Abstract
Study design:
Prospective cohort.
Objectives:
To characterize spinal cord injury (SCI)-related pain and treatment in victims of the 2008 Sichuan earthquake.
Setting:
Mianzhu County, China.
Methods:
Twenty-six patients who sustained SCI in the 2008 Sichuan earthquake and who were treated in the same hospital were enrolled. Data was collected on pain severity with a visual analog scale, depression with Patient Health Questionnaire-9, quality of life (QoL) with World Health Organization Quality of Life-BREF and social participation with the Craig Hospital Handicap Assessment and Reporting Technique Short Form at three assessment points. Detailed pain descriptions including therapeutic interventions were elicited at the fourth assessment. Pain determinants were analyzed with a longitudinal Tobit regression, and Pearson’s correlations of pain severity with depression, QoL and social participation stratified by measurement point were calculated.
Results:
SCI-related pain was highly prevalent and prevalence of neuropathic pain was nearly twice that of nociceptive pain. Most patients reported pain since the onset and severity was not significantly reduced over time. Cervical injury, complete lesions and education level were significant pain determinants. Depression and QoL scores were highly correlated with pain at the first two assessments points but not at the third measurement. Most patients did not seek treatment because they regarded pain as either a normal condition after SCI or were afraid of drug dependency.
Conclusion:
This initial longitudinal assessment and characterization of SCI-related pain in earthquake victims provides a foundation for further exploration of the biological and psychosocial determinants of pain severity and of the correlation of chronic pain with other outcomes of interest in this population. Patient pain-treatment-seeking behavior and therapeutic interventions should be evaluated concurrently.
Similar content being viewed by others
Introduction
The Sichuan earthquake of 21 May 2008 resulted in 87 476 deaths and over 12 000 severely injured persons.1 Spinal cord injury (SCI), one of the most severe disabling injuries, was sustained by an estimated 200 victims.2 Pain, an unpleasant sensory and emotional experience associated with actual or potential tissue damage,3 is a common and debilitating complication in SCI patients. Chronic pain is generally defined as continuous or intermittent presence of pain for at least 6 months, and a 3-month cut-off is sometimes used in SCI research; more often, no chronicity criterion is applied.4 Reported pain prevalence in SCI patients ranges from 25.5 to 96.2%4 and recent studies of earthquake victims show a comparable range of 33–100%.2 Heterogeneity of reported pain measures between studies, however, prevents determination of combined incidence or prevalence.4
Pain in SCI can be divided into nociceptive and neuropathic components. Neuropathic pain is caused by a lesion or disease of the somatosensory nervous system. By contrast, nociceptive pain occurs with a normally functioning somatosensory nervous system and results from actual or threatened damage to non-neural tissue due to stimulation of nociceptors.5 Chronic nociceptive and neuropathic pain have not been classified in earthquake victims with SCI.
This investigation therefore aims to longitudinally assess and comprehensively characterize SCI-related chronic pain in earthquake victims. Potential physical and psychosocial determinants of pain as well as correlations between pain and depression, quality of life (QoL) and social participation outcomes are also explored. Finally, patient treatment-seeking behavior and therapeutic interventions are examined.
Materials and methods
Design
This is a prospective cohort study with four assessment points.
Sample and attrition
The 26 SCI patients who were treated in Mianzhu Hospital, located in one of the most severely affected earthquake areas, were enrolled. All patients participated in the initial baseline assessment (from May to August 2009) and the first follow-up assessment (from August to November 2010). Two patients were lost to follow-up and one patient had died by the third assessment (July 2012). These assessments were conducted in person and the final, fourth assessment consisted of a phone interview conducted with the 23 remaining patients (October 2012). While the first three assessments points were determined by a Chinese Association of Rehabilitation Medicine protocol, the fourth assessment was organized by the authors to collect additional relevant information.
Assessments and measures
An assessment form developed by the Chinese Association of Rehabilitation Medicine protocol, which included relevant standardized measures was used to evaluate earthquake victims at the first three assessments. This form measured pain severity with a visual analog scale (VAS), ranging from 0 (no pain) to 10 (most severe pain the patient can imagine).6 Physical functioning was assessed using the Chinese version of the Barthel index which ranges from 0 (complete dependence) to 100 (complete independence).7 Social participation was measured with the Craig Hospital Handicap Assessment and Reporting Technique Short Form. This measure comprises six domains: physical independence, cognitive independence, mobility, occupation, social integration and economic self-sufficiency.8 The World Health Organization Quality of Life-BREF (WHOQOL-BREF)9 was used to assess the QoL. The first two items are self-ratings for overall QoL and health, whereas the following 24 items measure the four broad domains of physical health, psychological health, satisfaction with social relationships and with the environment. Presence and severity of depression was evaluated with the Patient Health Questionnaire-9.10 Patient demographic and SCI characteristic data including age, sex, marital status, education, level of lesion and ASIA Impairment Scale classification were abstracted from patient hospital records.
The fourth assessment employed a phone interview to elicit patient responses to questions on aspects of SCI-related pain. Pain characteristics including severity, timing, location, pattern, quality (descriptors), and aggravating and alleviating factors were queried.11, 12 Severity was assessed with a verbal rating scale corresponding to the VAS. Pain intervention information including patient treatment-seeking behavior as well as type of intervention prescribed, compliance and outcome was also elicited. ID Pain (Chinese version), a six-item questionnaire consisting of five sensory descriptor items and one item assessing pain restriction to joints (indicative of nociceptive pain), was administered to help differentiate nociceptive and neuropathic pain.13
The International Spinal Cord Injury Pain Classification was then used to classify patient pain based on patient data from the fourth assessment and the ID pain score was used to corroborate findings.5 The International Spinal Cord Injury Pain organizes pain types into a three-tiered structure: tier I includes ‘nociceptive’, ‘neuropathic’, ‘other’ and ‘unknown’ pain subtypes; tier II differentiates neuropathic pain by the site of pain relative to the level of injury as ‘at level’ and ‘below level’, as well as other; nociceptive pain is dived into ‘musculoskeletal’, ‘visceral’ and other subtypes. Tier III differentiates pain by its anatomical source and pathology and was not considered in this study. A single patient may be classified as ‘mixed’ with subtypes comprising both nociceptive and neuropathic pain types, for example, below-level neuropathic pain and nociceptive musculoskeletal pain.12
Data were independently entered by two coders and differences were reconciled.
Data analysis
Demographical and SCI characteristics of the study population were described as were pain severity and corresponding pain trajectories for the four assessments. Determinants of pain severity were analyzed with a longitudinal Tobit regression to account for the known ceiling and floor effects of VAS.14 Predictors were age, gender, marital status, education level, level of lesion, completeness of injury, employment status, patient care treatment seeking, date of VAS measurement, and an interaction of the final measurement and treatment (to account for the effect of treatment over time). The regression analysis was bootstrapped owing to the small sample size (that is, repeated on 50 random data samples with replacement of missing values based on values of the randomly selected cases) to minimize the effect of outliers.15 Bivariate Pearson’s correlations of pain with other outcomes (Craig Hospital Handicap Assessment and Reporting Technique Short Form, WHOQOL-BREF, Patient Health Questionnaire-9) were also analyzed for the first three assessments. Data on treatment modalities elicited at the fourth assessment were descriptively analyzed. Analyses were performed with Stata 12 (StataCorp LP, College Station, TX, USA).
Results
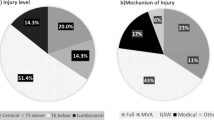
Population demographic and SCI data are provided in Table 1. Of the three persons with cervical lesions, two were classified as ASIA E (that is, sensory and motor function were normal) and one had a central cord syndrome (that is, incomplete injury; ambulatory). Thoracic injury patients included six complete paraplegics and nine patients with incomplete lesions (that is, two ASIA B, three ASIA C, three ASIA D and one ASIA E). All patients with lumbar lesions were incomplete injuries (that is, four ASIA C, two ASIA D) and the two patients with sacral lesions had conus medullaris syndrome (that is, incomplete injury; ambulatory).
Although patient-unadjusted mean pain scores gradually decreased over time, differences between the four assessment points were not significant (Figure 1).
Figure 2 shows trajectories of pain severity over measurement points for patients who reported (a) minimal difference in pain between baseline and the last measurement; (b) increased pain at the last measurement and (c) an overall decrease in pain. Most patients who reported increased pain severity showed a relatively constant increase (solid line). However, trajectories varied in patients with decreased pain; of these, two patients showed a constant reduction (dashed line), whereas five fluctuated between peak and trough (solid). Potential relationships between trajectories and therapeutic interventions or other factors were not explored.
Of the 23 patients interviewed by phone at the fourth assessment (Table 2), 22 (96%) reported either intermittent or continuous presence of pain for at least 6 months, that is, chronic pain; one denied pain. Onset of pain ranged since the time of injury to 12 months. Pain duration ranged from 41 to 53 months, averaging 48 months (s.d.: 3.8). Pain severity ranged from two to ten. Location of pain included one or both lower extremities (n=17; 77%), the back (n=3; 14%), the waist (n=2; 9%), the upper body (n=1; 4.3%), the hip (n=1; 4.3%) and the left abdomen (n=1; 4.3%). Although abdominal pain may be associated with visceral function, no relationship with food intake or related symptoms of sweating or nausea were noted in this patient.5 Most patients spontaneously described the quality of their pain as ‘numb’ (59%) or ‘burning’ (50%) and its pattern as either ‘continuous’ (10), ‘intermittent’ (9) or ‘momentary’ (3). Cold weather was reported by eight patients as aggravating their pain, whereas three implicated body posture (lengthy periods of sitting were noted by two patients). Alleviating factors included distracting activities (six patients), whereas resting and medication were each mentioned by a single patient.
Six patients (27%) were classified as having nociceptive musculoskeletal pain, three of whom also likely had an additional neuropathic component (Table 2) that is, mixed pain classification. Two of these patients reported an increase in pain severity owing to a change in body position, indicative of musculoskeletal pain;5 pain was also described by these patients (ages 40, 50; Table 2) burning and ‘shooting/numb’, respectively, suggesting neuropathic pain.5 The third patient (age 63; Table 2) used the descriptors numb, indicating neuropathic pain, and ‘distending’ (distending is understood to mean ‘zhang tong’, a Chinese term usually used to describe a dull, aching pain accompanied by a sensation of distension and likely of musculoskeletal origin). The remaining 16 patients (72%) were classified as neuropathic pain cases strictly. Thus, 19 patients had a neuropathic pain component (82%). Neuropathic pain was more common below than at the level of lesion (78 vs 26%).
ID pain-screening results indicated that neuropathic pain was very likely in nine patients, likely in eight, possible in four and unlikely in one patient.
Pain determinants
Pain severity did not significantly improve over time according to the fully adjusted Tobit regression model (Table 3). Patients with cervical lesions reported significantly less pain than those with lumbosacral lesions, whereas patients with complete lesions (ASIA A) and illiterate patients reported significantly higher pain scores (that is, about a 3-point pain scale increase compared with incomplete lesion or literate patients, respectively).
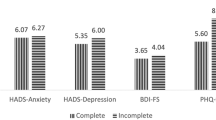
Correlations of pain with other outcomes
Depression (Patient Health Questionnaire-9) correlated strongly and significantly with pain severity at the initial baseline assessment (2009) and in 2010 but not significantly in 2012 (Table 4). Most WHOQOL domains correlated negatively with pain in 2009 and 2010. Craig Hospital Handicap Assessment and Reporting Technique domains were minimally correlated with pain except for physical independence and social function in 2010. Most correlations of pain severity with WHOQOL and Craig Hospital Handicap Assessment and Reporting Technique domains decreased at the 2012 assessment. WHOQOL environmental satisfaction showed a moderate negative correlation, however.
Pain interventions
Of the 22 patients reporting pain in the October 2012 interview, 15 (68%) had not received any treatment for pain, whereas the remaining 7 (32%) had been prescribed medications. Two patients were prescribed nonsteroidal anti-inflammatory drugs alone, one a nonsteroidal anti-inflammatory drug with an opioid and another patient an opioid (tramadol) in combination with an antidepressant (amitriptyline). Three persons could not remember the medication type or name. All patients reported taking medication as prescribed and three reported no improvement in pain symptoms. No other pain interventions including physical exercise, cognitive behavioral therapy or traditional Chinese medicine modalities were reported.
Most patients who did not seek pain treatment from a doctor either believed that pain following SCI was normal, and therefore should be tolerated without physician’s intervention (n=10), feared addiction to pain medication (n=5) or thought that pain medication would be ineffective (n=2). Bivariate analysis showed a moderate association of seeking treatment with education level (Cramer’s V=0.31; P=0.35); high school graduates sought treatment more frequently than either those in primary school or who were illiterate. No other sociodemographic variable was related to seeking treatment.
Discussion
This study is the first to longitudinally assess and characterize SCI-related pain in earthquake victims. Chronic pain was prevalent in this population as in similar populations.2 Most patients reported pain since the onset, which was described as continuous or intermittent, and occurred mostly in the lower extremities. Average pain severity did not significantly decrease over time, although some individual pain trajectories varied considerably. Neuropathic pain was more than twice as prevalent as nociceptive musculoskeletal pain compared with a non-earthquake SCI cohort in which musculoskeletal pain was the most common type of pain experienced.16 In the absence of comparative studies, this difference in findings cannot be explained as both samples are convenience samples, and therefore the relative contribution of the etiological mechanism compared with potential other factors (for example, sampling bias) is unknown.
Persons in this study with cervical lesions reported significantly less pain than those with lumbosacral lesions. This finding may be a statistical artifact, however, as only three patients had cervical lesions. Also, patients with complete lesions (ASIA A) reported significantly higher pain scores than those with incomplete lesions. Literature reporting associations of completeness and level of injury with prevalence and severity of pain is inconclusive;4 a longitudinal study of the prevalence and characteristics of pain in the first 5 years following SCI showed no relationship between the presence of pain overall and level or completeness of lesion, for example.16
Illiteracy in this cohort was associated with increased chronic pain, which has been related in a review of back pain patients to psychosocial and socioeconomic factors including impaired coping, increased susceptibility to stress and greater participation in high-risk health behaviors.17 Similarly, less educated people may more likely be affected by SCI-related chronic pain. Low education level may also correspond to low health literacy in SCI-related chronic pain patients as has been shown in patients with other chronic health conditions wherein low education level has been associated with poorer knowledge of the condition and limited self-management skills.17, 18
SCI-related chronic pain has been previously associated with depressive symptoms.19 Depression scores were highly correlated with pain at the first two assessment measurement points but not at the third assessment. Habituation to chronic pain could explain this finding, as most patients believed that pain following SCI was a normal complication. Social participation and QoL scores were also no longer associated with pain by 2012, which indirectly implies a role for habituation as well. Community-based rehabilitation measures1 over time could also have contributed to reduced impact of pain on psychosocial functioning and QoL by 2012.
Most persons did not seek physician’s treatment for their persistent pain because they either regarded it as a normal complication of SCI that could not be treated or because they feared developing drug dependency. Interview responses indicated a general lack of understanding of SCI-related pain characteristics, as well as use of medications including opioids and nonpharmacological pain management options. Half of the patients who took medication reported no improvement in pain symptoms, aligning with studies that suggest that pharmacological treatments have limited effect on pain relief in SCI.20 Nonpharmacological interventions such as physical exercise, cognitive behavioral therapy or traditional Chinese medicine techniques including acupuncture may benefit this population.18, 20, 21, 22
This study is limited by its small sample size, although the population demographics and SCI characteristics are similar to those reported in other earthquakes.2 Hospital record and patient self-report data would ideally have been confirmed by physical examination, given additional study administration personnel. Physical findings that would possibly differentiate musculoskeletal from neuropathic pain could not be obtained in the interview-based determination.
Depression, QoL and social participation were assessed in the first three measurements only, limiting the length of longitudinal assessment, and description of SCI-related pain with classification was elicited solely in the final assessment. Serial longitudinal classification could have potentially identified a relative progression of musculoskeletal and neuropathic pain types. Finally, although verbal rating scale is an acceptable alternative to VAS in the assessment of chronic pain severity and VAS and verbal rating scale scores are highly correlated, measurement bias at the final assessment cannot be excluded, as verbal rating scale scores have shown a tendency to be higher than VAS scores.23
Additional studies addressing the relationship between pain trajectories and interventions could be performed to further assess and characterize SCI-related chronic pain in earthquake victim populations. More robust evidence on the biological and psychosocial determinants of pain severity and the correlation of chronic pain with related outcomes is needed. These findings would clarify patient pain-treatment-seeking behaviors and therapeutic interventions. The roles of patient education level and depression should be emphasized and nonpharmacological pain interventions considered. Assessment of SCI-related pain in earthquake victims should begin immediately after the disaster to minimize depression and to optimize physical functional recovery, social participation and QoL. In conclusion, this initial longitudinal assessment and characterization of SCI-related pain in earthquake victims provides a foundation for further exploration of the biological and psychosocial determinants of pain severity and of the correlation of chronic pain with related outcomes in this population.
Data Archiving
There were no data to deposit.
References
Zhang X, Reinhardt JD, Gosney JE, Li J . The NHV rehabilitation services program improves long-term physical functioning in survivors of the 2008 Sichuan earthquake: a longitudinal quasi experiment. PLoS One 2013; 8: e53995.
Yongqiang Li, Reinhardt JD, Gosney JE, Zhang X, Hu X, Chen S et al. Evaluation of functional outcomes of physcial rehabilitation and medical complications in spinal cord injury victims of the Sichuan earthquake. J Rehabil Med 2012; 44: 534–540.
Loeser JD, Treede RD . The Kyoto protocol of IASP basic pain terminology. Pain 2008; 137: 473–477.
Dijkers M, Bryce T, Zanca J . Prevalence of chronic pain after traumatic spinal cord injury: a systematic review. J Rehabil Res Dev 2009; 46: 13–29.
Bryce TN, Biering-Sorensen F, Finnerup NB, Cardenas DD, Defrin R, Lundeberg T et al. International spinal cord injury pain classification: part I. Background and description. March 6-7, 2009. Spinal Cord 2012; 50: 413–417.
Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE . Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res 2008; 31: 165–169.
Leung SO, Chan CC, Shah S . Development of a Chinese version of the Modified Barthel Index— validity and reliability. Clin Rehabil 2007; 21: 912–922.
Walker N, Mellick D, Brooks CA, Whiteneck GG . Measuring participation across impairment groups using the Craig Handicap Assessment Reporting Technique. Am J Phys Med Rehabil 2003; 82: 936–941.
Jang Y, Hsieh CL, Wang YH, Wu YH . A validity study of the WHOQOL-BREF assessment in persons with traumatic spinal cord injury. Arch Phys Med Rehabil 2004; 85: 1890–1895.
Bombardier CH, Kalpakjian CZ, Graves DE, Dyer JR, Tate DG, Fann JR . Validity of the Patient Health Questionnaire-9 in assessing major depressive disorder during inpatient spinal cord injury rehabilitation. Arch Phys Med Rehabil 2012; 93: 1838–1845.
Celik EC, Erhan B, Lakse E . The clinical characteristics of neuropathic pain in patients with spinal cord injury. Spinal Cord 2012; 50: 585–589.
Widerstrom-Noga E, Biering-Sorensen F, Bryce T, Cardenas DD, Finnerup NB, Jensen MP et al. The international spinal cord injury pain basic data set. Spinal Cord 2008; 46: 818–823.
Li J, Feng Y, Han J . Linguistic adaptation into Chinese and multicentered validation of three questionnaires for the screening of neuropathic pain. Chinese J Pain Med 2011; 17: 9.
Twisk J, Rijmen F . Longitudinal tobit regression: a new approach to analyze outcome variables with floor or ceiling effects. J Clin Epidemiol 2009; 62: 953–958.
Efron B, Tibshirani R . Bootstrap methods for standard errors, confidence intervals, and other measures of statistical accuracy. Stat Sci 1986; 1: 54–75.
Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ . A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain 2003; 103: 249–257.
Dionne CE, Von Korff M, Koepsell TD, Deyo RA, Barlow WE, Checkoway H . Formal education and back pain: a review. J Epidemiol Commun Health 2001; 55: 455–468.
Heutink M, Post MW, Bongers-Janssen HM, Dijkstra CA, Snoek GJ, Spijkerman DC et al. The CONECSI trial: results of a randomized controlled trial of a multidisciplinary cognitive behavioral program for coping with chronic neuropathic pain after spinal cord injury. Pain 2012; 153: 120–128.
Hoffman JM, Bombardier CH, Graves DE, Kalpakjian CZ, Krause JS . A longitudinal study of depression from 1 to 5 years after spinal cord injury. Arch Phys Med Rehabil 2011; 92: 411–418.
Heutink M, Post MW, Wollaars MM, van Asbeck FW . Chronic spinal cord injury pain: pharmacological and non-pharmacological treatments and treatment effectiveness. Disabil Rehabil 2011; 33: 433–440.
Norrbrink C, Lindberg T, Wahman K, Bjerkefors A . Effects of an exercise programme on musculoskeletal and neuropathic pain after spinal cord injury: results from a seated double-poling ergometer study. Spinal Cord 2012; 50: 457–461.
Norrbrink C, Lundeberg T . Acupuncture and massage therapy for neuropathic pain following spinal cord injury: an exploratory study. Acupunct Med 2011; 29: 108–115.
Cork RC, Isaac I, Elsharydah A, Saleemi S, Zavisca F, Alexander L . A comparison of the verbal rating scale and the visual analog scale for pain assessment. Int J Anesthesiol 2004; 8.
Acknowledgements
We graciously thank the earthquake victims and rehabilitation volunteers who participated in this study. The outstanding work of volunteers Sijing Chen, Xiaorong Hu, Chengjie Yan and Shouguo Liu is especially acknowledged. We are also grateful for the generous support of the Caring For Children Foundation (Hong Kong), Handicap International and the Mianzhu Hospital. The work of Drs Wen and Zhang has been funded by the Caring for Children Foundation, Hong Kong, China. Dr Raouf Gharbo of the International Society of Phyical and Rehabilitation Medical Committee for Rehabilitation Disaster Relief (Physicians for Peace) is kindly acknowledged for his expert technical review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Disclaimer
This institution had at no time any influence on the analysis or interpretation of the data nor on drafting the manuscript.
Rights and permissions
About this article
Cite this article
Wen, H., Reinhardt, J., Gosney, J. et al. Spinal cord injury-related chronic pain in victims of the 2008 Sichuan earthquake: a prospective cohort study. Spinal Cord 51, 857–862 (2013). https://doi.org/10.1038/sc.2013.59
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.59