Abstract
Study designs:
Longitudinal and correlational study with repeated measures.
Objectives:
The aim of this study was to test the concurrent validity of the Berg Balance Scale (BBS) for a spinal cord injury (SCI) population.
Participants:
A total of 32 individuals with an ASIA D SCI walking 10 m independently, with or without walking assistive devices.
Setting:
An intensive rehabilitation center in Montréal, Canada.
Methods:
Subjects were evaluated on the BBS, the Walking Index for Spinal Cord Injury (WISCI II), the Spinal Cord Injury Functional Ambulation Inventory (SCI-FAI), the 10-m walk test (10MWT) and the Timed Up and Go (TUG). Individuals were reassessed during rehabilitation when progressing to a device providing less support or to unassisted gait.
Results:
All walking tests were highly correlated with the BBS (0.714<Rs<0.816, P⩽0.01). A significant ceiling effect was found on the BBS, the WISCI and on most subsections of the SCI-FAI. Assistive devices used for walking relate well to the BBS score (Spearman's ρ 0.714, P<0.01).
Conclusion:
The BBS is an appropriate assessment of standing balance for individuals with SCI. Complementary evaluation with the 10MWT or the 2MWT is recommended to supplement the ceiling effect on the BBS.
Similar content being viewed by others
Introduction
Walking is one of the most commonly listed goals by persons with a spinal cord injury (SCI).1 Far from being unrealistic, statistics show that up to one-third of all people with a new SCI will recover some walking ability at 1 year post injury.2 The initial presence of motor function is especially relevant to infer on the future ambulatory status. It has been shown that 80–100% of ASIA D patients (incomplete lesion with muscles having grade ⩾3 below the neurological lesion level3) will recover at least partial walking function a year after the initial insult.4 Therefore, implementing validated outcome measures that quantify walking and balance capacities is of primary importance to guide rehabilitation of individuals with SCI.
Various dedicated walking evaluations for the SCI population have been developed lately. The Walking Index for Spinal Cord Injury (WISCI II) and the Spinal Cord Injury Functional Ambulation Inventory (SCI-FAI) are designed to portray various features of walking function.5, 6 However, no balance assessment has been validated for this clientele, even though this dimension is crucial for a comprehensive walking and standing skills assessment.
The Berg Balance Scale (BBS) was originally developed to assess balance capacities for geriatric and stroke populations.7 Easy to implement and inexpensive, this assessment possesses satisfactory metrological properties and has been used with a wide repertoire of populations.8, 9, 10 Its universality is such that some authors use it as the gold standard for balance in criterion validity studies.11, 12 Consequently, clinicians have applied the BBS for different patients with a wide variety of conditions for which it has not been validated, such as SCI.
It has been suggested in the literature on the BBS that the score obtained may be related to some extent to the walking assistive device used in the geriatric population.13 It remains to be established whether this relationship applies to the SCI population as well. If it does, it would add support to the clinicians’ recommendations on the most appropriate walking assistive devices.
The aim of this research project, therefore, is to document the concurrent validity of the BBS with various walking parameters for an SCI population. Specifically, existing links between the use of mobility aids and the BBS score are explored. Differences between the performance of paraplegic and tetraplegic individuals in the various Berg tasks are also investigated. It is hypothesized that balance, as measured by the BBS, would be related to all walking outcome measures and be similar among tetraplegic and paraplegic individuals.
Subjects and methods
Subjects and setting
Overall, 32 subjects with SCI were recruited on a volunteer basis from the in-population of the Institut de réadaptation Gingras-Lindsay de Montréal. Inclusion criteria were as follows: (1) Adults with SCI ASIA D either of traumatic or nontraumatic etiology and (2) the ability to walk 10 m independently with or without upper-extremity assistive devices. Subjects who had other concomitant neurological conditions in addition to the SCI or who had walking difficulties before the SCI were excluded from the study. Ethics approval was obtained from the research center ethics committee. The subject's consent was obtained after he/she had read and understood the information about the research objectives and procedure.
Procedure
An experienced physical therapist conducted the assessment of all subjects in the physiotherapy department. The following evaluations were performed: BBS7, SCI-FAI6, WISCI II5, the 10-m walk test (10MWT14) and the Timed Up and Go (TUG14). Most evaluations were performed within a single session that lasted approximately 1 h. Subjects were allowed to rest 5 min between evaluations as needed. If, for time constraints or fatigue, a subject was unable to have all evaluations in one session, the latter were pursued the next day. Subjects were reassessed during their hospitalization if they could walk with an assistive device providing less support (for example, walker to a cane) or if they progressed to unassisted gait. The evaluation process ended when a patient was discharged from the facility. Overall, three subjects were reassessed once. The following data were collected for all subjects: gender, age, height, weight, type and time of injury, level of lesion, ASIA Impairment Scale and presence of any relevant associated conditions.
Outcome measures
The BBS is a clinical measure of balance consisting of 14 tasks of progressing difficulty.7 Each task is graded on a 5-point ordinal scale and then summed up to obtain a possible total score ranging from 0 to 56. Scoring is based on the ability to meet certain time or distance requirements, and to perform the items without assistance. Subjects wore their usual shoes and braces, if necessary, during testing. Assessments were conducted without the subjects’ walking assistive device.
The WISCI II is a walking assessment based on an ordinal scale comprising 21 levels.5, 15 This scale represents a gradation of walking performance based on the need for physical assistance, braces and walking aids. The maximal level at which a person was able to walk safely was recorded. The SCI-FAI is an assessment of ambulation divided into four sections devoted to the description of gait characteristics (walking parameter), use of assistive devices for the upper and lower extremities, the functional aspect of ambulation (walking mobility) and a 2-min walk test (2MWT).6 Subjects were instructed to walk at a comfortable walking speed with their usual mobility devices.
For the 10MWT, subjects were asked to walk at their normal walking speed over a distance of 15 m using their usual assistive device.14 The middle 10-m section was timed using a stopwatch. The task was performed thrice and the resulting speeds obtained were averaged. The TUG is a well-known functional walking test.14 The time needed to perform the task was recorded with a stopwatch and averaged over three trials.
Statistical analysis
All data were analyzed using SPSS statistical software (version 13.0 for Windows, SPSS Inc., Chicago, IL, USA). Descriptive statistics on patient characteristics and clinical outcomes were first collected. Normality of distribution was explored using the Kolmogorov–Smirnov test. Except for the 10MWT and the 2MWT, results were considered as having a non-normal distribution. Parametric and non-parametric tests (independent t-test, Wilcoxon's rank-sum test) were therefore performed to compare the data on the paraplegic and tetraplegic subjects. Correlations were performed on clinical data. The Pearson's product moment correlation was computed for the timed and measured walking tests (10MWT, TUG, 2MWT). Spearman's ρ coefficients were used on data from ordinal scales (BBS, WISCI, SCI-FAI). Statistical significance was accepted at a 0.05 level. The relationship between the BBS score and the assistive device was investigated with a box plot. ‘Extreme score’ was defined as a participant's score being greater than 3 interquartile ranges from the lower edge of the box.
Results
Subjects' characteristics and clinical outcomes
In total, 32 subjects (7 women and 25 men) participated in the study and completed the clinical evaluation (Tables 1 and 2). Except for the LEMS (lower-extremity motor score) (P=0.052), parametric and non-parametric tests performed on the sample revealed no significant differences between paraplegic and tetraplegic subjects (P>0.05).
Correlation analyses
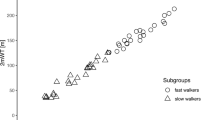
The clinical variables were significantly interrelated with coefficients ranging from moderate to high (0.609<r<0.980; Table 3 and Figure 1). Balance, as assessed by the BBS, correlated significantly well with all the different walking aspects evaluated in this study. Overall, the strongest levels of association were observed for the TUG scores (Table 3).
Assistive devices
The results showed that subjects with paraplegia and tetraplegia differed regarding the relation between their use of assistive devices and the BBS score obtained (Figure 2). For the paraplegia group, walker users (n=3; 20%) had BBS scores below 30/56, whereas those in the tetraplegia group (n=5; 29%) had a broader range of BBS scores (31–55/56). The use of two walking aids (cane, crutches) was restricted to the paraplegia group (BBS range 44–51/56; n=4). Walking with a cane or without any assistive devices was achieved with a BBS score above 50 in the paraplegia group. It ranges from 39 to 56 in the tetraplegia group. Except for two participants, walking with no assistive device (‘none’ in Figure 2) in the tetraplegia group was seen when the score in the BBS was normal (56/56).
Performance of paraplegic and tetraplegic subjects in individual BBS tasks
Visual analysis reveals a different pattern between tetraplegic and paraplegic individuals on the various Berg items (Figure 3). In particular, paraplegic subjects are more challenged than tetraplegic subjects throughout the various tasks. The mean score tends to decrease across items for paraplegics, indicating the progressive difficulty of the BBS, whereas for the tetraplegics, almost all subjects are able to execute tasks 1 to 7 (standing feet together) and then items 8–14, which start to be more challenging, with the highest difficulty corresponding to task 14 (standing on one foot).
Mean score for each 14 tasks of the Berg Balance Scale (BBS). BBS tasks: (1) sitting to standing; (2) standing unsupported; (3) sitting unsupported; (4) standing to sitting; (5) transfers; (6) standing eyes closed; (7) standing feet together; (8) reaching forward; (9) retrieving object from floor; (10) turning to look behind; (11) turning 360°; (12) placing alternate foot on stool; (13) tandem standing; and (14) standing on one foot.
Ceiling effect
A significant ceiling effect was found in the clinical evaluations. According to Mao et al.,16 a significant ceiling effect is involved when more than 20% of subjects reach the maximal score of the scale. Hence, a ceiling effect was present on the BBS (37.5%), the WISCI II (44.8%) and the different sections of the SCI-FAI (parameter: 68.8%, assistive devices: 34.4% and walking mobility: 34.4%; Table 4). The ceiling effect could likewise be observed in some scatter plots (Figure 1). These graphs also reveal that continuous clinical variables such as the 10MWT did not present a ceiling effect and thus allow to further differentiate subjects with a maximal BBS score.
Discussion
This study helps us to clarify existing links between balance as assessed by the BBS and different aspects of walking function. In light of our findings, the BBS seems an appropriate evaluation of balance for people with SCI, as shown by its strong association with the various clinical walking evaluations used in this research project. Thus, a better standing balance is closely connected to a more normal gait pattern, a higher walking speed, a lesser use of supervision or physical assistance and, therefore, a more functional walking status. In particular, the BBS is associated with walking assessments specific to SCI, such as the WISCI and the SCI-FAI. Other researchers also reported a strong association between the WISCI, the 10MWT and the BBS.17, 18 Consequently, these results tend to support the use of the BBS as a valid clinical assessment for this population.
The high correlation between the use of walking assistive devices and the BBS has its relevance. Our results tend to support the clinical intuition that an impaired balance status translates into a greater reliance on walking equipment. The use of a walker, crutches or a cane expands the base of support when standing.19 The center of gravity and the center of pressure are more easily kept within the base during gait, turning and stopping tasks, thereby improving the stability of the person with balance impairment. The BBS seems a promising tool to help determine the most appropriate assistive device for a person. Indeed, Berg et al.13 has shown that the BBS was efficient to discriminate between subjects according to their use of each type of assistive devices. Walker users tend to have a lower BBS score on average than cane users, mainly if they have paraplegia. Subjects who could walk without any assistive devices tended to have a BBS score near the maximal value. Moreover, the BBS score is related to walking without any physical assistance or supervision. In our sample, a minimal Berg score of 31/56 for tetraplegic subjects and 17/56 for paraplegic subjects was required to achieve this level. Such a difference might be explained by the relative upper and lower-extremity muscle strengths. As opposed to paraplegics, tetraplegic subjects need a higher level of lower-extremity motor function to walk independently, as compensation by weight bearing on their upper extremities is limited because of weakness. This observation is supported by a significantly higher mean LEMS for tetraplegic walker users compared with paraplegic walker users (Wilcoxon test, P=0.024). Likewise, Waters et al.20 have shown that persons with incomplete tetraplegia having various degrees of upper-extremity paralysis are often less capable of using upper-extremity assistive devices than individuals with incomplete paraplegia having normal upper-extremity functions. Our study also shows that tetraplegic subjects using a walker have a greater range of Berg scores compared with paraplegics. As tetraplegic subjects have impairments involving the upper and lower extremities, a walker may constitute the best choice for individuals with different balance abilities and hand function. A walker may also be used to compensate for the presence of spasticity interfering with lower limb function. Although this aspect was not formally evaluated in this project, previous research has shown that spasticity might be related to walking outcome.17
To our knowledge, this is the first report to relate walking assistive devices to a clinical balance assessment for an SCI population. However, owing to the limited sample size, caution must be exercised before using these results when selecting an assistive device or determining the need for physical assistance. Moreover, the range of Berg scores specific to a particular assistive device tends to overlap those of other devices. Thus, making a clear decision based only on those scores is sometimes inappropriate. Furthermore, as all recruited subjects had the ASIA D type of lesion, inferences cannot be made on subjects with other types of lesions. In fact some paraplegic subjects with a complete injury can walk with appropriate assistive devices despite limited standing balance and, hence, a low BBS score. Nonetheless, we believe that, provided these limitations are taken into account, our results may be used to help analyze and support clinical decisions about the use of assistive devices and walking independence.
Although no significant difference was found on the Berg score between paraplegic and tetraplegic subjects, a closer look at individual tasks reveals differences between their mean performances. Although most tetraplegic participants could handle adequately the first seven tasks before experiencing any difficulty, most paraplegic subjects had difficulty across a majority of the 14 items (Figure 3). This finding could also be attributed to the lower-extremity strength, as the paraplegic individuals in our sample tend to have a lower LEMS than the tetraplegic individuals (Table 1).
The presence of a ceiling effect was found in many of the evaluations used in this study. Ceiling effects limit the usefulness of an evaluation, as comparison among better functioning subjects may not be possible.16 The BBS and the WISCI present such an effect, as reported elsewhere.9, 16, 21 However, as all subjects who had a maximal score on the BBS could walk independently and without any assistive device, it remains clinically useful to infer the need of assistive devices or physical assistance. It is worth noting that a significant number of subjects with a maximal score on the Berg scale or the WISCI had a walking speed below normal or functional value.22, 23 Thus, the maximal score on these two instruments is not necessarily indicative of the normal walking function. A timed or measured walking evaluation, such as the 10MWT, would therefore be a useful adjunct to these evaluations to further characterize higher functioning individuals. No known study has reported a ceiling effect on the SCI-FAI. The gait parameter section is particularly prone to this effect. A revision of this scale would be beneficial to improve its usefulness in the clinical setting.
In conclusion, we recommend using the Berg scale with incomplete SCI to assess the balance ability of these individuals. Future studies should compare this evaluation with laboratory measures of balance to further substantiate its validity.
References
Ditunno PL, Patrick M, Stineman M, Ditunno JF . Who wants to walk? Preferences for recovery after SCI: a longitudinal and cross-sectional study. Spinal Cord 2008; 46: 500–506.
Barbeau H, Ladouceur M, Norman KE, Pepin A, Leroux A . Walking after spinal cord injury: evaluation, treatment, and functional recovery. Arch Phys Med Rehabil 1999; 80: 225–235.
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003; 26 (Suppl 1): S50–S56.
Scivoletto G, Di Donna V, Scivoletto G, Di Donna V . Prediction of walking recovery after spinal cord injury. Brain Res Bull 2009; 78: 43–51.
Dittuno PL, Dittuno Jr JF . Walking index for spinal cord injury (WISCI II): scale revision. Spinal Cord 2001; 39: 654–656.
Field-Fote EC, Fluet GG, Schafer SD, Schneider EM, Smith R, Downey PA et al. The Spinal Cord Injury Functional Ambulation Inventory (SCI-FAI). J Rehabil Med 2001; 33: 177–181.
Berg K, Wood-Dauphinee S, Williams JI, Gayton D . Measuring balance in the elderly: preliminary development of an instrument. Physiother Can 1989; 41: 304–311.
Cattaneo D, Regola A, Meotti M, Cattaneo D, Regola A, Meotti M . Validity of six balance disorders scales in persons with multiple sclerosis. Disabil Rehabil 2006; 28: 789–795.
Newstead AH, Hinman MR, Tomberlin JA, Newstead AH, Hinman MR, Tomberlin JA . Reliability of the Berg Balance Scale and balance master limits of stability tests for individuals with brain injury. J Neurol Phys Ther 2005; 29: 18–23.
Qutubuddin AA, Pegg PO, Cifu DX, Brown R, McNamee S, Carne W et al. Validating the Berg Balance Scale for patients with Parkinson's disease: a key to rehabilitation evaluation [see comment]. Arch Phys Med Rehabil 2005; 86: 789–792.
Liston RA, Brouwer BJ . Reliability and validity of measures obtained from stroke patients using the Balance Master. Arch Phys Med Rehabil 1996; 77: 425–430.
Tyson SF, DeSouza LH . Development of the Brunel Balance assessment: a new measure of balance disability post stroke. Clin Rehabil 2004; 18: 801–810.
Berg KO, Maki BE, Williams JI, Holliday PJ, Wood-Dauphinee SL . Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil 1992; 73: 1073–1080.
Lam T, Noonan VK, Eng JJ, Team SR . A systematic review of functional ambulation outcome measures in spinal cord injury. Spinal Cord 2008; 46: 246–254.
Ditunno Jr JF, Ditunno PL, Graziani V, Scivoletto G, Bernardi M, Castellano V et al. Walking index for spinal cord injury (WISCI): an international multicenter validity and reliability study. Spinal Cord 2000; 38: 234–243.
Mao HF, Hsueh IP, Tang PF, Sheu CF, Hsieh CL, Mao H-F et al. Analysis and comparison of the psychometric properties of three balance measures for stroke patients. Stroke 2002; 33: 1022–1027.
Scivoletto G, Romanelli A, Mariotti A, Marinucci D, Tamburella F, Mammone A et al. Clinical factors that affect walking level and performance in chronic spinal cord lesion patients. Spine 2008; 33: 259–264.
Ditunno Jr JF, Barbeau H, Dobkin BH, Elashoff R, Harkema S, Marino RJ et al. Validity of the walking scale for spinal cord injury and other domains of function in a multicenter clinical trial. Neurorehabil Neural Repair 2007; 21: 539–550.
Bateni H, Maki BE . Assistive devices for balance and mobility: benefits, demands, and adverse consequences. Arch Phys Med Rehabil 2005; 86: 134–145.
Waters RL, Yakura JS, Adkins RH . Gait performance after spinal cord injury. Clin Orthop 1993; 288: 87–96.
van Hedel HJ, Wirz M, Dietz V, van Hedel HJA . Standardized assessment of walking capacity after spinal cord injury: the European network approach. Neurol Res 2008; 30: 61–73.
Lapointe R, Lajoie Y, Serresse O, Barbeau H . Functional community ambulation requirements in incomplete spinal cord injured subjects. Spinal Cord 2001; 39: 327–335.
Bohannon RW . Comfortable and maximum walking speed of adults aged 20–79 years: reference values and determinants. Age Ageing 1997; 26: 15–19.
Acknowledgements
The project was supported by funding from the Ordre professionnel de la Physiothérapie du Québec and the Multidisciplinary Team on Locomotor Rehabilitation after Spinal Cord Injury and Stroke. JF Lemay holds a scholarship from Fonds de la recherche en Santé du Québec (FRSQ) and S Nadeau has a senior scientist salary from FRSQ. The authors thank Isabelle Robidoux and Catherine Dansereau for their collaboration throughout the project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lemay, JF., Nadeau, S. Standing balance assessment in ASIA D paraplegic and tetraplegic participants: concurrent validity of the Berg Balance Scale. Spinal Cord 48, 245–250 (2010). https://doi.org/10.1038/sc.2009.119
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.119
Keywords
This article is cited by
-
Development and validation of the sitting balance assessment for spinal cord injury (SitBASCI)
Spinal Cord (2022)
-
Feasibility and tolerance of a robotic postural training to improve standing in a person with ambulatory spinal cord injury
Spinal Cord Series and Cases (2021)
-
Postural control strategy after incomplete spinal cord injury: effect of sensory inputs on trunk–leg movement coordination
Journal of NeuroEngineering and Rehabilitation (2020)
-
Berg Balance Scale: inter-rater and intra-rater reliability of the Spanish version with incomplete spinal cord injured subjects
Spinal Cord Series and Cases (2020)
-
Effects of water immersion on quasi-static standing exploring center of pressure sway and trunk acceleration: a case series after incomplete spinal cord injury
Spinal Cord Series and Cases (2019)