Abstract
The severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) has changed the clinical day-to-day practice. The aim of this study was to evaluate the impact of the pandemic on patients with high-grade glioma (HGG) as well as to derive best practice recommendations. We compared a multi-institutional cohort with HGG (n = 251) from 03/2020 to 05/2020 (n = 119) to a historical cohort from 03/2019 to 05/2019 (n = 132). The endpoints were outcome (progression-free survival (PFS) and overall survival (OS)) as well as patterns of care and time intervals between treatment steps. The median OS for WHO grade 4 gliomas was 12 months in 2019 (95% Confidence Interval 9.7–14.3 months), and not reached in 2020 (p = .026). There were no other significant differences in the Kaplan–Meier estimates for OS and PFS between cohorts of 2019 and 2020, neither did stratification by WHO grade reveal any significant differences for OS, PFS or for patterns of care. The time interval between cranial magnetic resonance imaging (cMRI) and biopsy was significantly longer in 2020 cohort (11 versus 21 days, p = .031). Median follow-up was 10 months (range 0–30 months). Despite necessary disease containment policies, it is crucial to ensure that patients with HGG are treated in line with the recent guidelines and standard of care (SOC) algorithms. Therefore, we strongly suggest pursuing no changes to SOC treatment, a timely diagnosis and treatment with short time intervals between first symptoms, initial diagnosis, and treatment, as well as a guideline-based cMRI follow-up.
Similar content being viewed by others
Introduction
After 2020, when the world first faced the new severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2)1, the clinical day-to-day practice for virtually any health care provider changed severely. The rapidly rising numbers of cases with increasing admissions to the intensive care units held the health care system hostage and led to changes in patterns of care for cancer patients2. This might have an impact on the oncologic outcome of cancer patients. Patients with high-grade glioma (HGG), whose survival may be drastically reduced, are particularly vulnerable during pandemic times, when the focus of health care providers shifts to containing and treating the contagion.
Previously, Azab et al. published a first evidence-based review on the impact of SARS-CoV-2 on the management of glioma patients3. The authors found no significant difference between SARS-CoV-2 negative and positive patients concerning surgical admissions. Complications and mortality outcomes were more significant in negative than positive patients. However, the authors reported the data to be heterogeneous.
Back in May 2020, we reported first practice recommendations on the neuro-oncology management for patients with HGG during the SARS-CoV-2 pandemic4. With the knowledge at that time, we proposed scenarios in cases of a possible pandemic crisis including hypofractionated radiotherapy (RT), modified chemotherapy to minimize immunosuppression, and in some cases omission of treatment if patients tested positive for SARS-CoV-24. However, with the growing evidence best practice recommendations might look different nowadays. Therefore, the aim of this article is to evaluate the actual impact of the SARS-CoV-2 pandemic on the outcome and patterns of care for patients with HGG, as well as to derive best practice recommendations for similar future scenarios.
Material and methods
Patients
We established a multi-institutional, retrospective and anonymized database, and collected data from seven German tertiary care centers specialized in neuro-oncology (Klinikum rechts der Isar of the Technical University of Munich (TUM), University Hospital Frankfurt am Main, University Medical Center Hamburg-Eppendorf, University Hospital Bonn, University Medical Center Göttingen, University Hospital Cologne, University Medical Center Mainz). We included patients with HGG (WHO grades 3 and 4) treated or diagnosed between March 2020 and May 2020, which comprised the primary study group. A historical control group was accrued from the corresponding period in 2019. The institutional review board of the Technical University of Munich (TUM) approved the study (No. 676/20 S). We performed this analysis in compliance with the principles of the Declaration of Helsinki and its latter amendments5. The need for informed consent was waived under the Bavarian Hospital Law (Bayerisches Krankhausgesetz Art. 27 Abs. 4) due to the study’s retrospective and anonymous design. The study is part of the egePan Unimed consortium which is funded by the Bundesministerium für Bildung und Forschung (BMBF) with the identifier 01KX2021. All data were anonymized before transferal between centers and storage. Only study personnel received access to data.
Endpoints
The primary endpoints were the estimations of overall survival (OS) and progression-free survival (PFS). Secondary endpoints were OS and PFS at 6 and 12 months. Further, we exploratively evaluated the impact of the SARS-CoV-2 pandemic on the patterns of care (e.g. time intervals between treatment steps).
Statistical analysis
The patient cohorts were compared by Kaplan–Meier estimators of OS and PFS with log rank testing for statistically significant differences. The predetermined times of 6 and 12 months for both OS and PFS were analyzed by z-tests. Student’s t-tests were used to compare metric baseline parameters.
All other statistical analyses were performed descriptively with exploratory intention using proportions, means, medians, and 95%-confidence intervals (95%CI). All statistical analyses were performed with SPSS version 28 (IBM, Armonk, USA). A p value of less than 0.05 was defined as statistically significant.
Results
Over 7 German university hospitals, 251 patients with a median age of 61 years (range 18–88 years) were included. 119 patients were treated in 2020, while 132 patients were treated in 2019. Patient characteristics are depicted in Table 1. In 2019, data on follow-up was available for 80% of grade 3 gliomas after 12 months, and in 2020 for 87.5% after 12 months. For grade 4 gliomas, 86.9% of the follow-up data were available after 12 months in 2019, and 78.6% in 2020. Two patients (1.7%) with grade 4 gliomas in the 2020 cohort tested positive for SARS-CoV-2 during the follow-up regimen, although without any impact on scheduling.
Oncological outcome
We evaluated the OS and PFS at 6 and 12 months for patients with WHO grade 3 (see Table 2), WHO grade 4 (see Table 3), and the entire study population (see Table 4). There were no statistically significant differences in PFS at 6 or 12 months between treatment years for the entire study population with WHO grade 3 and 4 tumors. Likewise, neither did stratification by WHO grade 3 or 4 result in significant differences for any of the parameters (Tables 2 and 3).
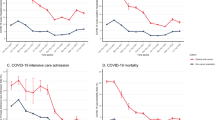
The Kaplan–Meier survival analyses did not exhibit any statistically significant difference in OS for WHO 3 gliomas between 2019 and 2020 (log rank; p = 0.291; see Fig. 1A). The median OS for WHO grade 4 gliomas was 12 months (95%CI 9.7–14.3 months) in 2019, and not reached in 2020 (log rank; p = 0.026; see Fig. 1B). The estimated PFS did not differ for either WHO grade 3 (log rank; p = 0.097; see Fig. 2A) or 4 gliomas (log rank; p = 0.070; see Fig. 2B).
Kaplan–Meier estimator for progression-free survival (PFS) compared between the 2019 and 2020 cohorts with WHO Grade 3 (A) and WHO Grade 4 (B) gliomas. Pts.—patients; SE—standard error; 95%CI—95% confidence interval. Kaplan–Meier statistics not conducted for WHO 3 due to censoring of all 2019 cases.
Patterns of care
We further evaluated the patterns of care for patients in 2020 versus 2019. Table 5 shows a comparison of the procedures performed. There was no significant difference in the distribution between years for any of the treatment modalities.
Table 6 presents the time intervals between the treatment steps. The time interval between initial cMRI and biopsy was significantly longer for patients in the 2020 cohort (Student’s t-test; p = 0.031). All other time intervals showed no significant difference.
Discussion
The diagnostics and patterns of care for HGGs rely not only on the intricate interdisciplinary cooperation within the infrastructure of a tertiary care center6,7,8. Patients are also dependent on timely referrals by the out-patient sectors of health care systems, necessitating well-organized communication and scheduling structures to ensure early histological diagnosis and rapid initiation of adjunct treatment regimens9. Our data demonstrated that when patients entered care at specialized centers, timely surgery and radiation were offered and no delay in treatment was observed.
Delays within these tried and tested frameworks may result in a subpar oncological outcome, although there are conflicting verdicts on this in the few studies published9,10,11,12,13. In our study, it was of prime interest to assess this possible collateral damage of the SARS-CoV-2 pandemic by comparing a cohort within the supposedly most critical period of the pandemic during early 2020 with a historical control. Within the confines of this study, we are able to report that with the exception of the OS for grade 4 tumors, no significant decline in oncological outcome was observed. Seeing as all tumor characteristics, GTR rates and treatment strategies did not differ between these cohorts, this difference in OS may be accounted for by the fact that the historical group had significantly longer and more consistent follow-up available, which is mirrored in the Kaplan–Meier estimation. There were no other statistical differences in oncological outcome. However, the time between cMRI and biopsy was significantly longer in patients in 2020, which might indicate a delayed patient referral to the tertiary care centers.
Our gross tumor resection (GTR) rates, OS and PFS estimates are congruent with contemporary pre-pandemic data14. In a recent pooled meta-analysis of 19 studies, Gandhi et al. found the OS ranging between 10 to 22 months and the PFS between 5 to 11 months15.
Patient management and referral processes are inevitably strained by the disease-containment measures, which in turn require a different approach to triage for the handling of routine and emergency health care services. While several scientific efforts have been made to define routines that accommodate disease-containment measures with entity-specific guidelines, it is imperative for any tertiary care provider to establish a patient management framework tailored to regional public health policies as well as the current SARS-CoV-2 load16,17,18,19,20.
Our assumption holds true that integrating disease containment policies without delaying neurooncological schedules is feasible and mainly a product of organizational processes. However, some degree of collateral damage may be inevitable. One must note that an essential component of guideline-conform diagnostic and treatment regimens strongly depend on patient compliance, which is substantially influenced by the perception of the perceived threat of an infection with the SARS-CoV-2 pathogen. This remains a largely unstudied element, and it is difficult to gauge the extent of a possible deficit in oncological outcome for lack of quality data.
What can be gleaned from this pandemic for future similar scenarios? We strongly advocate to not altering the standard of care (SOC) paradigms of both primary and tertiary health care providers. Various articles report on a reduced outcome when patients were treated without maximal resection21, without radio(chemo)therapy22,23, without adjuvant chemotherapy22, or without maintenance therapy with tumor treating fields24. From the start, patients with HGG are vulnerable patients with reduced oncological outcome. Therefore, one should not deprive those patients of their right for treatment and the best possible outcome.
Further, a timely diagnosis and short time intervals between treatment steps are of essence. We found a significantly longer time interval between initial cMRI and biopsy during 2020. It is possible that due to the low number of cases with biopsy, the effect on the outcome might not be significant. However, it is clear that such delays during all treatment steps should be strictly avoided. Previously, Aggarwal et al. showed that patients with HGG paradoxically had a significantly worse OS when they were diagnosed earlier12. However, the authors compared patients with earlier diagnosis who were admitted to the hospital presenting as emergencies compared to patients with delayed diagnosis who were referred as outpatients. For delayed surgery, Flanigan et al. showed that a longer wait time to surgery was associated with a worse OS in glioblastoma patients presenting with seizures only25. Although there are conflicting data concerning delays between surgery and radiochemotherapy, Buszek et al. recently showed that glioblastoma patients with GTR and a postponement of > 8 weeks exhibit a worse OS26.
Therefore, we recommend a timely diagnosis and treatment with short time intervals between first symptoms, initial diagnosis, and treatment. To accomplish that and not jeopardize patient care, established hygiene standards and prevention interventions are extremely important. Ngandu et al. showed in their scoping review that with non-pharmaceutical prevention interventions it was possible to avoid hospital-acquired SARS-CoV-2 infections completely or in large part27.
Therefore, the actions taken against the pandemic remain a key factor for the fight against SARS-CoV-2, however, the measures should not lead to a delayed treatment of cancer patients, specifically patients with HGG.
The available cMRI follow-up was not significantly different in both groups, with 59.8% in 2019 versus only 52.9% in 2020. There is no existing evaluation of the effectiveness of the clinically used imaging schedules for the follow-up of patients with HGG28. However, we believe that a close monitoring with cMRI as described in most clinical guidelines29,30 is desirable, particularly in a pandemic scenario. Therefore, we suggest to closely follow patients with cMRI according to established guidelines. Follow-up of patients with HGG should not be neglected during a pandemic and this adherence to follow-up consultations must remain at high priority without violating the disease containment measures during a pandemic.
In concordance with our recent consensus paper4, we may collate the following best practice recommendations for the neuro-oncological management of patients with HGG during a global pandemic scenario in Table 7.
As it is natural with retrospective observations, our study has limitations. The median follow-up is relatively short, and a future analysis with longer follow-up is planned. Due to the shorter follow-up in the cohort of 2020, we opted to additionally calculate binary outcome analyses (PFS and OS at 6 and 12 months). It is crucial to understand that various other confounders may factor into the outcome deficit; despite similar treatment regimens, patients may avoid consultations for fear of contracting the virus, reschedule interventions, treatment, or follow-up consultations.
Conclusion
The current pandemic demonstrated that patients with HGG are particularly vulnerable in these times. In our retrospective analysis, the Kaplan–Meier survival analyses did not exhibit any statistically significant differences in OS for WHO 3 gliomas between 2019 and 2020 (p = 0.291). The median OS for WHO grade 4 gliomas was 12 months (95%CI 9.7–1.43 months) in 2019, and not reached in 2020 (p = 0.026). The estimated PFS did not differ for either WHO grade 3 (p = 0.097) or 4 gliomas (p = 0.070). Therefore, it is essential to ensure that these patients’ treatment complies with the recent guidelines and SOC algorithms. Measures must be taken that even in times were resources need to be allocated such as during a pandemic, oncologic patient care is secured. It is important to note that some governmental disease containment policies may result in collateral damage to those in need of regular health care, which holds especially true for HGG patients when patient referrals and follow-up schedules are not secured. In summary, we suggest applying no changes to SOC treatment and pursuing short time intervals between first symptoms, initial diagnosis, therapeutic strategies, as well as cMRI follow-up according to established guidelines.
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
References
Wu, F. et al. A new coronavirus associated with human respiratory disease in China. Nature 579, 265–269. https://doi.org/10.1038/s41586-020-2008-3 (2020).
Dhada, S., Stewart, D., Cheema, E., Hadi, M. A. & Paudyal, V. Cancer services during the COVID-19 pandemic: systematic review of patient’s and Caregiver’s experiences. Cancer Manag. Res. 13, 5875–5887. https://doi.org/10.2147/cmar.S318115 (2021).
Azab, M. A. & Azzam, A. Y. Impact of COVID-19 pandemic on the management of glioma patients around the world. An evidence-based review. Brain Disord. 2, 100012–100012. https://doi.org/10.1016/j.dscb.2021.100012 (2021).
Bernhardt, D. et al. Neuro-oncology management during the COVID-19 pandemic with a focus on WHO Grade III and IV Gliomas. Neuro. Oncol. https://doi.org/10.1093/neuonc/noaa113 (2020).
World Medical Association Declaration of Helsinki. ethical principles for medical research involving human subjects. J. Am. Coll. Dent. 81, 14–18 (2014).
Weller, M. et al. EANO guideline for the diagnosis and treatment of anaplastic gliomas and glioblastoma. Lancet Oncol 15, e395-403. https://doi.org/10.1016/s1470-2045(14)70011-7 (2014).
Wick, W. & al., e. Gliome, S2k-Leitlinie, < www.dgn.org/leitlinien > (2021).
Weller, M. et al. EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood. Nat. Rev. Clin. Oncol. 18, 170–186. https://doi.org/10.1038/s41571-020-00447-z (2021).
Warren, K. T. et al. Time to treatment initiation and outcomes in high-grade glioma patients in rehabilitation: a retrospective cohort study. CNS Oncol. 9, Cns64, doi:https://doi.org/10.2217/cns-2020-0018 (2020).
Potharaju, M., Mathavan, A., Mangaleswaran, B., Ghosh, S. & John, R. Delay in adjuvant chemoradiation impacts survival outcome in glioblastoma multiforme patients. Acta Oncol. (Stockholm, Sweden) 59, 320–323. https://doi.org/10.1080/0284186x.2019.1672893 (2020).
Ahn, S., Park, J. S., Song, J. H., Jeun, S. S. & Hong, Y. K. Effect of a time delay for concomitant chemoradiation after surgery for newly diagnosed glioblastoma: a single-institution study with subgroup analysis according to the extent of tumor resection. World Neurosurg. 133, e640–e645. https://doi.org/10.1016/j.wneu.2019.09.122 (2020).
Aggarwal, A. et al. Diagnostic delay and survival in high-grade gliomas - evidence of the “waiting time paradox”?. Br. J. Neurosurg. 29, 520–523. https://doi.org/10.3109/02688697.2015.1012050 (2015).
Kosmin, M. et al. The impact of route of diagnosis on survival in patients with glioblastoma. Br. J. Neurosurg. 32, 628–630. https://doi.org/10.1080/02688697.2018.1436693 (2018).
Marra, J. S. et al. Survival after radiation therapy for high-grade glioma. Rep. Pract. Oncol. Radiother. 24, 35–40. https://doi.org/10.1016/j.rpor.2018.09.003 (2019).
Gandhi, S. et al. Survival outcomes among patients with high-grade glioma treated with 5-aminolevulinic acid–guided surgery: a systematic review and meta-analysis. Front. Oncol. https://doi.org/10.3389/fonc.2019.00620 (2019).
Zimmermann, M. & Nkenke, E. Approaches to the management of patients in oral and maxillofacial surgery during COVID-19 pandemic. J. Cranio-Max.-Fac. Surg. 48, 521–526. https://doi.org/10.1016/j.jcms.2020.03.011 (2020).
Stensland, K. D. et al. Considerations in the triage of urologic surgeries during the COVID-19 pandemic. Eur. Urol. 77, 663–666. https://doi.org/10.1016/j.eururo.2020.03.027 (2020).
Moletta, L. et al. International guidelines and recommendations for surgery during Covid-19 pandemic: a systematic review. Int. J. Surg. (Lond., Engl.) 79, 180–188. https://doi.org/10.1016/j.ijsu.2020.05.061 (2020).
Fligor, S. C. et al. Gastrointestinal malignancies and the COVID-19 pandemic: evidence-based triage to surgery. J. Gastrointest. Surg. 24, 2357–2373. https://doi.org/10.1007/s11605-020-04712-5 (2020).
Cohen, S. P. et al. Pain management best practices from multispecialty organizations during the COVID-19 pandemic and public health crises. Pain Med 21, 1331–1346. https://doi.org/10.1093/pm/pnaa127 (2020).
McGirt, M. J. et al. Independent association of extent of resection with survival in patients with malignant brain astrocytoma. J. Neurosurg. 110, 156–162. https://doi.org/10.3171/2008.4.17536 (2009).
Stupp, R. et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10, 459–466. https://doi.org/10.1016/s1470-2045(09)70025-7 (2009).
Laperriere, N., Zuraw, L. & Cairncross, G. Radiotherapy for newly diagnosed malignant glioma in adults: a systematic review. Radiother. Oncol. 64, 259–273. https://doi.org/10.1016/s0167-8140(02)00078-6 (2002).
Stupp, R. et al. Maintenance therapy with tumor-treating fields plus temozolomide vs temozolomide alone for glioblastoma: a randomized clinical trial. JAMA 314, 2535–2543. https://doi.org/10.1001/jama.2015.16669 (2015).
Flanigan, P. M. et al. Improved survival with decreased wait time to surgery in glioblastoma patients presenting with seizure. Neurosurgery 81, 824–833. https://doi.org/10.1093/neuros/nyx084 (2017).
Buszek, S. M. et al. Optimal timing of radiotherapy following gross total or subtotal resection of glioblastoma: a real-world assessment using the national cancer database. Sci. Rep. 10, 4926. https://doi.org/10.1038/s41598-020-61701-z (2020).
Ngandu, N. K. et al. Hospital acquired COVID-19 infections amongst patients before the rollout of COVID-19 vaccinations, a scoping review. BMC Infect. Dis. 22, 140. https://doi.org/10.1186/s12879-022-07128-5 (2022).
Thompson, G., Lawrie, T. A., Kernohan, A., Jenkinson, M. D. Interval brain imaging for adults with cerebral glioma. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD013137.pub2 (2019).
National Comprehensive Cancer Network. Central Nervous System Cancers (Version 2.2021), https://www.nccn.org/professionals/physician_gls/pdf/cns.pdf (2021).
Weller, M. et al. European Association for Neuro-Oncology (EANO) guideline on the diagnosis and treatment of adult astrocytic and oligodendroglial gliomas. Lancet Oncol. 18, e315–e329. https://doi.org/10.1016/s1470-2045(17)30194-8 (2017).
Funding
Open Access funding enabled and organized by Projekt DEAL. The study is part of the egePan Unimed consortium which is funded by the Bundesministerium für Bildung und Forschung (BMBF) with the identifier 01KX2021.
Author information
Authors and Affiliations
Contributions
The initial concept of the study was developed by SEC, JG and BM. The data was acquired by MMEV, AW, HK, TZ, RD, MV, CN, TA, and DM. The statistical analysis was performed by AW. The first draft of the manuscript was written by MMEV and AW and was revised by SEC, BM, JG, as well as all other authors. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Ulrich Herrlinger has received lecture and/or advisory board honoraria from Medac, Bayer, Janssen, and Karyopharm. All other authors declare no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vogel, M.M.E., Wagner, A., Gempt, J. et al. Impact of the SARS-CoV-2 pandemic on the survival of patients with high-grade glioma and best practice recommendations. Sci Rep 13, 2766 (2023). https://doi.org/10.1038/s41598-023-29790-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-29790-8
This article is cited by
-
Tumor size, treatment patterns, and survival in neuro-oncology patients before and during the COVID-19 pandemic
Neurosurgical Review (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.