Abstract
Road traffic mortalities (RTMs), a leading cause of death globally, mostly occur in low- and middle-income countries, and having sufficient healthcare resources could lower the number of these fatalities. Our study aimed to illustrate the incidence of RTMs per 100,000 population and to compare the distribution of healthcare resources from 2011 to 2021 with rates of RTMs in the 77 provinces of Thailand. We divided the population into adults (≥ 15 years) and children (0–14 years). Lorenz curve and Gini coefficient were used to measure the level of distribution and equality of hospital resources and in relation to RTMs across the country. The average number of deaths was 30.34 per 100,000 per year, with male predominance. The RTM rates for adults and children were 32.71 and 19.08 per 100,000 respectively, and motorcycle accidents accounted for the largest percentage of deaths across all age groups. The Gini coefficient showed that operating rooms (0.42) were the least equally distributed hospital resource, while physicians were the most equally distributed (0.34). Anomalies were identified between the distribution of RTMs and available hospital resources. We hope our study will be beneficial in reallocating these resources more fairly to reflect the different numbers of traffic accidents in each province with the aim of reducing lower traffic-related deaths.
Similar content being viewed by others
Introduction
Road traffic injuries (RTIs) are among the leading causes of death, and it is expected that by 2030 they will rise from 9 to 7th in the global ranking, causing significant public health concerns1,2. A road traffic mortality (RTM) is defined as any person killed immediately or dying within 30 days of a road traffic incident3. Ninety percent of these deaths occur in low- and middle-income countries (LMICs) despite the fact that these nations have only 54% of the vehicles in the world4. According to the World Health Organisation (WHO) estimates, there are 32.7 fatalities per 100,000 people, with motorcycles accounting for the majority most of these deaths5. Traffic-related mortality and morbidity in LMICs have created a great burden, with an estimated 90% of disability-adjusted life years (DALYs) being lost worldwide as a result of RTIs which occur in LMICs6.
Pre-hospital and in-hospital trauma services for LMICs have been found to be insufficient7,8. Regions with low and moderate health care resources (HCRs) have been found to have higher rates of mortality from RTIs than those with high HCRs9. Hence, if HCRs were re-distributed to cater for regions with high rates of RTMs, the RTI mortality and morbidity rates could potentially be reduced.
Thailand, a middle-income country, had the second-highest rate of RTMs globally in 20155, which was partly due to a sharp rise in motorisation triggered by economic expansion6. In 2017, road accidents cost Thailand over 60 million dollars, approximately 0.8% of the nation’s gross domestic product (GDP)10.
More than half of all road traffic deaths are amongst vulnerable road users such as pedestrians, cyclists, and motorcyclists. Male victims have been reported to outnumber females approximately threefold, with motorcyclists accounting for about four-fifths of fatalities11. Globally, 186,300 children aged between 0 and 9 years, die from road traffic accidents each year12. Injured children who are treated at paediatric trauma centres have better outcomes than those who are cared for in an adult centre or a non-trauma centre13. This reflects the fact that children require specific medical care which is different from that needed for adults; therefore, statistics on children’s mortality rates need to be investigated.
This report aims to assess the equality of the distribution of hospital resources, taking into account RTMs in Thailand; to observe RTM trends over 11 years for the whole population, dealing with adults and children separately; and to analyse potential factors affecting RTM rates.
Methods
Study setting
This study gathered information from Thailand, a middle-income country located in Southeast Asia populated by over 70 million people across 513,120 km2. There are 77 provinces, and Bangkok is the capital city. The total number of registered vehicles in 2022 was 41,346,378, of which half were motorcycles.
This retrospective, cross-sectional study was approved by the institutional review board (IRB) of Rajavithi Hospital, Thailand and was conducted in accordance with the tenets of the Declaration of Helsinki. Informed consent was not obtained in this study, as approved by the hospital’s IRB.
The number of RTMs were recorded over an 11-year period between January 1, 2011 and December 31, 2021. The RTM data were compiled by the Department of Disease Control of the Ministry of Public Health, which gathered details from three sources: death certificates; reported deaths from traffic injuries on the Police Information System; and from the central motor vehicle insurance registry. All data were approved and released on the official website of the Digital Government Development Agency.
Data included age, sex, type of accident (motorcycles, cars, pedestrians, trucks including ten wheelers and agriculture vehicles, and bicycles), and cause of death. The latter was recorded using the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD10).
The National Statistical Office provided information regarding Thailand’s population and healthcare personnel and facilities. The population was divided into adults and children, defined according to Thailand’s law as those aged below 15 years. The total population was taken as the average population over 11 years. In terms of hospital resources, we included number of hospital beds, operating rooms (ORs), intensive care unit (ICU) beds, physicians, and nurses. Information regarding hospital resources were gathered for each province over the same 11-year period as the population data.
We also reported RTMs before and during the COVID-19 pandemic, which we defined as the (two-year) pandemic period between January 1st, 2020 and December 31st, 2021.
Factors that were used to assess the correlations with RTMs in the 77 provinces in Thailand were as follows: average income per year; the number of registered vehicles; the volume of oil usage; and the volume of rain, details of which were provided by The National Statistical Office.
Statistical analysis
Road traffic mortality rates per 100,000 population were calculated and divided into three groups (total, adults, and children) for all provinces. The number of beds, ORs, ICU beds, physicians, and nurses were also calculated per 100,000 population for each province. Frequencies and percentages were used for categorical data while continuous data were reported using mean, median, and standard deviation (SD) after confirmation of normal distribution of the data. Paired-T test was used to compare the number of fatalities during and prior to the COVID-19 pandemic.
Lorenz curve and Gini coefficient were used to measure the level of distribution and equality of health care resources and in relation to incidences of RTMs across the country. Spearman rank-order correlation analysis was used to evaluate the correlations between related factors and RTMs.
The Lorenz curve compares the distribution of a specific variable with uniform distribution representing equality, which is shown by a diagonal line14,15. The farther the Lorenz curve is from the diagonal line, the greater the inequality. The cumulative proportion of the RTMs is shown on the x axis, and the cumulative proportion of healthcare resources on the y axis. The Gini coefficient is the ratio of the area between the Lorenz curve and the diagonal line, to the area below the diagonal line in the Lorenz curve. Gini coefficient values range from 0 to 1, with 0 being perfect equality, and 1 representing the maximum inequality possible.
All statistical analyses were done with Microsoft excel and SPSS version 22 for Windows, and a p-value of < 0.05 was consider statistically significant.
Ethics declarations
This study has been approved by the Ethics Committee of Rajavithi Hospital (Number 65067).
Results
Overall
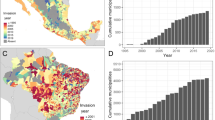
The total number of RTMs over these 11 years was 218,964, of which the majority were adults (89.11%). The average number of deaths was 30.34 per 100,000 people per year with male predominance. The RTI mortality rates for adults and children were 32.71 and 19.08 per 100,000 respectively (Table 1, Fig. 1).
A statistically significant difference was found between the overall rates of RTMs before COVID-19 and during the pandemic, with average ratios of 32.05 (± 1.61) and 22.82 (± 5.83) (P = 0.001) deaths per 100,000 respectively.
RTMs for the entire population were highest in 2011, at 34.33 per 100,000 and lowest in 2021 at 18.7 per 100,000. RTMs involving children were highest in 2019, going up to 26.09 deaths per 100,000 children (Table 1).
Overall, the mean age of death was 39.68 ± 19.92 years. With regard to children, the mean age of death was 10.45 ± 4.19 years (Table 1).
Type of road accidents
Motorcycle accidents were the most common cause of death across all age groups, while bicycle accidents were responsible for less than 1% of RTMs throughout the period. Over these 11 years, the type of accidents showed a relatively similar trend for adults and children (Table 2). The most common ICD-10 diagnosis for the cause of death was V892: person injured in unspecified motor-vehicle accident, at 43.35%, followed by V299: motorcycle rider(driver)(passenger) injured in unspecified traffic accident, at 14.12%.
RTMs across each province
Rayong had the highest number of RTMs for the whole population and for adults at 62.05 and 66.94 deaths per 100,000 population respectively while Mae Hong Sorn had the fewest RTMs per 100,000 population out of all 77 provinces. Bangkok, the capital city of Thailand, had 14.41 RTMs per 100,000 population, ranking it as the third-lowest province in terms of RTMs per population (Supplementary Table S1). Rates of RTMs per 100,000 population are illustrated on the heat map (Fig. 2).
Distribution of hospital resources
Bangkok had the most hospital resources per 100,000 population in terms of hospital beds, ORs, ICU beds, physicians, and nurses. The average number of hospital beds and ICUs were 164.11 and 9.46 per 100,000 population respectively. Pathum Thani had the lowest number of beds and ORs per population, while the lowest number of ICUs per population was found in Chaiyaphum. There were on average 37.34 physicians and 207.65 nurses per 100,000 people. Samut Sakhon had the lowest number of physicians, while Bueng Kan had the fewest nurses (Supplementary Table S1).
The levels of equality in distribution of HCRs throughout Thailand are illustrated by Lorenz curve (Fig. 3). According to the Gini coefficient, the resource that was least equally distributed was the number of ORs (0.42), while physicians were most equally distributed (0.34) (Table 3).
Associated factors
Income per year (P = 0.001), number of registered vehicles (P = 0.003), and amount of oil consumption (P = 0.002) all had moderate positive correlations with RTMs while the volume of rainfall did not (Table 4, Fig. 4).
Discussion
Thailand, part of Southeast Asia, is an LMIC with over 70 million people spread unevenly across 77 provinces, with half of registered vehicles being motorcycles. RTIs are the second leading cause of death in Thailand16, with approximately 30 out of 100,000 people dying from these incidents every year, and children accounting for over 10% of these fatalities. Throughout the 11 years of this study, motorcycles were the main vehicles involved in RTMs, followed by cars, and a significant difference was seen between mortality rates before and during the COVID-19 pandemic. There were significant disparities between the distribution of hospital resources and rates of RTMs across Thailand.
Overall
In 2010, RTIs accounted for 334,815 deaths in South-East Asia. RTMs were higher in middle-income nations than in low-income countries17. Thailand had on average 30.34 deaths per 100,000 population from RTIs, and neighbouring LMIC Malaysia reported similar mortality rates of 34.5 RTMs per 100,000 population18. In contrast, mortality rates from RTIs in two other Southeast Asian countries, Laos and Vietnam, were 11.619 and 20.320 per 100,000 population respectively.
RTMs are a significant health concern in the paediatric population. Studies have analysed injury rates of children involved in road traffic accidents, and LMICs have been found to account for 95% of RTMs in children globally21. Our study showed that the mortality rate for children involved in RTIs was 19.08 per 100,000 and rose to as high as 26 per 100,000 children. Previous studies in Thailand have reported that 80% of the injured and dead from RTIs were motorcyclists22. Traffic accidents were the second most common paediatric injury in Thailand, with head injury being the most common cause of death23. For adolescents aged 14–19, road accidents were reported as the number one cause of death24. Malaysia reported that in 2013, the main cause of death for 10- to 24-year-old males was transport-related injury, with those sustained by people traveling by car and motorbike responsible for 20 and 5.5 per 100,000 deaths from all causes respectively25. In stark contrast, a study from Australia, a high-income country, showed RTI mortality rates at between 6.3 and 10.3 per 100,000 population26, and mortality rates for children < 15 years old in the United States ranged between 0.25 and 21.91 deaths per 100,000 children. Decreased mortality rates have been associated with the availability of trauma centers in the county27.
Premature childhood deaths result in societal as well as economic losses, with Thailand reporting that premature mortality contributed up to 88% of DALYs lost due to RTIs. This is high compared to other countries such as Australia (73%), Iran (62%), and Serbia (57%)11. Higher proportions of RTMs in LMICs result from the popularity of motorcycles, which are more affordable in these countries. Thailand was faced with a loss of about 100 million USD of quality-adjusted life years or approximately 300 million USD of value of statistical life years from traffic mortalities between 2010 and 201224.
Lockdown policies during the COVID-19 pandemic led to a sharp drop in traffic volume and a global decline in RTIs28,29. Travel restrictions imposed during COVID-19 significantly reduced vehicle mobility by more than 50% worldwide. Though relative increases in severity of injury and numbers of deaths were observed, the pandemic reduced the absolute number of RTIs. Like other countries, Thailand faced lockdown policies and decreased road usage together with alcohol restrictions. These road usage restrictions were implemented in April 2020, when people were not allowed to leave their homes between 10 PM and 4 AM, and traveling between cities was prohibited. The attendant decrease in the number of hours of road usage, along with the alcohol-free period, led to a significant decline in RTMs in Thailand during the COVID-19 pandemic. Interestingly, in 2021, around 21,000 people died from COVID-19 infection, while deaths form traffic accidents numbered approximately 12,000.
The average age of people dying as a result of RTIs was 40 years old, which is in the working age group. Productivity losses due to road traffic accidents are mainly concentrated in the 16- to 45-year-old groups. Road traffic injuries and fatalities in young adults significantly affect the nation’s GDP since younger people bear the largest share of the economic burden10,22.
Type of road accidents
Regions that were more populated did not necessarily have higher RTMs. Distribution of RTMs by road user groups has been shown to vary across countries. Motorcyclists account for most of the RTMs in Southeast Asian regions, while motorised four-wheelers constitute less than 20% of traffic-related mortalities6, and this in keeping with the findings of our study. Eighty-eight percent of motorized 2–3 wheelers are found in LMICs, with 75% in Southeast Asia30. Thailand was noted to have a high usage of 2-wheelers in addition to lax law enforcement, causing higher 2-wheeler deaths than in countries like Japan where law enforcement is more rigorous4. The second most common ICD-10 diagnosis from our study of persons injured in motor-vehicle accidents was specified as motorcycle injury. Similarly, Laos reported that 76% of RTIs involved motorcyclists19.
RTMs across each province
Rayong and Chonburi were the two provinces with the highest RTMs at 62 and 49 per 100,000 population, possibly because they had the highest proportion of motorcycles per population; in fact, the number of registered motorcycles exceeded the population of the provinces. Bangkok has about a tenth of the country’s population with RTMs at only about a fourth of these top two provinces. This highlights the fact that higher numbers of people does not necessarily mean more road accidents. Studies have found that less-urbanised districts were associated with higher mortality than large metropolitan areas27. Other risk factors involved in RTMs in Southeast Asia were type of roads, number of male motorcycle drivers, driving without a driver’s license, and non-use of helmets31.
Distribution of hospital resources
Both in-hospital and pre-hospital care have been identified as factors affecting RTMs32,33,34,35,36,37. A paper from Iran showed that pre-hospital trauma care was dispensed unequally across the nation and should be adjusted to reduce the number of RTMs32. The estimated number of lives that could potentially be saved globally if a complete trauma system with 100% coverage was available in LMICs was estimated at 200,000 per year. Having trauma centres and efficient trauma teams has also been shown to reduce deaths from RTIs38. Mortality rates from motorcycle injuries in the United Arab Emirates dropped significantly due to improved pre-hospital and in-hospital trauma care39.
Our study looked further into the distribution of available hospital resources and found that they were not balanced in accordance with mortality rates from RTIs in each province. A paper from Poland reported that poor HCRs were responsible for anomalies in mortality rates due to traffic accidents in each region9 and that ORs were found to be the least equally distributed out of all the hospital resources. This is due to the extensive process required to provide appropriate venues, as well as surgical teams and equipment, making it harder to open ORs. In contrast, physicians in Thailand were more equally distributed than other resources, and this could be because Thailand has been trying to allocate enough doctors to each province according to its population. HCRs were previously allocated according to the number of people in each province, which was why Bangkok, which had the highest population, had the most HCRs per 100,000 population. Physicians and nurses could be reallocated appropriately, and provision of other facilities, such as ORs and ICUs, could be integrated into healthcare policies, while taking into account the rates of RTMs in each province and focusing attention on trauma teams and facilities.
Associated factors
Gross national income (GNI), urban speed limits, road quality, and regular road infrastructure inspections have all been shown to be influential factors in the rate of RTMs40,41,42,43,44. Countries with high GNI per capita have fewer deaths per 100,000 population even though they have higher numbers of vehicles while nations with low GNI per capita have higher rates of deaths per 100,000 population despite having fewer vehicles4.
Traffic injuries have repeatedly been shown to follow the trends of economic growth. Globally, a drastic increase in the number of vehicles led to RTMs reaching 135 cases per 100 vehicles in the year 2000, but this fell to 64 cases per 100 vehicles in 201631. Other factors that were found from this study to correlate with RTMs were, income, number of registered vehicles, and amount of precipitation. RTIs in Thailand have been shown to go in the same direction as the nation’s economy45.
Amounts of precipitation did not correlate with RTMs in our study, in contrast to another study previously conducted in Thailand which found a significant increase in road accidents resulting from high rainfall. These contradictory results were probably due to differences in data collection and analysis: our study calculated the amount of rain throughout the year and found no correlation with RTMs while the previous study grouped different rain intensities measured by daily rates of precipitation46.
Strengths and weaknesses
One of the main strengths of this study was that it provided the largest data available in all 77 provinces in Thailand from various reliable governmental resources and collected them over a period of 11 years. We also divided the population into adults and children so that Thailand could have data on different age groups, which will be helpful when allocating medical personnel, since children and adults require different types of medical attention.
Another strength of this study is that we showed which hospital resources were the most unequally distributed in order to help prioritise which resources needed to be adjusted first.
The limitations of this paper were that although we had the number of RTMs of each province, we did not know the exact location where the accidents occurred; therefore, we could not assess factors such as road types which have shown to be associated with RTMs. We also did not have details on levels of alcohol consumption or helmet usage in the reported RTMs, both of which affect mortality. We reported RTM rates for children but did not sub-group physicians into paediatricians and emergency department physicians, so that we could not establish how effectively trauma cases are handled in each province. The times at which the accidents occurred were not available, and we did not divide the period into weekdays, weekends, and long holidays, so we were not able to analyse these risk factors of RTMs, as this was not within the scope of the study.
Conclusion
RTM distribution varies across the world and also across different areas within countries; therefore, effective policies and resource adjustments should be based on evidence for each individual nation. We have provided information regarding distribution of RTMs across all the provinces in Thailand, further dividing them into adults and children, who require different types of medical attention. A marked inequality was found between the distribution of RTMs and availability of hospital resources, and we hope that our report will be of use in allocating these resources more appropriately in order to cater for the amount of traffic accidents in each area and lower traffic-related deaths.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Mathers, C., Fat, D. M. & Boerma, J. T. The Global Burden of Disease: 2004 Update (World Health Organization, 2008).
World Health Organization. SDG Target 3.6 Road Traffic Injuries: By 2030, Halve the Number of Global Deaths and Injuries from Road Traffic Accidents. https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/sdg-target-3.6-road-traffic-injuries. Accessed 21 Sep 2022 (2022).
Intersecretariat Working Group on Transport Statistics. Glossary of Transport Statistics/Transmitted Jointly by the Eurostat, UNECE and the European Conference of Ministers of Transport (ECMT): 2003. (United Nations Digital Library, 2003).
Pal, C. et al. An insight of World Health Organization (WHO) accident database by cluster analysis with self-organizing map (SOM). Traffic Inj. Prev. 19(sup1), S15-s20 (2018).
Szymanski, T., Toroyan, T., Iaych, K., Peden, M., Heimann, A., Senisse, A. et al. Global Status Report on Road Safety. (WHO, 2015).
Naci, H., Chisholm, D. & Baker, T. D. Distribution of road traffic deaths by road user group: A global comparison. Inj. Prev. 15(1), 55–59 (2009).
Alibhai, A., Hendrikse, C. & Bruijns, S. R. Poor access to acute care resources to treat major trauma in low- and middle-income settings: A self-reported survey of acute care providers. Afr. J. Emerg. Med. 9(Suppl), S38-s42 (2019).
Shanthakumar, D., Payne, A., Leitch, T. & Alfa-Wali, M. Trauma care in low- and middle-income countries. Surg. J. (N Y). 7(4), e281–e285 (2021).
Genowska, A., Jamiołkowski, J., Szafraniec, K., Fryc, J. & Pająk, A. Health care resources and 24,910 deaths due to traffic accidents: An ecological mortality study in Poland. Int. J. Environ. Res. Public Health 18(11), 5561 (2021).
Chantith, C., Permpoonwiwat, C. K. & Hamaide, B. Measure of productivity loss due to road traffic accidents in Thailand. IATSS Res. 45(1), 131–136 (2021).
Ditsuwan, V., Veerman, L. J., Barendregt, J. J., Bertram, M. & Vos, T. The national burden of road traffic injuries in Thailand. Popul. Health Metrics 9(1), 2 (2011).
Li, L. et al. Legislation coverage for child injury prevention in China. Bull. World Health Organ. 93(3), 169–175 (2015).
Sathya, C. et al. Mortality among injured children treated at different trauma center types. JAMA Surg. 150(9), 874–881 (2015).
Gravelle, H. & Sutton, M. Inequality in the geographical distribution of general practitioners in England and Wales 1974–1995. J. Health Serv. Res. Policy 6(1), 6–13 (2001).
Theodorakis, P. N., Mantzavinis, G. D., Rrumbullaku, L., Lionis, C. & Trell, E. Measuring health inequalities in Albania: A focus on the distribution of general practitioners. Hum. Resour. Health 4, 5 (2006).
Porapakkham, Y. et al. Estimated causes of death in Thailand, 2005: Implications for health policy. Popul. Health Metrics 8, 14 (2010).
Karim, M. et al. Road Safety Status in the WHO South-East Asia Region (WHO, 2013).
Jindal, A.K., & Mukherji, S. World Report on Road Traffic Injury Prevention, M. Peden et al. (World Health Organisation Geneva, 2004) (217, 22 illustrations; soft bound; Rs. 2000, ISBN: 9241562609. Medical Journal Armed Forces India. 2005; 61: 91).
Slesak, G., Inthalath, S., Wilder-Smith, A. & Barennes, H. Road traffic injuries in northern Laos: Trends and risk factors of an underreported public health problem. Trop. Med. Int. Health. 20(11), 1578–1587 (2015).
Ngo, A. D. et al. Road traffic related mortality in Vietnam: Evidence for policy from a national sample mortality surveillance system. BMC Public Health 12, 561 (2012).
Li, Q., Alonge, O. & Hyder, A. A. Children and road traffic injuries: Can’t the world do better?. Arch. Dis. Child. 101(11), 1063–1070 (2016).
Chadbunchachai, W., Suphanchaimaj, W., Settasatien, A. & Jinwong, T. Road traffic injuries in Thailand: Current situation. J. Med. Assoc. Thai. 95(Suppl 7), S274–S281 (2012).
Piyapromdee, M. D. U., Adulyanukosol, M. D. V. & Lewsirirat, M. D. S. Increasing road traffic injuries in underage motorcyclists. J. Southeast Asian Orthopaed. 39(1–2), 3–7 (2022).
Ongkittikul, S., Tantipidok, P. & O-charoen, N. Cost of road accidents involving children in Thailand. TDRI Q. Rev. 24, 12–26 (2014).
Abdul-Razak, S., Azzopardi, P. S., Patton, G. C., Mokdad, A. H. & Sawyer, S. M. Child and adolescent mortality across Malaysia’s epidemiological transition: A systematic analysis of global burden of disease data. J Adolesc Health 61(4), 424–433 (2017).
Chang, S. S. M., Symons, R. C. A. & Ozanne-Smith, J. Child road traffic injury mortality in Victoria, Australia (0–14 years), the need for targeted action. Injury 49(3), 604–612 (2018).
Mokdad, A. A., Wolf, L. L., Pandya, S., Ryan, M. & Qureshi, F. G. Road traffic accidents and disparities in child mortality. Pediatrics 146(5), 20193009 (2020).
Yasin, Y. J., Grivna, M. & Abu-Zidan, F. M. Global impact of COVID-19 pandemic on road traffic collisions. World J. Emerg. Surg. 16(1), 51 (2021).
Shaik, M. E., Hossain, Q. S. & Rony, G. Impact of COVID-19 on public transportation and road safety in Bangladesh. SN Comput. Sci. 2(6), 453 (2021).
World Health Organisation. Powered Two- and Three-Wheeler Safety: A Road Safety Manual for Decision-Makers and Practitioners 2017 (World Health Organization, 2017).
Razzaghi, A. et al. Risk factors of deaths related to road traffic crashes in World Health Organization regions: A systematic review. Arch. Trauma Res. 8, 57 (2019).
HaghparastBidgoli, H., Bogg, L. & Hasselberg, M. Pre-hospital trauma care resources for road traffic injuries in a middle-income country—A province based study on need and access in Iran. Injury 42(9), 879–884 (2011).
Paravar, M. et al. Pre-hospital trauma care in road traffic accidents in Kashan, Iran. Arch. Trauma Res. 1(4), 166–171 (2013).
Mock, C., Arreola-Risa, C. & Quansah, R. Strengthening care for injured persons in less developed countries: A case study of Ghana and Mexico. Inj. Control Saf. Promot. 10(1–2), 45–51 (2003).
Mock, C. N., Jurkovich, G. J., Nii-Amon-Kotei, D., Arreola-Risa, C. & Maier, R. V. Trauma mortality patterns in three nations at different economic levels: Implications for global trauma system development. J. Trauma 44(5), 804–812 (1998) (discussion 12–14).
Montazeri, A. Road-traffic-related mortality in Iran: A descriptive study. Public Health 118(2), 110–113 (2004).
Chokotho, L., Mulwafu, W., Singini, I., Njalale, Y. & Jacobsen, K. H. Improving hospital-based trauma care for road traffic injuries in Malawi. World J. Emerg. Med. 8(2), 85–90 (2017).
Razzak, J. A. et al. Improvement in trauma care for road traffic injuries: An assessment of the effect on mortality in low-income and middle-income countries. Lancet 400(10348), 329–336 (2022).
Yasin, Y. J., Eid, H. O., Alao, D. O., Grivna, M. & Abu-Zidan, F. M. Reduction of motorcycle-related deaths over 15 years in a developing country. World J. Emerg. Surg. 17(1), 21 (2022).
Bishai, D., Quresh, A., James, P. & Ghaffar, A. National road casualties and economic development. Health Econ. 15(1), 65–81 (2006).
La Torre, G., Van Beeck, E., Quaranta, G., Mannocci, A. & Ricciardi, W. Determinants of within-country variation in traffic accident mortality in Italy: A geographical analysis. Int. J. Health Geogr. 6, 49 (2007).
Noland, R. B. Medical treatment and traffic fatality reductions in industrialized countries. Accid. Anal. Prev. 35(6), 877–883 (2003).
Rivas-Ruiz, F., Perea-Milla, E. & Jimenez-Puente, A. Geographic variability of fatal road traffic injuries in Spain during the period 2002–2004: An ecological study. BMC Public Health 7, 266 (2007).
van Beeck, E. F., Borsboom, G. J. & Mackenbach, J. P. Economic development and traffic accident mortality in the industrialized world, 1962–1990. Int. J. Epidemiol. 29(3), 503–509 (2000).
Suriyawongpaisal, P. & Kanchanasut, S. Road traffic injuries in Thailand: Trends, selected underlying determinants and status of intervention. Inj. Control Saf. Promot. 10(1–2), 95–104 (2003).
Sangkharat, K., Thornes, J. E., Wachiradilok, P. & Pope, F. D. Determination of the impact of rainfall on road accidents in Thailand. Heliyon 7(2), e06061 (2021).
Acknowledgements
We would like to acknowledge the assistance of Miss Pawarisa Uthaivoravit, Mister Apipu Sirifah, Miss Warisara Wattanasiripong, Miss Panicha Larpcharoentavee, and Miss Thanachanok Mangma, who helped manage data.
Author information
Authors and Affiliations
Contributions
K.S.: Conceptualization, methodology, formal analysis, writing—original draft. P.S.: Resources, methodology, formal analysis, writing—review and editing. N.S.: Methodology, statistical analysis, writing—review and editing. A.A.: Resources, writing—review and editing. T.T.: Conceptualization, writing—review and editing, supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seresirikachorn, K., Singhanetr, P., Soonthornworasiri, N. et al. Characteristics of road traffic mortality and distribution of healthcare resources in Thailand. Sci Rep 12, 20255 (2022). https://doi.org/10.1038/s41598-022-24811-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-24811-4
This article is cited by
-
The simplified tailor-made workflows for a 3D slicer-based craniofacial implant design
Scientific Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.