Abstract
Three-dimensional exoscopes have been designed to overcome certain insufficiencies of operative microscopes. We aimed to explore the clinical use in various spinal surgeries. We performed surgery on patients with different spine entities in a neurosurgical department according to the current standard operating procedures over a 4-week period of time. The microsurgical part has been performed with Aesculap AEOS 3D microscope. Three neurosurgeons with different degree of surgical expertise completed a questionnaire with 43 items based on intraoperative handling and feasibility after the procedures. We collected and analyzed data from seventeen patients (35% male/65% female) with a median age of 70 years [CI 47–86] and median BMI of 25.8 kg/m2 [range 21–33]. We included a variety of spinal pathologies (10 degenerative, 4 tumor and 3 infectious cases) with different level of complexity. Regarding setup conflicts we observed issues with adjustment of the monitor position or while using additional equipment (e.g. fluoroscopy in fusion surgery) (p = 0.007/p = 0.001). However image resolution and sharpness as well as 3D-depth perception were completely satisfactory for all surgeons in all procedures. The utilization of the exoscopic arm was easy for 76.5% of the surgeons, and all of them declared a significant improvement of the surgical corridor. The 3D-exoscope implementation appears to achieve very satisfactory results in spinal procedures especially with minimally invasive approaches.
Similar content being viewed by others
Introduction
Since the introduction of operative microscopes (OMs) in modern microsurgery by Caspar and Yasargil in 1977, there has been a relentless effort to improve visualization, magnification, illumination and ergonomics for the surgeon. Recent studies have criticized limited movement and maneuverability of conventional OMs due to heavy hydraulic counterbalance systems1,2. Frequent need for repositioning and fatigue resulting from enforced fixation of the surgeon’s eyes to the OM eyepieces, as well as the limited visualization only for the operating and assisting surgeons, have been pointed out as major shortcomings2. In contrast, modern exoscopes have been designed to overcome those disadvantages and, in previous studies, were demonstrated to have comparable three-dimensional visualization with superior ergonomics and enhanced field of view, allowing for even better positioning of surgical instruments2,3,4. In a current review of the usage of exoscopes in neurosurgery, Montemurro et al. describe the current exoscopic systems on the market—VITOM® (Karl Storz, Tuttlingen, Germany), ORBEYETM (Olympus, Tokyo, Japan), Modus VTM (Synaptive Medical, Toronto, ON, Canada), Kinevo 900 (Carl Zeiss Meditec AG, Jena, Germany), BrainPath® (Nico Corporation, Indianapolis, IN, US) and Aeos® (Aesculap, Tüttlingen, Germany)5. The authors postulate that those systems provide a more convenient, high-resolution visualization without compromising the surgical corridor. Some modern features include the lock-on-target and waypoints together with the footswitch which enables to place the camera and to return to saved targets of interest, even hands-free. These functions together with the mostly horizontal visual axis of the surgeon and assistant fixed on the monitors during surgery allow for more ergonomic posture and integration of the whole OR staff during the procedure6,7. Also the possibility of 3D vision for all OR staff members enables the utilization for education purposes8,9. The implementation of the novel Aeos three-dimensional (3D) robotic digital microscope (Aesculap, Tüttlingen, Germany) has been previously displayed in the clinical and experimental setting3,10,11. We aimed to investigate the overall use and application in spinal procedures.
Methods
Ethics approval
The local ethics committee of Ludwig-Maximilians university approved the study protocol in accordance with the Declaration of Helsinki (local ethics nr. 22-0101).
Study design
We performed a prospective observational analysis of patient- and procedure-specific clinical data and questionnaires consisting of 43 items using a 5- to 7-point Likert scale (Table 1), which have been previously described3,12. Three neurosurgeons with different levels of surgical experience and skills (A = spine professional; B = consultant; and C = resident with an average of 9 years [CI 6–13] of professional experience) were formerly introduced to the Aeos robotic digital microscope by the manufacturer prior to first use and were advised to perform all spine procedures with the system of interest between October 1–31, 2021. Following each procedure the surgeons completed questionnaires, which contained information on the intraoperative satisfaction in terms of image quality, ergonomics, usability and fatigue. All data was collected, encrypted, processed and analyzed according to the study protocol.
Patient selection
All patients older than 18 years old who were undergoing a spinal procedure with the Aeos exoscope regardless of spine pathology were enrolled. Procedure-related information, such as patient positioning, operation/anesthesia time (OT/AT), blood loss (BL) and complications, were obtained.
Statistics
Statistical analysis was performed using the software SPSS Statistics™ (version 28, IBM Corp, Armonk, New York, USA). Descriptive statistics were performed for the clinical parameters and the questionnaire items data. Normal distribution was assumed according to the central limit theorem. In categorical variables, a Levene test for independent samples and a Chi-squared-test was used to compare two samples. Data in text and graphs are shown as mean standard deviation (SD). A p value ≤ 0.05 was considered significant.
Ethical approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Ludwig Maximilian University (LMU) (project Nr. 22-0101). We retrospectively analyzed prospectively collected data from a patients cohort treated at our clinics with the AEOS exoscope. Based on the retrospective character, informed consent was waived by the local ethics committee of LMU (Prof. Dr. R. M. Huber).
Results
Study population and surgical procedures
Seventeen patients (35% male/65% female) with a mean age of 68.8 years [CI 47–86] and mean BMI of 25.8 kg/m2 [CI 21–33] were included in the final analysis. The indications varied for 10 degenerative (59%), 4 tumor (23%) and 3 infectious (18%) cases with different levels of complexity according to the German Spine Society Score (GSSS) (Table 2; Fig. 1). We performed 6 lumbar decompressions with or without discectomy, 3 anterior cervical discectomies with fusion, 4 thoracolumbar corpectomies via minithoracotomy or retroperitoneal approach, 3 cervical total disc replacements and 1 tumor resection via anterior lumbar approach. Based on the GSSS, there was a balanced case complexity distribution with 35% basic (Score 1), 35% moderate (Score 3) and 30% advanced (Score 6) procedures. Although Surgeon A performed more cases (52%) and higher complexity cases (41%), there was no significant difference considering the overall case complexity distribution (p = 0.29) (Fig. 2).
Outcome and adverse events
Mean OT was 102 min [CI 59–186], and mean AT was 163 min [CI 105–319]. Mean BL was 491 ml [CI 100–3000 ml], with 47% of all cases not exceeding a BL of 200 ml. Higher BL (mean 1200 ml) was especially observed in tumor surgery (24%) but without statistical significance (p = 0.22) due to inhomogeneous distribution based on diagnosis. Only 1 patient (6%) experienced a complication due to a significant BL (3000 ml), which occurred during a L2 corpectomy indicated for vertebral metastasis of renal cell carcinoma origin, although a preoperative embolization had been performed. The vertebrectomy has been aborted after vertebral body resection due to critical hypotension, and the patient has been packed and transferred to ICU. An uneventful second look surgery with permanent implant insertion was successfully performed 7 days later. In terms of BMI, there was no statistical correlation to a higher blood loss (p = 0.43) or prolonged surgical times (p = 0.59) (Figs. 3, 4). No neurological deterioration and no system specific complications were observed during the procedures.
Questionnaire evaluation
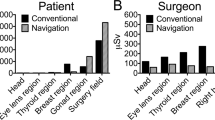
Setup management
In all procedures, surgeons either strongly (47%) or at least agreed (53%) that the surgical zone remained unblocked during surgeries (Figs. 5, 9). In 76% of all cases, the endoscopic arm was easy to control, and only 1 case appeared to be particularly challenging. Setup conflicts occurred in 12% of procedures, which we observed during surgeries in the lateral position, as both the fluoroscope and the exoscope were installed from the opposite site of the surgeon and assistant and had to be adjusted in order to obtain satisfying imaging. We further characterized the recommended OR setup for cervical and thoracolumbar procedures based on the patient and equipment positioning (Fig. 6). Solely the positioning for transthoracic and retroperitoneal approaches used to be more complicated due to the need of frequent fluoscopic control of the spine level and implants. This was particularly difficult as the exoscope and C-Arm gantry were installed on the same side anterior to the patient’s body. Therefore we used the exoscope for the opening, marked the exact position and removed it while installing the retractor and performing the discectomy and contralateral release. Afterwards we placed it once again in the same position for the vertebrectomy and removed it when the cage was in situ. The permanent cage expansion was performed under fluoscopic control and direct visualization. Even if it appeared to be challenging with a mean time prolongation of 34 min [CI 25; 43] in the first 2 cases, we did not abort the use of the exoscope and performed all surgeries without additional OM application. All surgeons agreed that surgical ergonomics during utilization was maintained, but surgical hand–eye coordination was affected in only 11% of all cases. The 3D image quality perception was defined as the perception of the particular surgeon for surgical depth and 3D image quality during the application of the 3D goggles and the exoscopic system. All participants felt that 3D image quality perception was satisfactory in all cases (Fig. 9). Eyestrain was evaluated based on the subjective perception of the surgeon during the use of the 3D goggles and did not occur in all cases. Surgeons stated that switching between different targets of view through the robotic arm’s automatic movement and focus adjustment was highly beneficial throughout complex multilevel procedures (Figs. 7 and 8 Exemplary cases, Fig. 9).
Exemplary case 1: anterior cervical discectomy and disc replacement or fusion. (A) Anterior discectomy and removal of the anterior longitudinal ligament; (B) Cervical disc replacement with prosthesis; (C) Cervical foraminotomy; (D) Saving two different targets of focus enables semi-automatic adjustment between the two levels of interest
Exemplary case 2: thoracic corpectomy and vertebral body replacement with a carbon fiber-reinforced PEEK implant for metastatic disease. (A) Transpleural minithoracotomy approach for vertebral body resection; (B) Vizualization of vertebral body replacement; (C) Providing different angles of view in the depth enables adequate preparation and hemostasis; (D) Watertight closure of pleural cavity after chest tube placement
Satisfaction
All surgeons rated the surgical satisfaction in 88% of all cases as high (41%) or very high (47%). In the remaining 12%, it was slightly above expectations. In 17.6% of all cases, surgeon’s frustration was above expectations, which was independent from the case complexity based on the GSSS scores (p = 0.34) and the surgeon’s experience (p = 0.16). We performed an ANOVA test to investigate the influence of further parameters e.g. surgical times, blood loss, spine level, age and BMI and could not identify a significant dependency for the level of frustration based on these values (Table 3). Mental and physical demands were below average in 82% and 76% of all cases, respectively. In only one case, surgeons indicated an above average level of demand, which was the previously mentioned vertebrectomy case for metastatic disease.
Limitations
In this study, we collected limited data in a single institution based on a short time application of a novel 3D exoscope. A higher number of treated patients and a comparative cohort treated with OM would have enabled a randomization and probably more significant results. Long-term follow-up data turns out to be missing in this study particularly considering implant subsidence and tumor or infection recurrence. However, we demonstrated highly satisfying results in several minimally invasive keyhole spine approaches independent from the surgeon’s experience when using the 3D exoscope.
Discussion
All procedures in this study were performed entirely with the AEOS exoscope, and there was no case in which surgeons switched to the OM due to case complexity. Although surgeons in our institution were only briefly instructed in the utilization of the new exoscope system, they quickly felt comfortable and confident using it even in complex procedures. The Aeos exoscope generates unobstructed access, allowing abundant space to insert and use even longer surgical instruments, which appears to be highly beneficial especially in minimally invasive lateral spine surgery. Giorgi et al. demonstrated in a series of patients with thoracolumbar fractures with spinal cord compression a crucial improvement of the user-friendliness and visualization in lateral thoracolumbar procedures through the possibility to simply shift between microscopic and macroscopic vision without moving the exoscope and without blocking the deep surgical field13. Although we experienced some surgical time prolongation in the first two lateral cases, we quickly established an OR setup for all spine procedures based on the patient positioning, which diminished the setup conflicts and allowed a better positioning of the C-Arm.The exoscopic systems already demonstrated satisfying magnification and stereoscopic vision even in more challenging and extensive deformity correction procedures14. Still the major advantages, which we also observed in our study, are the improvement of 3D depth perception and magnification in minimally invasive procedures like the classical anterior cervical approach and the lateral thoracolumbar minithoracotomy or the retroperitoneal approach. Yao et al. even demonstrated shorter surgical times and fewer complications in anterior cervical discectomies with fusion due to more adequate ipsi- and contralateral decompression with reduced time of focusing and higher maneuverability and ergonomics15. Also the exoscope facilitates a long working distance, which allows surgeons to perform bimanually with standard instruments without conflict with the camera and the use of additional monitor makes it possible for all participants to be better integrated in the procedure15. Surgeons in our study confirmed that the robotic arm allowed better control with superior ergonomics and less fatigue compared to the OM. The ergonomics and feasibility were rated high, which correlates with the experience in previous studies3,4,12. Taking into consideration the data from earlier publications, we believe that the frequent use of an exoscope might prevent the development of neck and back pain for surgeons in long-lasting procedures due to a unnatural bending posture2,3,4,15. The combination of augmented reality for complex tumor or degenerative cases might be of further interest and was not explored during this study. Additionally, the application of different filters might also be helpful in tumor cases and should be further explored.
Conclusion
The 3D Aeos exoscope facilitates high quality visualization and three-dimensional depth perception in minimally invasive spinal procedures.
Data availability
The data presented in this study are available on request from the corresponding author.
References
Amoo, M., Henry, J. & Javadpour, M. Beyond magnification and illumination: Preliminary clinical experience with the 4K 3D ORBEYE exoscope and a literature review. Acta Neurochir. (Wien) 163(8), 2107–2115. https://doi.org/10.1007/s00701-021-04838-8 (2021).
Siller, S. et al. A high-definition 3D exoscope as an alternative to the operating microscope in spinal microsurgery. J. Neurosurg. Spine https://doi.org/10.3171/2020.4.SPINE20374 (2020).
Maurer, S. et al. Evaluation of a novel three-dimensional robotic digital microscope (aeos) in neurosurgery. Cancers (Basel) https://doi.org/10.3390/cancers13174273 (2021).
Muhammad, S., Lehecka, M. & Niemela, M. Preliminary experience with a digital robotic exoscope in cranial and spinal surgery: A review of the Synaptive Modus V system. Acta Neurochir. (Wien) 161(10), 2175–2180. https://doi.org/10.1007/s00701-019-03953-x (2019).
Montemurro, N. et al. The exoscope in neurosurgery: An overview of the current literature of intraoperative use in brain and spine surgery. J. Clin. Med. https://doi.org/10.3390/jcm11010223 (2021).
Abramovic, A. et al. Surgeon’s comfort: The ergonomics of a robotic exoscope using a head-mounted display. Brain Spine 2, 100855. https://doi.org/10.1016/j.bas.2021.100855 (2022).
Oertel, J. M. & Burkhardt, B. W. Vitom-3D for exoscopic neurosurgery: Initial experience in cranial and spinal procedures. World Neurosurg. 105, 153–162. https://doi.org/10.1016/j.wneu.2017.05.109 (2017).
Kwan, K. et al. Lessons learned using a high-definition 3-dimensional exoscope for spinal surgery. Oper. Neurosurg. (Hagerstown) 16(5), 619–625. https://doi.org/10.1093/ons/opy196 (2019).
Moisi, M. D. et al. Advancement of surgical visualization methods: Comparison study between traditional microscopic surgery and a novel robotic optoelectronic visualization tool for spinal surgery. World Neurosurg. 98, 273–277. https://doi.org/10.1016/j.wneu.2016.11.003 (2017).
Hafez, A. et al. Comparison of operating microscope and exoscope in a highly challenging experimental setting. World Neurosurg. 147, e468–e475. https://doi.org/10.1016/j.wneu.2020.12.093 (2021).
Herlan, S. et al. 3D exoscope system in neurosurgery-comparison of a standard operating microscope with a new 3D exoscope in the cadaver lab. Oper. Neurosurg. (Hagerstown) 17(5), 518–524. https://doi.org/10.1093/ons/opz081 (2019).
Rosler, J. et al. Clinical implementation of a 3D4K-exoscope (Orbeye) in microneurosurgery. Neurosurg. Rev. https://doi.org/10.1007/s10143-021-01577-3 (2021).
Giorgi, P. D. et al. Spinal cord compression in thoracolumbar burst fractures: Application of high-definition three-dimensional exoscope in minimally invasive lateral surgery. Eur. J. Orthop. Surg. Traumatol. https://doi.org/10.1007/s00590-022-03319-7 (2022).
Rechav Ben-Natan, A. et al. Use of an exoscope for enhanced visualization of a Schwab grade 5 osteotomy to correct kyphotic deformity. Neurosurg. Focus Video 6(1), V19. https://doi.org/10.3171/2021.10.FOCVID21190 (2022).
Yao, Y. et al. Three-dimensional high-definition exoscope (Kestrel View II) in anterior cervical discectomy and fusion: a valid alternative to operative microscope-assisted surgery. Acta Neurochir. (Wien) 163(12), 3287–3296. https://doi.org/10.1007/s00701-021-04997-8 (2021).
Funding
Open Access funding enabled and organized by Projekt DEAL. This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conzeptualization: S.M. and E.S.; methodology: S.M., E.S., T.P., J.O.; software: S.M.; validation: E.S.; formal analysis: S.M.; investigation: P.K., M.N.B., C.W., K.S.; resources: E.S.; data curation: S.M., M.N.B.; writing: S.M. and E.S.; visualization: S.M., M.N.B.; supervision: E.S. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Motov, S., Bonk, M.N., Krauss, P. et al. Implementation of a three-dimensional (3D) robotic digital microscope (AEOS) in spinal procedures. Sci Rep 12, 22553 (2022). https://doi.org/10.1038/s41598-022-27082-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-27082-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.