylaxis was given. The difference in the two groups was statistically significant (P=0.041). Even on the intergroup analysis for various variables that are known to influence the incidence of DVT (posterior approach for surgery and completeness of injury), there was a statistically significant difference in incidence of DVT between the two groups thus reinforcing the benefit of thromboprophylaxis. Stratification of the sample probably resulted in reducing the power for certain subgroup analysis. This may have been the reason for lack of a statistically significant difference for these subgroups.
The incidence of DVT in our study is definitely much higher than the reported incidence in Indian patients (3.0–10%)12, 13, 14 but certainly less than what has been reported in the western literature (60–80%).5, 6 However, the incidence of symptomatic DVT was equal in both groups and there were no DVT-related complications in both the groups.
This lower incidence has been attributed to several factors like high fibrinolytic activity, inherited resistance to thrombosis formation, complete lack of activated protein C resistance, a higher incidence of blood group O, low socioeconomic status leading to consumption of low fat diet, lower incidence of obesity, climatic differences and the practice of massage by attendants.14 Critics suggest that the most important factor may be lack of awareness and proper studies on incidence of DVT in SCI. Another factor that affects the incidence of DVT is the mode of screening, whether routine screening20 is carried out in all patients with SCI or only in patients who exhibit signs and symptoms of DVT.9 The lower reported incidence of DVT in our country may be due to the lack of routine screening of patients with SCI for DVT, and it has been proved by studies that majority of patients with DVT in SCI are asymptomatic and serial calf measurements and clinical signs and symptoms are a poor predictor of DVT in patients with SCI.3, 4 This observation was reinforced in this study too as six out of eight patients who developed DVT in the non-prophylactic group were asymptomatic. Owing to the lack of authentic data on the incidence of DVT in Indian population sustaining SCI, there is confusion/debate on whether to routinely use thromboprophylaxis in patients with ASCI.
In this study, we used color doppler ultrasonography for diagnosis of DVT. Doppler ultrasonography is non-invasive and can be repeated as many times as required.
The study demonstrates that there is significant incidence of DVT in ASCI in Indian population and pharmacological prophylaxis with low-molecular weight heparin significantly decreases the incidence. There was a statistically significant higher incidence of asymptomatic DVT in the non-prophylactic group. However, as there was no difference in the incidence of symptomatic DVT or significant complications of DVT like PE in the two groups, the question whether pharmacological prophylaxis should be routinely used in subjects with ASCI remains unanswered. This may be due to a smaller sample size in the study. Hence, a larger study based on finding the actual incidence of PE in Indian patients with ASCI would be required to conclude definitely in this regard. The difficulty in documenting PE in the Indian circumstances has to be kept in mind while designing this study.
Limitations of the study
The relatively small sample size and the use of doppler test routinely only once at 2 weeks were the limitations of the study. Even though there was a provision to repeat the doppler if there were any signs or symptoms suggestive of DVT, some asymptomatic DVT occurring after 2 weeks may have been missed.
Certain variables such as blood group and massage, which may influence the incidence of DVT, have not been taken into consideration in this study.
Conclusion
There is a significant incidence of DVT in Indian patients with ASCI but definitely less than what has been reported in western literature. Pharmacological prophylaxis with low-molecular weight heparin significantly decreases the incidence of DVT in patients with ASCI. However, as there was no difference in the incidence of symptomatic DVT or significant DVT-related complications in the study and control groups, a larger study would be required to draw a definite conclusion on the role of pharmacological prophylaxis in the Indian population.
Data Archiving
There were no data to deposit.
References
Lindblad B, Eriksson A, Bergqvist D . Autopsy-verified pulmonary embolism in a surgical department: analysis of the period from 1951 to 1988. Br J Surg 1991; 78: 849–852.
Sandler DA, Martin JF . Autopsy proven pulmonary embolism in hospital patients: are we detecting enough deep vein thrombosis? J R Soc Med 1989; 82: 203–205.
Chu DA, Ahn JH, Ragnarsson KT, Helt J, Folcarelli P, Ramirez A . Deep venous thrombosis: diagnosis in spinal cord injured patients. Arch Phys Med Rehabil 1985; 66: 365–368.
Swarczinski C, Dijkers M . The value of serial leg measurements for monitoring deep vein thrombosis in spinal cord injury. J Neurosci Nurs 1991; 23: 306–314.
Anderson FA Jr, Wheeler HB, Goldberg RJ, Hosmer DW, Patwardhan NA, Jovanovic B et al. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT Study. Arch Intern Med 1991; 151: 933–938.
Geerts WH, Heit JA, Clagett GP, Pineo GF, Colwell CW, Anderson FA Jr et al. Prevention of venous thromboembolism. Chest 2001; 119: 132S–175SS.
Walsh JJ, Tribe C . Phlebo-thrombosis and pulmonary embolism in paraplegia. Paraplegia 1965; 3: 209–213.
Watson N . Venous thrombosis and pulmonary embolism in spinal cord injury. Paraplegia 1968; 6: 113–121.
Jain V, Dhaon BK, Jaiswal A, Nigam V, Singla J . Deep vein thrombosis after total hip and knee arthroplasty in Indian patients. Postgrad Med J 2004; 80: 729–731.
Nathan S, Aleem MA, Thiagarajan P, Das De S . The incidence of proximal deep vein thrombosis following total knee arthroplasty in an Asian population: a Doppler ultrasound study. J Orthop Surg (Hong Kong) 2003; 11: 184–189.
Parakh R, Kapadia SR, Sen I, Agarwal S, Grover T, Yadav A . Pulmonary embolism: a frequent occurrence in Indian patients with symptomatic lower limb venous thrombosis. Asian J Surg 2006; 29: 86–91.
Agarwal NK, Mathur N . Deep vein thrombosis in acute spinal cord injury. Spinal Cord 2009; 47: 769–772.
Rathore MF, Hanif S, New PW, Butt AW, Aasi MH, Khan SU . The prevalence of deep vein thrombosis in a cohort of patients with spinal cord injury following the Pakistan earthquake of October 2005. Spinal Cord 2008; 46: 523–526.
Saraf SK, Rana RJ, Sharma OP . Venous thromboembolism in acute spinal cord injury patients. Indian J Orthop 2007; 41: 194–197.
Merli GJ, Crabbe S, Paluzzi RG, Fritz D . Etiology, incidence, and prevention of deep vein thrombosis in acute spinal cord injury. Arch Phys Med Rehabil 1993; 74: 1199–1205.
Mitchell DC, Grasty MS, Stebbings WS, Nockler IB, Lewars MD, Levison RA et al. Comparison of duplex ultrasonography and venography in the diagnosis of deep venous thrombosis. Br J Surg 1991; 78: 611–613.
Rose SC, Zwiebel WJ, Nelson BD, Priest DL, Knighton RA, Brown JW et al. Symptomatic lower extremity deep venous thrombosis: accuracy, limitations, and role of color duplex flow imaging in diagnosis. Radiology 1990; 175: 639–644.
Thromboembolic Risk Factors (THRIFT) Consensus Group. Risk of and prophylaxis for venous thromboembolism in hospital patients. BMJ 1992; 305: 567–574.
Geerts WH, Pineo GF, Heit JA, Bergqvist D, Lassen MR, Colwell CW et al. Prevention of venous thromboembolism: the seventh ACCP Conference on antithrombotic and thrombolytic therapy. Chest 2004; 126: 338S–400S.
Furlan JC, Fehlings MG . Role of screening tests for deep venous thrombosis in asymptomatic adults with acute spinal cord injury: an evidence-based analysis. Spine (Phila Pa 1976) 2007; 32: 1908–1916.
Acknowledgements
We acknowledge the contribution of Mr Kulwant Singh in statistical analysis of the data and that of Dr Vandana Phadke for her help in finalizing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Halim, T., Chhabra, H., Arora, M. et al. Pharmacological prophylaxis for deep vein thrombosis in acute spinal cord injury: an Indian perspective. Spinal Cord 52, 547–550 (2014). https://doi.org/10.1038/sc.2014.71
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.71
This article is cited by
-
Prevention of thromboembolism in spinal cord injury -S1 guideline
Neurological Research and Practice (2020)
-
Challenges in comprehensive management of spinal cord injury in India and in the Asian Spinal Cord network region: findings of a survey of experts, patients and consumers
Spinal Cord (2018)