Abstract
This study characterized population-level trends and associations with hepatitis C virus (HCV) antibody (Ab) prevalence in the Middle East and North Africa (MENA). Data source was the standardized and systematically gathered MENA HCV Epidemiology Synthesis Project Database. Random-effects univariable and multivariable meta-regressions were conducted. 2,621 HCV Ab prevalence measures on 49,824,108 individuals were analyzed. In the analysis including all populations, 71% of the variation in prevalence was explained, mostly by at-risk population type. Compared to the general population, prevalence was 23-fold higher among people who inject drugs, and 14-fold higher among high-risk clinical populations. In the analysis including only the general population, 67% of the variation in prevalence was explained, mostly by country/subregion. Compared to Afghanistan, prevalence was highest in Egypt and Pakistan. Prevalence in the general population was declining at a rate of 4% per year, but outside the general population, the decline was at only 1% per year. HCV Ab prevalence in MENA is declining rapidly, but this decline is largely occurring in the general population following introduction of blood and injection safety measures. The decline in populations at higher risk of exposure is slow and below the level needed to achieve HCV elimination by 2030.
Similar content being viewed by others
Introduction
Viral hepatitis is the fifth leading cause of mortality in the Middle East and North Africa (MENA) region, two-thirds of which is caused by hepatitis C virus (HCV)1,2. MENA has the highest burden of HCV infection of all regions1,3,4,5. In 2019, an estimated 470,000 new HCV infections occurred in MENA5, accounting for 30% of the global number of new HCV infections5. Furthermore, in 2019 HCV caused 13,705 deaths due to liver cancer and 57,994 deaths due to cirrhosis and other chronic liver diseases in MENA6. Despite the high burden, only three MENA countries have conducted a nationally representative population-based survey to assess infection levels7,8,9,10. These countries include Egypt8,10, Pakistan7, and Libya9. HCV infection levels in the remaining countries are inadequately characterized.
With the breakthroughs in HCV treatment, and specifically, introduction of highly efficacious direct-acting antivirals (DAA)11, there is a historic opportunity to drastically reduce the burden of HCV infection, and even eliminate this infection as a public health concern. The World Health Organization (WHO) has set elimination of viral hepatitis as a global target by 203012,13. This requires diagnosis of 90% of people living with hepatitis B and/or C and treating 80% of those eligible for treatment should be cured (hepatitis C) or virally suppressed (hepatitis B), in addition to strengthening other prevention components including hepatitis B vaccination, prevention of mother-to-child transmission of hepatitis B, injection safety and harm reduction. With this target in mind, characterizing HCV epidemiology has been rendered all the more critical to help identify carriers of this virus and treating them.
Against this background, the MENA HCV Epidemiology Synthesis Project was launched4, an undertaking to investigate HCV epidemiology in MENA, and to inform public health policy, programming, resource allocation, and research priorities for the region. The aim of the present study is to delineate key trends and associations in HCV epidemiology in MENA through a series of meta-regressions, using the MENA HCV Synthesis Project Database4 that includes approximately 2,600 systematically assembled HCV antibody (Ab) prevalence measures on 50 million individuals.
Methods
Data sources and database
All studies reporting HCV Ab prevalence in a MENA country were extracted from the MENA HCV Epidemiology Synthesis Project Database4. The database was populated through a series of systematic reviews on countries and subregions of MENA including Afghanistan14, Egypt15,16, Fertile Crescent (which includes Iraq, Jordan, Lebanon, Palestine, and Syria), Gulf (which includes Bahrain, Kuwait, Oman, Qatar, Saudi Arabia, and the United Arab Emirates)17, Horn of Africa (which includes Djibouti, Somalia, Sudan, and Yemen), Iran18, Maghreb (which includes Algeria, Libya, Mauritania, Morocco, and Tunisia)19, and Pakistan20. The database included 2,621 Ab prevalence measures on 49,824,108 tested individuals.
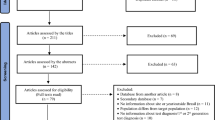
All reviews followed a standardized methodology4,15,16,17,18,19,20,21,22, informed by the Cochrane Collaboration Handbook23, and reported their findings using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA)24. Specific methodology details, including detailed PRISMA flowcharts, can be found in each of the respective systematic reviews4,15,16,17,18,19,20,21,22. In brief, the data sources for these reviews included international scientific databases (PubMed and Embase), regional- and country-level databases (Iran’s Scientific Information database, Iraqi Academic Scientific Journals’ database, among others), reports and routine data from countries and international organizations, the MENA HIV/AIDs Epidemiology Synthesis Project Database25,26, and abstract archives of international scientific conferences.
The search criteria in each of these reviews was broad, employing a combination of index terms and free text terms for HCV and the relevant countries4,15,16,17,18,19,20,21,22. No language restrictions were imposed, and all records reporting HCV measures after the year it was first formally identified, 198927, were included.
Informed by previous literature28,29, the populations tested for HCV Ab were classified into six population categories based on the level of risk of being exposed to HCV infection4,15,16,17,18,19,20,21,22. The categories, along with examples of these populations, can be found in Table 1. An additional category of “mixed” populations was included for studies in which populations of different levels of risk were combined and could not be separated.
Quantitative analysis
Random-effects univariable and multivariable meta-regressions were used to determine predictors and trends in HCV Ab prevalence, along with sources of between-study heterogeneity. A priori relevant variables in these analyses included population or subpopulation, country/subregion, study site, sampling methodology, sample size, year(s) of data collection, and year of publication. Variables were included in the final multivariable analysis model if they were found to be associated with HCV Ab prevalence with a p-value of ≤ 0.20 in the univariable analysis. Adjusted relative risks (ARR) were reported, quantifying the ratio of HCV Ab prevalence relative to a reference HCV Ab prevalence. An ARR with a p-value of ≤ 0.05 indicated strong evidence for an association between that variable and HCV Ab prevalence.
For studies in which the year of data collection was unavailable, this variable was imputed by subtracting the year of data collection in the rest of studies from the year of publication, and using the median of these values in imputing the year of data collection. Sensitivity analysis was performed with and without the imputed values to determine if the imputation had any impact on the results. Meta-regressions were performed on STATA version 13, using the metan command.
Results
All populations analysis
Main analysis
The multivariable meta-regression analysis including all populations explained 71% of the variation in HCV Ab prevalence in MENA and showed that population type is by far the strongest predictor of prevalence (Table 2). Population type explained alone 45% of the variation in HCV Ab prevalence. There was a clear hierarchy by population type and HCV Ab prevalence was lowest in the general population (Fig. 1A). Compared to the general population, HCV Ab prevalence was highest in people who inject drugs (PWID) [ARR of 23.46, (95% confidence interval (CI):18.43–29.87, p < 0.001)], followed by high-risk clinical populations [ARR of 14.44, (95% CI 12.29–16.96, p < 0.001)] (Fig. 1A).
Study site was also a predictor of HCV Ab prevalence (Table 2), but largely because of the association between population type and study site. Still, after controlling for population type, testing at prisons and rehab/drop-in-centers was associated with higher HCV Ab prevalence with an ARR of 4.79 (95% CI 3.55–6.46, p < 0.001) and 4.74 (95% CI 3.28–6.84, p < 0.001), respectively, compared to testing at blood banks.
Country/subregion was a strong predictor of HCV Ab prevalence and explained alone 18% of the variation in prevalence (Table 2). HCV Ab prevalence was highest in Egypt and Pakistan (Fig. 1B). For the remaining countries/subregions, HCV Ab prevalence was much lower and the variation in prevalence across countries was small. The lowest HCV Ab prevalence levels were found in the Fertile Crescent and Iran (Fig. 1B).
The multivariable meta-regression indicated evidence that HCV Ab prevalence is declining. The rate of decline was estimated at 3% per year [ARR of 0.97, (95% CI 0.96–0.98, p < 0.001)].
Additional analysis
For a better understanding of HCV epidemiology outside the general population, the above analysis was repeated, but after excluding all measures in the general population (Table 3). The analysis confirmed similar findings for the effects of population type, study site, and country/subregion, but the estimated rate of decline in HCV Ab prevalence over the last three decades was only 1% per year [ARR of 0.99, (95% CI 0.98–1.00, p = 0.005)].
General population analysis
Main analysis
The analysis including only the general population explained 67% of the variation in HCV Ab prevalence in MENA and showed that country/subregion is by far the strongest predictor of prevalence (Table 4). Country/subregion explained alone 58% of the variation in HCV Ab prevalence. Compared to Afghanistan as a reference country, HCV Ab prevalence in the general population was highest in Egypt [ARR of 8.02, (95% CI 5.57–11.55, p < 0.001)] and Pakistan [ARR of 5.30, (95% CI 3.64–7.72, p < 0.001)]. For the remaining countries/subregions, HCV Ab prevalence was much lower and the variation in prevalence across countries was small. The lowest HCV Ab prevalence levels were found in the Fertile Crescent and Iran (Fig. 1C).
There were only small differences in HCV Ab prevalence by subpopulation of the general population and by study site (Table 4). Most of the differences did not reach statistical significance. There was evidence that HCV Ab prevalence in the general population is declining. The rate of decline was estimated at 4% per year [ARR of 0.96, (95% CI 0.95–0.97), p < 0.001)].
Additional analysis
To confirm the findings of the above analysis, the analysis was repeated excluding all measures in blood donors (Table 5). This was conducted as blood donor data may lead to underestimation of HCV prevalence in the general population at large30,31—blood donors tend to be selectively a healthy and low risk population that is less likely to be HCV infected30. The analysis confirmed similar findings for the effects of country/subregion, subpopulation type, and study site, but the estimated rate of decline in HCV Ab prevalence was slightly lower—it was estimated at 3% per year [ARR of 0.97, (95% CI 0.96–0.98), p < 0.001)].
HCV Ab prevalence and study methods
There was evidence for a strong small-study effect in all analyses. HCV Ab prevalence was lower in studies with a sample size ≥ 100 participants. In the analysis including all populations (Table 2), studies with a sample size ≥ 100 participants reported 29% lower prevalence than studies with a sample size < 100 [ARR of 0.71, (95% CI 0.64–0.79), p < 0.001], indicating a small-study effect. In the analysis for the general population (Table 4), studies with a sample size ≥ 100 participants reported 40% lower prevalence than studies with a sample size < 100 [ARR of 0.60, (95% CI 0.47–0.77), p < 0.001], indicating also a small-study effect.
There was evidence that the sampling methodology also had an effect on reported HCV Ab prevalence, but only in the general population (Table 4). Studies in the general population that did not use probability-based sampling reported 35% lower prevalence than studies that used probability-based sampling [ARR of 0.65, (95% CI 0.54–0.78), p < 0.001]. No evidence was seen for this effect in the analysis for all populations other than the general population (Table 3).
A sensitivity analysis was conducted to examine whether the imputation calculation for the year of data collection could have affected the study findings. The analysis confirmed the same findings for both, the analysis for all populations (Supplementary Table S1) and the analysis for the general population (Supplementary Table S2). An additional sensitivity analysis was conducted excluding studies with a sample size of < 100 participants, to examine the impact of the small-study effect that was observed in the previous analyses. The analysis confirmed the same findings as those of the main analysis (Supplementary Table S3).
Discussion
HCV Ab prevalence is declining rapidly in the population of MENA at a rate of 3–4% per year (Tables 2 and 4). This decline may be explained by the broad improvements in blood supply screening, injection safety, and infection control that have been rolled out over the last three decades following the discovery of this infection32. The observed decline supports the effectiveness of these interventions and demonstrates the importance of their scale-up in all countries. Demography may also contribute to explaining the decline. The decline may reflect a cohort effect, in a context of rapidly growing population size over the last three decades33,34. Exposure to HCV infection may have been higher in earlier decades34, but most of the living population of MENA was born after the year 1990.
However, this decline largely reflects the decline in HCV transmission in the general population, where the rate of decline was steepest (Tables 4 and 5). The decline in populations at higher risk of exposure was modest at only 1% per year (Table 3). This suggests that HCV transmission is increasingly becoming concentrated in higher risk populations with limited transmission in the general population, at least in most countries. This is a consequence of the specific interventions that have been effectively implemented in MENA, including injection and blood safety32, that reduced transmission in the general population, but less so in other populations, including PWID and high-risk clinical populations. This highlights the importance of expanding harm reduction interventions among PWID35,36 and in prisons37, and the need for further improvements in infection control at healthcare facilities38.
The findings indicate reasons for optimism, but also reasons for concern. The rapidly declining HCV Ab prevalence is consistent with progress towards the WHO elimination target by 2030. However, the findings also highlight that this progress is likely to stall, as the improvements are happening in the general population and not in the populations at higher risk, where most infection incidence will be occurring over the coming years. Without major improvements in tackling HCV incidence among PWID and high-risk clinical populations, such as through different strategies for screening and treatment39,40,41, it is unlikely that the region will achieve the WHO elimination target by 2030. Moreover, improvements may materialize in some countries of the region, such as in Egypt, which has had a successful national program for screening and treatment42, but less so in other countries such as in Pakistan where incidence continues at considerable levels, including in the general population43,44,45,46.
The findings demonstrate a clear epidemiological pattern of a hierarchy in HCV Ab prevalence by population type. The likelihood of being infected varied immensely across populations. Compared to the general population, the risk of being infected was 23-fold higher for PWID and 14-fold higher for high-risk clinical populations (Table 2). HCV Ab prevalence varied also substantially across countries/subregions within MENA, highlighting how the epidemiology of this infection can vary from one country to another, even within the same region, reflecting historical factors, particularly relating to expansion of healthcare during the twentieth century43,44,47,48.
The analyses identified a strong small-study effect49 in reporting HCV Ab prevalence (Tables 2–5). For example, in studies among the general population, studies with a sample size ≥ 100 participants reported 40% lower prevalence than studies with a sample size < 100, highlighting how studies employing small samples are likely to have been in select populations that were not in truth representative of the wider general population.
The analyses identified also a strong effect for the sampling methodology on reported HCV Ab prevalence, but only in the general population (Tables 4 and 5). Studies in the general population that did not use probability-based sampling reported 35% lower prevalence than studies that used probability-based sampling. This outcome may reflect that studies using convenience samples drawn from the general population are likely to underestimate HCV Ab prevalence in the total population, perhaps because of under-sampling of PWID and high-risk clinical populations who are harder to reach and may not participate in general population surveys50.
This study aimed to characterize trends and associations with HCV Ab prevalence, however, not all those who are HCV Ab positive are chronically infected by HCV. Our earlier review and meta-analysis for HCV viremic rate (proportion of chronically infected individuals out of HCV Ab positive individuals) found that the overall pooled mean viremic rate in MENA is 67.6% (95% CI 64.9–70.3%)51. Across risk populations, the pooled mean rate ranges between 57.4% (95% CI 49.4–65.2%) in people who inject drugs, and 75.5% (95% CI 61.0–87.6%) in populations with liver-related conditions51. Across countries/subregions of MENA, the pooled mean rate ranges between 62.1% (95% CI 50.0–72.7%) and 70.4% (95% CI 65.5–75.1%)51.
Recent scale-up of HCV treatment, such as in Egypt42, should also have reduced the viremic rate in at least some countries. These reductions in viremic rate, that are coincident with HCV Ab prevalence declines, should amplify the reductions in HCV incidence in MENA. This outcome highlights the need to have current estimates for HCV incidence in the different countries of the region, as well as estimates of those chronically infected and in need of treatment, to inform policy and programming efforts. Such estimates can be available through mathematical modeling, as was done for Egypt52 and Pakistan41, but such studies need to be extended also to the rest of the MENA countries.
This study has limitations. With the scale-up of HCV treatment, HCV Ab prevalence will increasingly become less associated with chronic-infection prevalence51,53. However, the impact of this on presented analyses is probably minimal given that treatment scale-up is recent in MENA and treatment coverage remains low in nearly all countries in the region54. There was variability in the availability of data across MENA countries. Despite this, a key strength of this study is the large analyzed database, assembled through a standardized protocol, which to our knowledge, is the largest and most comprehensive for HCV infection in MENA. The use of this database allowed for extensive analyses in the present study that should provide in the future a framework and quantitative adjustment factors for a representative mathematical modeling estimation of HCV infection levels and numbers of persons affected by this infection in each of MENA countries. The study provides a methodological component in the estimation processes of HCV infection and disease burden at a time when these estimates are critically needed to track and validate progress towards HCV elimination by 2030.
In conclusion, HCV Ab prevalence is declining in MENA, however, this decline is mainly occurring in the general population, due to interventions such as injection and blood safety. Despite this decline, HCV incidence remains higher in MENA relative to other WHO regions, with an estimated 470,000 new HCV infections in 20195. HCV infection appears to be increasingly concentrated in higher risk populations. Achieving elimination of HCV infection by 2030 hinges on expansion of screening and treatment programs, harm reduction services for PWID in settings such as prisons and rehab/drop-in-centers, and enforcement of stringent infection control and sanitary healthcare practices in clinical settings.
References
Stanaway, J. D. et al. The global burden of viral hepatitis from 1990 to 2013: Findings from the Global Burden of Disease Study 2013. The Lancet 388, 1081–1088 (2016).
Mohd Hanafiah, K., Groeger, J., Flaxman, A. D. & Wiersma, S. T. Global epidemiology of hepatitis C virus infection: new estimates of age-specific antibody to HCV seroprevalence. Hepatology 57, 1333–1342 (2013).
World Health Organization (WHO). Global Hepatitis Report, 2017. Available at: http://www.who.int/hepatitis/publications/global-hepatitis-report2017/en/. (accessed 7 October 2021).
World Health Organization. Epidemiology of hepatitis C virus in the WHO Eastern Mediterranean Region: implications for strategic action. Report No. 9789290222866, (Cairo: WHO Regional Office for the Eastern Mediterranean, Available at: https://apps.who.int/iris/bitstream/handle/10665/336174/9789290222866-eng.pdf?sequence=1&isAllowed=y, 2020).
World Health Organization. Global progress report on HIV, viral hepatitis and sexually transmitted infections, 2021: accountability for the global health sector strategies 2016–2021: actions for impact: web annex 2: data methods. Report No. 9240030999, (2021).
Global Burden of Disease Collaborative Network.
Global Burden of Disease Study 2019 (GBD 2019) Results. Seattle, United States: Institute for Health Metrics and Evaluation (IHME), 2020. Available from https://vizhub.healthdata.org/gbd-results/. Accessed Oct 6, 2022.
Qureshi, H., Bile, K. M., Jooma, R., Alam, S. E. & Afridi, H. U. R. Prevalence of hepatitis B and C viral infections in pakistan: Findings of a national survey appealing for effective prevention and control measures. Eastern Med Health J 16, S15-23 (2010).
El-Zanaty, F. & Way, A. Egypt Demographic and Health Survey 2008, (Ministry of Health, El-Zanaty and Associates, and Macro International (Egypt, 2009).
Daw, M. A. & El-Bouzedi, A. Prevalence of hepatitis B and hepatitis C infection in Libya: Results from a national population based survey. BMC Infect. Dis. 14, 17. https://doi.org/10.1186/1471-2334-14-17 (2014).
Ministry of Health and Population [Egypt], El-Zanaty and Associates [Egypt], ICF International. Egypt Health Issues Survey 2015. Cairo: Ministry of Health and Population, 2015.
Flamm, S. L. Advances in the treatment of hepatitis C virus infection from EASL 2015. Gastroenterol. Hepatol. 11, 1–23 (2015).
World Health Organization. Global health sector strategy on viral hepatitis 2016–2021. Towards ending viral hepatitis. Report No. WHO/HIV/2016.06, (Available at: https://apps.who.int/iris/bitstream/handle/10665/246177/WHO-HIV-2016.06-eng.pdf?sequence=1, 2016).
World Health Organization. Combating hepatitis B and C to reach elimination by 2030: advocacy brief. Report No. WHO/HIV/2016.04, (Geneva, WHO, Available at: https://apps.who.int/iris/bitstream/handle/10665/206453/WHO_HIV_2016.04_eng.pdf, 2016).
Chemaitelly, H., Mahmud, S., Rahmani, A. M. & Abu-Raddad, L. J. The epidemiology of hepatitis C virus in Afghanistan: Systematic review and meta-analysis. Int. J. Infect. Dis.: IJID : Off. Publ. Int. Soc. Infect. Dis. https://doi.org/10.1016/j.ijid.2015.09.011 (2015).
Kouyoumjian, S., Chemaitelly, H. & Abu-Raddad, L. J. Characterizing hepatitis C virus epidemiology in Egypt: systematic reviews, meta-analyses, and meta-regressions. Sci. Rep. 8, 1661. https://doi.org/10.1038/s41598-017-17936-4 (2018).
Mohamoud, Y. A., Mumtaz, G. R., Riome, S., Miller, D. & Abu-Raddad, L. J. The epidemiology of hepatitis C virus in Egypt: A systematic review and data synthesis. BMC Infect. Dis. 13, 288. https://doi.org/10.1186/1471-2334-13-288 (2013).
Mohamoud, Y. A., Riome, S. & Abu-Raddad, L. J. Epidemiology of hepatitis C virus in the Arabian Gulf countries: Systematic review and meta-analysis of prevalence. Int. J. Infect. Dis.: IJID: Off. Publ. Int. Soc. Infect. Dis. https://doi.org/10.1016/j.ijid.2016.03.012 (2016).
Mahmud, S., Akbarzadeh, V. & Abu-Raddad, L. J. The epidemiology of hepatitis C virus in Iran: Systematic review and meta-analyses. Sci. Rep. 8, 150 (2018).
Fadlalla, F. A., Mohamoud, Y. A., Mumtaz, G. R. & Abu-Raddad, L. J. The epidemiology of hepatitis C virus in the maghreb region: systematic review and meta-analyses. PLoS ONE 10, e0121873. https://doi.org/10.1371/journal.pone.0121873 (2015).
Al Kanaani, Z., Mahmud, S., Kouyoumjian, S. P. & Abu-Raddad, L. J. The epidemiology of hepatitis C virus in Pakistan: systematic review and meta-analyses. R. Soc. Open Sci. 5, 180257. https://doi.org/10.1098/rsos.180257 (2018).
Chemaitelly, H., Chaabna, K. & Abu-Raddad, L. J. The Epidemiology of Hepatitis C Virus in the Fertile Crescent: Systematic Review and Meta-Analysis. PLoS ONE 10, e0135281. https://doi.org/10.1371/journal.pone.0135281 (2015).
Chaabna, K., Kouyoumjian, S. P. & Abu-Raddad, L. J. Hepatitis C Virus Epidemiology in Djibouti, Somalia, Sudan, and Yemen: Systematic Review and Meta-Analysis. PLoS ONE 11, e0149966. https://doi.org/10.1371/journal.pone.0149966 (2016).
The Cochrane collaboration. Cochrane handbook for systematic reviews of interventions. (Wiley-Blackweill, 2008).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & Group, P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6, e1000097, https://doi.org/10.1371/journal.pmed.1000097 (2009).
Abu-Raddad L, A. F., Semini I, Reidner G, Wilson D, Tavil O. Characterizing the HIV/AIDS epidemic in the Middle East and North Africa: time for strategic action. (Washington DC: The World Bank Press, 2010).
Abu-Raddad, L. J. et al. Epidemiology of HIV infection in the Middle East and North Africa. AIDS (London, England) 24(Suppl 2), S5-23. https://doi.org/10.1097/01.aids.0000386729.56683.33 (2010).
Kuo, G. et al. An assay for circulating antibodies to a major etiologic virus of human non-A, non-B hepatitis. Science 244, 362–364 (1989).
Lavanchy, D. Evolving epidemiology of hepatitis C virus. Clin. Microbiol. Infect.: The Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 17, 107–115. https://doi.org/10.1111/j.1469-0691.2010.03432.x (2011).
Gower, E., Estes, C., Blach, S., Razavi-Shearer, K. & Razavi, H. Global epidemiology and genotype distribution of the hepatitis C virus infection. J. Hepatol. 61, S45–S57 (2014).
Zou, S. et al. Prevalence, incidence, and residual risk of human immunodeficiency virus and hepatitis C virus infections among United States blood donors since the introduction of nucleic acid testing. Transfusion 50, 1495–1504. https://doi.org/10.1111/j.1537-2995.2010.02622.x (2010).
Mahmud, S., Chemaitelly, H., Alaama, A. S., Hermez, J. G. & Abu-Raddad, L. Hepatitis C virus among blood donors and general population in Middle East and North Africa: Meta-analyses and meta-regressions. World J. Meta-Anal. 10, 12–24 (2022).
World Health Organization. Global status report on blood safety and availability 2016. Available at: https://apps.who.int/iris/bitstream/handle/10665/254987/9789241565431-eng.pdf; 2017 Accessed on: 1/12/21. Report No.: 9789241565431.
United Nations Population Division. World population prospects: the 2015 revision, <http://esa.un.org/unpd/wpp/DataQuery/> (2015).
Ayoub, H. H., Chemaitelly, H., Kouyoumjian, S. P. & Abu-Raddad, L. J. Characterizing the historical role of parenteral antischistosomal therapy in hepatitis C virus transmission in Egypt. Int. J. Epidemiol. 49, 798–809 (2020).
Mahmud, S. et al. The status of hepatitis C virus infection among people who inject drugs in the Middle East and North Africa. Addiction 115, 1244–1262. https://doi.org/10.1111/add.14944 (2020).
Mumtaz, G. R. et al. HIV among people who inject drugs in the Middle East and North Africa: systematic review and data synthesis. PLoS Med. 11, e1001663. https://doi.org/10.1371/journal.pmed.1001663 (2014).
Heijnen, M., Mumtaz, G. R. & Abu-Raddad, L. J. Status of HIV and hepatitis C virus infections among prisoners in the Middle East and North Africa: review and synthesis. J. Int. AIDS Soc. 19, 20873. https://doi.org/10.7448/IAS.19.1.20873 (2016).
Mahmud, S., Kouyoumjian, S. P., Al Kanaani, Z., Chemaitelly, H. & Abu-Raddad, L. J. Individual-level key associations and modes of exposure for hepatitis C virus infection in the Middle East and North Africa: a systematic synthesis. Ann Epidemiol 28, 452–461, https://doi.org/10.1016/j.annepidem.2018.03.007 (2018).
Chemaitelly, H. et al. Who to test for Hepatitis C virus in the Middle East and North Africa?: Pooled analyses of 2500 prevalence measures, including 49 million tests. Hepatol. Commun. 3, 325–339. https://doi.org/10.1002/hep4.1310 (2019).
Ayoub, H. H. & Abu-Raddad, L. J. Impact of treatment on hepatitis C virus transmission and incidence in Egypt: A case for treatment as prevention. J. Viral Hepat. 24, 486–495. https://doi.org/10.1111/jvh.12671 (2017).
Ayoub, H. H. & Abu-Raddad, L. J. Treatment as prevention for hepatitis C virus in Pakistan: mathematical modelling projections. BMJ Open 9, e026600. https://doi.org/10.1136/bmjopen-2018-026600 (2019).
Waked, I. et al. Screening and treatment program to eliminate hepatitis C in Egypt. N. Engl. J. Med. 382, 1166–1174. https://doi.org/10.1056/NEJMsr1912628 (2020).
Mahmud, S., Al Kanaani, Z. & Abu-Raddad, L. J. Characterization of the hepatitis C virus epidemic in Pakistan. BMC Infect. Dis. 19, 809. https://doi.org/10.1186/s12879-019-4403-7 (2019).
Ayoub, H. H., Al Kanaani, Z. & Abu-Raddad, L. J. Characterizing the temporal evolution of the hepatitis C virus epidemic in Pakistan. J Viral Hepat 25, 670–679, https://doi.org/10.1111/jvh.12864 (2018).
Lim, A. G. et al. Curbing the hepatitis C virus epidemic in Pakistan: the impact of scaling up treatment and prevention for achieving elimination. Int. J. Epidemiol. 47, 550–560. https://doi.org/10.1093/ije/dyx270 (2018).
Lim, A. G. et al. Health and economic benefits of achieving hepatitis C virus elimination in Pakistan: A modelling study and economic analysis. PLoS Med. 18, e1003818. https://doi.org/10.1371/journal.pmed.1003818 (2021).
Ayoub, H. H., Chemaitelly, H., Kouyoumjian, S. P. & Abu-Raddad, L. J. Characterizing the historical role of parenteral antischistosomal therapy in hepatitis C virus transmission in Egypt. Int. J. Epidemiol. 49, 798–809. https://doi.org/10.1093/ije/dyaa052 (2020).
Miller, F. D. & Abu-Raddad, L. J. Evidence of intense ongoing endemic transmission of hepatitis C virus in Egypt. Proc. Natl. Acad. Sci. U.S.A. 107, 14757–14762. https://doi.org/10.1073/pnas.1008877107 (2010).
Smolak, A., Chemaitelly, H., Hermez, J. G., Low, N. & Abu-Raddad, L. J. Epidemiology of Chlamydia trachomatis in the Middle East and north Africa: A systematic review, meta-analysis, and meta-regression. Lancet Glob. Health 7, e1197–e1225 (2019).
Edlin, B. R., Eckhardt, B. J., Shu, M. A., Holmberg, S. D. & Swan, T. Toward a more accurate estimate of the prevalence of hepatitis C in the United States. Hepatology 62, 1353–1363 (2015).
Harfouche, M. et al. Hepatitis C virus viremic rate in the Middle East and North Africa: Systematic synthesis, meta-analyses, and meta-regressions. PloS one 12 (10) https://doi.org/10.1371/journal.pone.0187177 (2017).
Ayoub, H. & Abu-Raddad, L. J. Impact of treatment on hepatitis C virus transmission and incidence in Egypt: A case for treatment as prevention. J. Viral Hepatitis 24, 486–495. https://doi.org/10.1111/jvh.12671 (2017).
Ayoub, H. H., Chemaitelly, H., Omori, R. & Abu-Raddad, L. J. Hepatitis C virus infection spontaneous clearance: has it been underestimated?. Int. J. Infect. Dis.: IJID: Off. Publ. Int. Soc. Infect. Dis. 75, 60–66. https://doi.org/10.1016/j.ijid.2018.07.013 (2018).
HCV Status 2020, EMRO, Regional Dashboard. Polaris Observatory - CDA Foundation. Available at: https://cdafound.org/polaris-regions-dashboard/. Accessed on: 4/12/2021.
Acknowledgements
The authors would like to thank Dr. Steven D. Aird for proofreading this manuscript.
Funding
This work was supported by the National Priorities Research Program (NPRP) [Grant Number 12S-0216–190094] from the Qatar National Research Fund (a member of Qatar Foundation). The statements made herein are solely the responsibility of the authors. The authors are also grateful for infrastructure support provided by the Biostatistics, Epidemiology, and Biomathematics Research Core at Weill Cornell Medicine-Qatar.
Author information
Authors and Affiliations
Contributions
S.M. conducted data extraction and analysis, and wrote the first draft of the paper. L.J.A. conceived and led the design of the study, analyses, and drafting of the article. All authors contributed to data collection and acquisition, and/or database development, and/or discussion and interpretation of the results, and to the writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mahmud, S., Chemaitelly, H., Alaama, A.S. et al. Characterizing trends and associations for hepatitis C virus antibody prevalence in the Middle East and North Africa: meta-regression analyses. Sci Rep 12, 20637 (2022). https://doi.org/10.1038/s41598-022-25086-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-25086-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.