Abstract
Poor glycemic control is a main public health problem among type 2 diabetes mellitus (T2DM) patients and a significant cause of the development of diabetic complications. This study aimed to assess the glycemic control status and its associated factors among type 2 diabetes patients in Felege-Hiwot and Debre Markos Referral Hospitals. A retrospective cohort study was conducted at Felege-Hiwot and Debre Markos Referral Hospitals from December 2014 to December 2015. We have reviewed the chart of these patients until January 2020. Type 2 diabetic patients on follow-up at Felege-Hiwot and Debre Markos Referral Hospitals who fulfilled the inclusion criteria of the study were included. The primary outcome was the level of blood glucose during the study period. Good glycemic control was defined as patients whose average fasting blood glucose measurement for three consecutive visits was between 70 and 130 mg/dL. A generalized linear mixed autoregressive order one model was used to identify the determinants of glycemic control. A total of 191 patients with 1740 observations were included in the study. The overall prevalence of good glycemic control was 58.4% (95% CI: 57.159.7%). The factors associated with good glycemic control at 95% confidence level adjusted odds ratio were being residing in rural (CI: 0.454, 0.614), negative proteinuria (CI: 1.211, 1.546), diastolic blood pressure < 90 (CI: 1.101, 1.522), systolic blood pressure < 140 (CI: 1.352, 1.895), serum creatinine (CI: 0.415, 0.660), duration per visit (CI: 0.913, 0.987), duration since diagnosis (CI: 0.985, 0.998), weight ≥ 78 kg (CI: 0.603, 0.881). Age 38–50, 51–59 and 60–66 years (CI: 1.267, 1.776), (CI: 1.057, 1.476) and (CI: 1.004, 1.403), respectively. The overall prevalence of poor glycemic control was high at Debre Markos and Felege Hiwot Referral Hospital. Living in a rural area, older age (≥ 67 years), positive proteinuria, higher weight (≥ 78 kg), higher serum creatinine levels, higher duration per visit, higher time duration of T2DM since diagnosis, and developing hypertension (SBP ≥ 140, DBP ≥ 90) were the predictors of lower good glycemic control achievements of T2DM patients. In response to this finding, an aggressive intervention that targets improving glycemic control is required.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus (T2DM) is a chronic disease. It is defined as high sugar in the blood and results from a defect in insulin secretion, insulin action, or both1,2.
Globally, the prevalence of diabetes was estimated to be 8.3% (6.2–11.8) in 2019 among individuals aged 20–79, including 50.1% who are undiagnosed. It will be 10.2% (8.1–13.2) by 2030. In African Region, with 59.7%, undiagnosed diabetes has a prevalence of 3.9% (2.1–7.1%) among individuals aged 20–79; it will be 4.1% (2.3–7.5%) by 2030. In Ethiopia, the prevalence of diabetes was predicted to be 3.2% of individuals aged 20–79 years in 20191,3. Global burden of disease data suggests diabetes mellitus (DM) may be responsible for 4.2 million individuals aged 20–79 years death in 20191.
T2DM is a rapidly rising non-communicable disease and a public health challenge in Ethiopia with disability and premature death due to the long-term effects of untreated diabetes mellitus1,3. Hence, glycemic control is a means of effectively preventing complications associated with T2DM4. However, the proportion of uncontrolled levels of blood sugar in T2DM was far above the ground in Ethiopia5,6,7,8,9.
The predictors of poor glycemic control were rural residence, age of the patients, duration with diabetes, time duration since diagnosis, drug regimen of oral anti-diabetics or insulin treatment, and body weight5,6,7,8. Yet, there is limited evidence on how these factors are associated with glycemic control using longitudinal data (repeated measured data) even if the glycemic control levels of T2DM patients fluctuate over time. Additionally, previous studies did not assess the influence of proteinuria and creatinine on glycemic control5,6,7,8.
Even if a few longitudinal studies were conducted on the predictors of blood glucose levels using fasting blood glucose levels as a continuous variable9,10,11, the findings of prior studies have not clear recommendations and conclusions about the controlled level of blood sugar of the patients because the negative predictors of fasting blood glucose levels led to hypoglycemia whereas the positive predictors of fasting blood glucose levels also lead to hyperglycemia.
Hence, this study aimed to investigate the glycemic control status and its associated factors among type 2 diabetes patients in Felege-Hiwot and Debre Markos Referral Hospitals using a longitudinal data analysis approach of a generalized linear mixed model. This study accounts for the glycemic control variation of patients over time and thus maximizes the amount of information drawn from the data.
Results
Characteristics of study participants
A total of 191 T2DM patients with 1740 observations were included in the analysis. There were more male patients (61.8%) than females (38.2%). The mean (SD) age of patients at the start of treatment was 57.9 (± 10.5) years. Two-thirds of the patients 144 (75.4) lived in urban areas. About 126 (65.9) and 122 (63.9) of the respondents had developed diabetes complications and hypertension, respectively (Table 1). The overall mean weight of T2DM patients was 73. 29 ± 5.53 Kg, with a minimum of 58 kg and a maximum of 87 kg (Table 1).
The overall mean duration of T2DM patients since diagnosis was 43.25 ± 9.57 months, with a minimum of 6 months and a maximum of 60 months (Table 2).
Prevalence of glycemic control in T2DM Patients
The overall prevalence of uncontrolled glycemic control was 41.6% (95% CI 40.3–42.9%) (Table 2). The overall mean of fasting blood sugar was 137.35mg/dl ± 81.64 (Table 1). The proportion of glycemic control fluctuated over time. Relatively speaking, the prevalence of well-glycemic control progressively rose with follow-up time (Fig. 1). Hence, 23.25% of the variation was explained in the GLMM model due to the incorporation between patient glycemic control variation over time (Table 3).
Factors associated with good glycemic control among T2DM patients
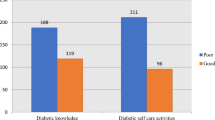
In bivariable analysis, the variable residence, age of the patient, weight, duration of T2DM since diagnosis, duration of T2DM per visit, follow-up time, proteinuria, diastolic blood pressure, systolic blood pressure, and serum creatinine were significantly associated with good glycemic control among T2DM patients at 0.2 level of significance (Table 2).
In multivariable analysis, residence, age, weight, duration of T2DM since diagnosis, duration per visit, follow-up time, proteinuria, diastolic blood pressure, systolic blood pressure, and serum creatinine had significant effects on good glycemic control at 0.05 level of significance (Table 3).
The odds of good glycemic control among patients who lived in rural areas were 47.2% lower compared to those patients who lived in urban areas (AOR 0.528, 95% CI 0.454, 0.614). The odds of good glycemic control for patients whose ages were 38–50, 51–59, and 60–66 years were about 50%, 24.9%, and 18.7% higher as compared with those patients whose ages were 67–80 years old, (AOR 1.500, 95% CI 1.267,1.776), (AOR 1.249, 95% CI 1.057, 1.476) and (AOR 1.187, 95% CI 1.004, 1.403), respectively.
The odds of good glycemic control for negative proteinuria T2DM patients were about 36.8% higher compared to positive proteinuria T2DM patients (AOR 1.368, 95% CI 1.211, 1.546). The odds of good glycemic control were lower by 47.7% when serum creatinine increased by one mg/dl (AOR 0.523, 95% CI 0.415, 0.660).
The odds of good glycemic control among patients whose diastolic blood pressure was < 90 mmHg were about 29.5% higher as compared with those patients whose diastolic blood pressure was ≥ 90 mmHg (AOR 1.295, 95% CI 1.101, 1.522). Similarly, the odds of good glycemic control for patients whose systolic blood pressure was < 140 mmHg were about 60.1% higher compared to those patients whose systolic blood pressure was ≥ 140 mmHg (AOR 1.601, 95% CI 1.352, 1.895).
The odds of good glycemic control for patients whose weights were 78–87 kg were about 27.1% lower compared to those patients whose weights were 58–69 kg (AOR 0.729, 95% CI 0.603, 0.881). The odds of good glycemic control were lower by 5.1% when the duration per visit of the patients increased by one month (AOR 0.949, 95% CI 0.913, 0.987). Likewise, the odds of good glycemic control were lower by 0.8% when the duration since the diagnosis of the patients increased by one month (AOR 0.992, 95% CI 0.985, 0.998).
Discussion
In this study, a generalized linear mixed model with autoregressive order one analysis was used to identify the determinant factors that affected good glycemic control among T2DM patients in two of the major hospitals in North West Ethiopia.
The study revealed that 58.4% of the patients had good glycemic control of blood glucose. The proportion of good glycemic control was comparable to the results reported in the Dilchora Referral Hospital, Ambo, Brazil, Iran, and Jordan5,12,13,14,15. In other studies, approved in Adama Medical College Hospital (35.9%), Ethiopia (31.1%), Referral Hospitals of Amhara Region (44.7%), Riyadh (32.3%), Al-Hasa (32.1%), Jazan (26%), Oman (35%), United Arab Emirates (31%), Kuwait (21.2%) and Rawalpindi (24%), good glycemic control was inferior unlike the current study6,7,8,16,17,18,19,20,21. The observed difference between this and other studies could be because of the difference in sample size, study design (this study used longitudinal data, while other studies used cross-sectional data), and the operational definition used (this study uses fasting blood glucose levels to categorize glycemic control, while other studies use hemoglobin A1c to categorize glycemic control). Besides, the presence of great variation in socioeconomic, cultural, and lifestyle of the study populations across different studies may play a great role in the observed difference.
The odds of good glycemic control among patients who lived in rural areas were 47.2% lower compared to those patients who lived in urban areas. The finding is in line with prior research studies22,23,24 and contradicts with the study conducted in Ethiopia, which reported no significant association between residents with poor glycemic control5,6,7,8,9. A possible reason for this finding might be due to lower awareness of treatment adherence among persons living in rural areas25. Besides, the majority of patients who live in rural areas may have lower educated levels.
The odds of good glycemic control for patients whose ages were 38–50, 51–59, and 60–66 years were about 50%, 24.9%, and 18.7% higher as compared with those patients whose ages were 67–80 years old, respectively. This finding agrees with the findings from India and Ethiopia8,26 and contradicts the study conducted in Ethiopia, which reported no significant association between age with poor glycemic control5,6,7. The possible cause for this finding is because of the happening of diabetes-related complications within higher ages27. This implies that older age not only increases the hazard of chronic illness; the supervision of the illnesses also becomes difficult.
The odds of good glycemic control for negative proteinuria T2DM patients were about 36.8% higher compared to positive proteinuria T2DM patients. The justification for this study is that positive proteinuria was an increasing the risk of vascular complications9, which may lead to poor glycemic control28,29.
The odds of good glycemic control decreased by 47.7% when serum creatinine increased by one mg/dl. The reason for this study is that increasing serum creatinine leads to an increase in the risk of vascular complications9, which leads to poor glycemic control28,29.
Patients whose diastolic blood pressure was < 90 mmHg had higher odds of good glycemic control compared to those patients whose diastolic blood pressure was ≥ 90 mmHg. Similarly, patients whose systolic blood pressure was < 140 mmHg had higher odds of good glycemic control compared with those patients whose systolic blood pressure was ≥ 140 mmHg. This result agrees with previous findings8,9,30,31 and contradicts the study conducted in Ethiopia, which reported no significant association between blood pressure control with poor glycemic control7. The possible justification for this study is due to the additional antihypertensive pill burden and the complication inhibiting the utilization of peripheral glucose, which finally increases the fasting blood glucose level32.
The odds of good glycemic control were lower by 5.1% when the duration per visit of the patients increased by one month. Likewise, the odds of good glycemic control were lower by 0.8% when the duration since the diagnosis of the patients increased by 1 month. This study is in line with the findings of the previous study8 and contradicts the study conducted in Ethiopia, which reported no significant association between duration since diagnosis in patients with poor glycemic control5,6,7. The possible justification for this study is that progressive impairment of insulin secretion through time because β cell failure could lead to poor glycemic control.
Patients whose weights were 78–87 kg had lower odds of good glycemic control compared to those patients whose weights were 58–69 kg. This finding was supported by previous studies6,7,8,30 and contradicts the study conducted in Ethiopia, which reported no significant association between the weight of patients with poor glycemic control5,9. The possible justification is that higher weight will increase blood sugar and increase the risk of diabetes complications.
The main limitation of the study is the limited information on predictors: such as family history, medication adherence, patients’ perception of health, the type of intervention, including the type of physical exercise, and nutritional status of a patient that may have influenced the outcome variables. Due to a lack of data on these predictors, we have excluded them from the analyses. Therefore, more public health and epidemiology research is needed to examine the impact of these variables to identify new risk factors of glycemic control for T2DM patients by using the HbA1c test, which is a good predictor of glycemic control over a long time.
Conclusions and recommendations
This study revealed that the overall prevalence of poor glycemic control was high at Debre Markos and Felege Hiwot Referral Hospital. Living in a rural area, older age (≥ 67 years), positive proteinuria, higher weight (≥ 78kg), higher serum creatinine levels, higher duration per visit, higher time duration of T2DM since diagnosis, and developing hypertension (SBP ≥ 140, DBP ≥ 90) were the predictors of lower good glycemic control achievements of T2DM patients. Therefore, strengthening and disseminating health education programs for diabetes patients at each follow-up visit on the importance of achieving optimal body weight, negative proteinuria, and controlling blood pressure to prevent and mitigate the complications resulting from poor glycemic control. Health professionals working in the hospital should provide good patient advice for type 2 DM patients: living in the rural area, older age (≥ 67 years), with higher serum creatinine levels, higher duration per visit and higher time duration of T2DM since diagnosis to maximize efforts on the prevention of T2DM complications and risk minimization resulting from poor glycemic control.
Methods
Study design, study area, and study period
An institutional-based retrospective follow-up study design was conducted at Felege-Hiwot and Debre Markos Referral Hospital with type 2 diabetes mellitus patients who were enrolled from December 2014 to December 2015. We have reviewed the chart of these patients until January 2020.
Felege-Hiwot Referral Hospital (FHRH) is found in Bahir Dar, the capital city of the Amhara Regional State, a region in the Northwest of Ethiopia, whereas Debre Markos Referral Hospital (DMRH) is found in Debre Markos, the capital city of East Gojjam zone, a region in the Northwest of Ethiopia.
These hospitals were selected because they are the only referral hospitals under the thematic research area of the finder (Debre Markous University). Besides, we expected that the chance of getting more recorded valid information was better than other non-referral hospitals because of the presence of experienced staff and modern laboratory equipment. As a result of this, we have selected those hospitals over others, purposively. In addition, these hospitals were geographically 264 km away. Thus, it is more likely to get an adequate size of type 2 diabetic patients from different socio-cultural and environmental conditions.
Source and study population
The source population was all T2DM patients who were found at Felege-Hiwot and Debre Markos Referral Hospitals, whereas the study population was all type 2 diabetic patients aged 18 years or older who came to the hospital for diagnosis and follow-up from December 2014 to December 2015. We have reviewed the chart of these patients until January 2020. A total of 191 patients, who fulfilled the inclusion criteria of the study, with 5220 observations of FBS repeatedly measured values were changed in to 1740 glycemic control status observations. Since, we have used each of the three consecutives measured FBS to determine the glycemic control status of the patients.
Inclusion and exclusion criteria
T2DM patients with three fasting blood glucose measurements within three months and above the age of 18 years were included in the study, whereas the patient chart would not be available during the data collection period and patients with missing key predictor variables were excluded from the study. Finally, 191 T2DM patients met the inclusive critter of the study, whereas 138 T2DM patients were excluded from the study (Fig. 2).
Study variables
The dependent variable was glycemic control status. The independent variables were socio-demographic variables (age, sex, residence), clinical characteristics (weight, duration of DM since diagnosis, duration per visit, specific type of drug regimen, comorbidity, DM complications), and physiological characteristics (creatinine, Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), and proteinuria).
Operational definitions
Fasting Blood Sugar is blood glucose measured from venous blood after at least 8 hours of overnight fasting33.
Good glycemic control was defined as patients whose average fasting blood glucose measurement of three consecutive visits was between 70 and 130 mg/dL33,34.
Poor glycemic control was defined as patients whose average blood glucose measurement for three consecutive visits was above 130 or below 70 mg/dL33,34.
Protein urea is defined as positive if the urine albumin concentration is between 30 mg/24 h and 300 mg/24 h and negative if it is < 300 mg/ 24 h9.
Data collection procedures and data quality control
Data were extracted by reviewing patient charts using a checklist. The data were collected by two nurses who had experience in diabetic follow-up and the required laboratory values were taken from the patient’s medical record. To control data quality, training was given to the data collectors and their supervisors. The data extraction checklist was pretested for consistency of understanding of the review tools and completeness of data items. The necessary adjustments were made to the final data extraction format. Finally, the filled formats were checked daily by the supervisor.
Ethics approval and consent to participate
Ethical approval was obtained from the Natural and Computational Science College Research Ethics Committee (Debre Markos University), and permission was obtained from the medical directors of the Hospital. We confirm that all methods were carried out by relevant guidelines and regulations. Due to the retrospective nature of the study, the need for informed consent was waived by the Research Ethics Committee of Natural and Computational Science College (Debre Markous University), but the data were anonymous and kept confidential.
Data analysis
Descriptive statistics were used to describe the percentage and frequency of patients with all covariates. In addition, a line graph was used to see the progression of glycemic control over time. A generalized linear mixed model with autoregressive order one covariance structure was used to identify the predictors of glycemic control among type 2 diabetic patients because AR(1) covariance structure has the best covariance structure than others in the current study. Since, it has the smallest AIC and BIC than other covariance structures (Table 4). The odds ratio was used to assess the association between glycemic control and risk factors. The 95%CI that did not include one or a P-value less than 5% was taken to identify a significant association between glycemic control and risk factors.
Generalized linear mixed model
We used the extension of multiple binary logistics regression to include both fixed and random effects (subjects) in the generalized linear mixed model because the dependent variable had dichotomous natures as well as we have cheeked that there was no dispersion parameter in the data. GLMMs are generally defined such that, conditioned on the random effect \(\upsilon\), the dependent variable \(Y (\mathrm{glycemic control for the }{\mathrm{i}}^{\mathrm{th}}\mathrm{ type }2\mathrm{ diabetes }{\mathrm{patient}}^{\mathrm{^{\prime}}}\mathrm{s}),\) is distributed to a binomial distribution with its expectation related to the linear predictor \(X\beta +Zu\) via a logit link function \(g\):
Here X and β are the fixed effects design matrix, and fixed effects; Z and u are the random effects design matrix and random effects. Generalized linear mixed models enabled us to see heterogeneity between patients.
Parameter estimation for generalized linear mixed models
The marginal quasi-likelihood method was used to estimate the model parameters. The complete likelihood for all observed data is formulated as35
The likelihood function has no general closed-form, and integrating over random effects is usually extremely computationally intensive. In addition to numerically approximating this, integral, methods motivated by Laplace approximation have been proposed36.
To build the generalized linear mixed model analysis, using the procedure we followed, first, we did a bivariable analysis for each of the explanatory variables and based on statistical significance at 0.2 level of significance, the identified variables to be candidates for the multivariable analysis37. As naturally different identified factors/variables do not operate separately, multivariable analysis helps to control for confounders and analyze the effects of a factor in the presence of other factors in the model.
We used Akaike and Bayesian information criteria to select the appropriate generalized linear mixed model with its best covariance structure, and the model with the smallest AIC or BIC was considered the best fit38,39.
Data availability
The data sets analyzed in this study are available from the corresponding author on reasonable request.
Abbreviations
- ADA:
-
America Diabetes Association
- AIC:
-
Akaike information criteria
- AOR:
-
Adjusted odds ratio
- BIC:
-
Bayesian information criteria
- CHD:
-
Coronary heart disease
- CI:
-
Confidence interval
- COR:
-
Crude odds ratio
- DBP:
-
Diastolic Blood pressure
- DM:
-
Diabetes Mellitus
- DMRH:
-
Debre Markos Referral Hospital
- FHRH:
-
Felege-Hiwot Referral Hospital
- GLMM:
-
Generalized linear mixed model
- IDF:
-
International Diabetes Federation
- PAD:
-
Peripheral arterial disease
- SBP:
-
Systolic Blood pressure
- T2DM:
-
Type 2 Diabetes Mellitus
References
IDF. Diabetes Prevalence in 2019 and Projections to 2030 and 2045(20–79 years) (IDF DIABETES ATLAS, 2019).
Cefalu, W. T. et al. Classification and diagnosis of diabetes: Standards of medical care in diabetes-2019. Diabetes Care 42, S13–S28 (2019).
IDF. IDF Africa Members - International Diabetes Federation (2020).
Reaven, P. D. et al. Intensive glucose control in patients with type 2 diabetes—15-year follow-up. N. Engl. J. Med. 380(23), 2215–2224 (2019).
Nigussie, S. et al. Rate of glycemic control and associated factors among type two diabetes mellitus patients in Ethiopia: A cross sectional study. PLoS ONE 16(5), e0251506 (2021).
Yosef, T., Nureye, D. & Tekalign, E. Poor glycemic control and its contributing factors among type 2 diabetes patients at Adama Hospital Medical College in East Ethiopia. Diabetes Metab. Syndr. Obes. 14, 3273 (2021).
Demoz, G. T. et al. Predictors of poor glycemic control among patients with type 2 diabetes on follow-up care at a tertiary healthcare setting in Ethiopia. BMC. Res. Notes 12(1), 1–7 (2019).
Feleke, B. E. et al. Glycemic control of diabetes mellitus patients in referral hospitals of Amhara Region, Ethiopia: A cross-sectional study. BioMed Res. Int. 20, 21. https://doi.org/10.1155/2021/6691819 (2021).
Shita, N. G. & Muluneh, E. K. Predictors of blood glucose change and vascular complication of type 2 diabetes mellitus patients in Felege Hiwot Referral Hospital, North West Ethiopia. Sci. Rep. 11(1), 1–9 (2021).
Andargie, A. A. & Zeru, M. A. A longitudinal data analysis on risk factors for developing type-2 diabetes mellitus at the University of Gondar Comprehensive Specialized Hospital, Gondar, Ethiopia. J. Public Health Epidemiol. 10(6), 171–182 (2018).
Aniley, T. T., Debusho, L. K., Nigusie, Z. M., Yimer, W. K. & Yimer, B. B. A semi-parametric mixed models for longitudinally measured fasting blood sugar level of adult diabetic patients. BMC Med. Res. Methodol. 19(1), 1–11 (2019).
Lozovey, N. R., Lamback, E. B., Mota, R. B., Caarls, M. B. & Neto, L. V. Glycemic control rate in type 2 diabetes mellitus patients at a public referral hospital in Rio de Janeiro, Brazil: demographic and clinical factors. J. Endocrinol. Metabo. 7(2), 61–67 (2017).
Woldu, M. A. et al. Factors associated with poor glycemic control among patients with type 2 diabetes mellitus in Ambo Hospital, Ambo; Ethiopia. Endocrinol. Metab. Synd. 3(143), 2161–1017 (2014).
Mohammadi, S., Karim, N. A., Talib, R. & Amani, R. Knowledge, attitude and practices on diabetes among type 2 diabetic patients in Iran: a cross-sectional study. Science 3(4), 520–524 (2015).
Lumanlan, D. B. & Quiaoit-Alegarbes, S. Knowledge, attitudes and practices and its association with glycemic control among type 2 diabetes mellitus patients in a tertiary hospital. Diabetes Res. Clin. Pract. 1(120), S175 (2016).
Al-Rasheedi, A. A. Glycemic control among patients with type 2 diabetes mellitus in countries of Arabic Gulf. Int. J. Health Sci. 9(3), 345 (2015).
Badedi, M. et al. Factors associated with long-term control of type 2 diabetes mellitus. J. Diabetes Res. 2016, 1–8 (2016).
Al-Rasheedi, A. A. S. The role of educational level in glycemic control among patients with type II diabetes mellitus. Int. J. Health Sci. 8(2), 177 (2014).
Khan, A. R. et al. Factors contributing to non-compliance among diabetics attending primary health centers in the Al Hasa district of Saudi Arabia. J. Fam. Community Med. 19(1), 26 (2012).
Al-Kaabi, J. et al. Assessment of dietary practice among diabetic patients in the United Arab Emirates. Rev. Diabetic Stud. 5(2), 110 (2008).
Al-Ibrahim, A. A. H. Factors Associated with Compliance to Diabetes Self-care Behaviors and Glycemic Control Among Kuwaiti People with Type 2 Diabetes (University of Maryland, 2012).
Fseha, B. Glycemic control and it’s associated factors in type 2 diabetic patients in Suhul Hospital, Northwest Tigray, Ethiopia. J. Diabetes Metab. 8(3), 729 (2017).
Abebe, S. M., Berhane, Y., Worku, A., Alemu, S. & Mesfin, N. Level of sustained glycemic control and associated factors among patients with diabetes mellitus in Ethiopia: a hospital-based cross-sectional study. Diabetes Metab. Syndr. Obes. 8, 65 (2015).
Fiseha, T., Alemayehu, E., Kassahun, W., Adamu, A. & Gebreweld, A. Factors associated with glycemic control among diabetic adult out-patients in Northeast Ethiopia. BMC. Res. Notes 11(1), 1–6 (2018).
Supiyev, A. et al. Diabetes prevalence, awareness and treatment and their correlates in older persons in urban and rural population in the Astana region, Kazakhstan. Diabetes Res. Clin. Pract. 112, 6–12 (2016).
Borgharkar, S. S. & Das, S. S. Real-world evidence of glycemic control among patients with type 2 diabetes mellitus in India: The TIGHT study. BMJ Open Diabetes Res. Care 7(1), e000654 (2019).
Laiteerapong, N. et al. The legacy effect in type 2 diabetes: Impact of early glycemic control on future complications (the Diabetes & Aging Study). Diabetes Care 42(3), 416–426 (2019).
Afroz, A., Zhang, W., Loh, A. J. W., Lee, D. X. J. & Billah, B. Macro-and micro-vascular complications and their determinants among people with type 2 diabetes in Bangladesh. Diabetes Metab. Syndr. 13(5), 2939–2946 (2019).
de Oliveira, R. E. M. & Franco, L. J. Glycemic control in elderly people with type 2 diabetes mellitus attending primary health care units. Prim. Care Diabetes 15, 733–736 (2021).
Ismail, M. F. S., Fares, M. M. & Abd-Alrhman, A. G. Prevalence of depression and predictors of glycemic control among type 2 diabetes mellitus patients at family medicine clinic, Suez Canal University Hospital Egypt. Middle East J. Fam. Med. 7(10), 4–13 (2019).
Wang, J. et al. Status of glycosylated hemoglobin and prediction of glycemic control among patients with insulin-treated type 2 diabetes in North China: a multicenter observational study. Chin. Med. J. 133(1), 17 (2020).
MacKenzie, J. D. Role of Anti-hypertension Class Drugs in the Pathogenesis of Diabetes Mellitus Complications (Boston University, 2019).
ADA. American Diabetes Association. Glycemic targets: Standards of medical care in diabetes 2020. Diabetes Care 43(S1), S66–S76. https://doi.org/10.2337/dc20-S006 (2020).
ADA. Classification and diagnosis of diabetes: standards of medical care in diabetes—2018. ADA Diabetes Care J. Clin. Appl. Res. Educ. 41(S1), S13–S27 (2018).
Pawitan, Y. In All Likelihood: Statistical Modelling and Inference Using Likelihood (Oxford University Press, 2001).
Breslow, N. E. & Clayton, D. G. Approximate inference in generalized linear mixed models. J. Am. Stat. Assoc. 88(421), 9–25 (1993).
Hosmer, D. W. & Lemeshow, S. Applied Survival Analysis: Time-to-Even (Wiley-Interscience, 1999).
Akaike, H. A new look at the statistical model identification. IEEE Trans. Autom. Control 19(6), 716–723 (1974).
Schwarz, G. Estimating the dimension of a model. Ann. Stat. 6(2), 461–464 (1978).
Acknowledgements
We would like to greatly acknowledge Debre Markos and Felege Hiwot Referral Hospital for allowing us to use the T2DM Patient data. Debre Markous University is gratefully acknowledged for financially supporting this work.
Funding
The source of funding for this research is Debre Markous University (Grant no. DMU/NCS).
Author information
Authors and Affiliations
Contributions
N.G. conceived the study, formulated the design, drafted the manuscript, analyzed, and interpreted the data. A.S. participated in the conception of the study and revised the manuscript critically for important intellectual content. All authors have read and approved the manuscript for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shita, N.G., Iyasu, A.S. Glycemic control and its associated factors in type 2 diabetes patients at Felege Hiwot and Debre Markos Referral Hospitals. Sci Rep 12, 9459 (2022). https://doi.org/10.1038/s41598-022-13673-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-13673-5
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.