Abstract
Radiotherapy after breast conserving surgery and mastectomy with node positive disease has been shown to reduce risk of recurrence and mortality in the treatment of breast cancer. Intensity-modulated radiation therapy (IMRT) after conservative surgery offers several advantages over conventional RT including improved acute and late toxicity and quality of life (QoL). We undertook this study to prospectively evaluate acute (≤90 days after last dose of radiotherapy) and long-term (>90 days) cutaneous, esophageal, and fibrosis toxicity and QoL in breast cancer patients treated by adjuvant IMRT after breast surgery. We included patients with complex volumes for which 3D RT does not allow a good coverage of target volumes and sparing organs at risk. We report here an interim analysis with a median follow-up of 13.1 months (range, 6.5–25.9 months). Most of the acute toxicity was cutaneous (95.9%) and oesophageal (59.6%), and mostly grade 1 and 2. Medium-term cutaneous toxicity rate was 25.6%, and mostly grade 1. Medium-term esophageal toxicity was rare (1.8%). In this series acute oesophageal toxicity was found to be associated with dosimetric factors. QoL was well preserved throughout the study, and aesthetic outcomes were good. Based on these data, tomotherapy may be a favorable alternative to other techniques in patients needing a complex irradiation of the breast and lymph node volumes.
Similar content being viewed by others
Introduction
Radiotherapy is recommended after breast conserving surgery and mastectomy with node positive disease in the treatment of breast cancer. A meta-analysis of data from over 10,000 women revealed that adjuvant radiotherapy reduces risk of recurrence by up to 15% and 15-year mortality rates by 4% in the treatment of breast cancer after breast-conserving surgery1. After total mastectomy, in the event of local lymph node invasion, radiotherapy allows reducing recurrence in up to 10% and the 20-year mortality rate in up to 8% of the cases, regardless of the number of invaded nodes1.
Adjuvant radiotherapy in the treatment of breast cancer, however, can result in acute and late adverse events. Acute toxicity affects notably the skin and esophagus, while late toxicity includes cosmetic and functional sequelae, lung fibrosis, cardiovascular toxicity and secondary cancers2,3,4,5,6.
3D conformational radiotherapy (3D-CRT) is the standard treatment but it presents some disadvantages including dose inhomogeneity leading to increased acute reactions, inadequate cosmetic outcomes7, organs at risk (OAR) toxicity and local recurrence risk8, as well as complex treatment settings in cases of associated lymph node irradiation.
Three recent randomized trials have demonstrated that intensity-modulated radiation therapy (IMRT) after conservative surgery offers several advantages over conventional RT including improved acute and late breast toxicity and quality of life (QoL)9,10,11,12,13. These trials, however, suffered from some limitations: included patients had an early stage breast cancer; treatment in the control arm was 2D-CRT, which is no longer the therapeutic standard; intervention in the experimental arm constituted a simplified IMRT technique; and few data were reported on local control and none on survival or late toxicity other than aesthetics.
Compared to 3D-CRT, IMRT allows covering target volumes while sparing OAR when radiating complex shapes. Even though the use of IMRT is increasing, a lack of available clinical data, notably regarding rotational IMRT, precludes its use in routine care14. Furthermore, IMRT increases the volume receiving low-dose with uncertainty regarding its long-term implications
The aim of this study was to evaluate acute and medium-term breast, cutaneous and esophageal toxicity in breast cancer patients treated by adjuvant IMRT. Secondary objectives were to analyze the association between clinical and dosimetric characteristics and toxicity, to evaluate QoL and aesthetic outcomes, and to compare the toxicity of the different delineation protocols used.
Methods
This was a single-centre, prospective evaluation of the tolerance of adjuvant IMRT by tomotherapy in the treatment of breast cancer patients after breast surgery within routine care (ClinicalTrials.gov Identifier: NCT02281149). The study was approved by the local ethics committee (“Comité de Protection des Personnes Nord Ouest IV”) and conducted in accordance with the Helsinki declaration and good clinical practice guidelines. Informed consent was obtained from all patients. Inclusion criteria were patients ≥18 years, with histologically proven breast cancer, undergoing adjuvant radiotherapy after partial or total mastectomy, with or without irradiation of axillary lymph nodes. Patients with metastatic disease, presenting a severe or non-controlled pathology that could compromise participation in this trial, breast-feeding or pregnant, and unable to undergo medical follow-up for geographical, social or psychological reasons were excluded.
Treatment procedure
Target and OAR volume delineation were performed according to ASTRO guidelines15 until January 2016 and ESTRO guidelines16 thereafter. A 5-mm margin was added to the clinical target volume (CTV) to obtain the planning target volume (PTV).
Prescribed dose to the breast/chest wall/axillary lymph nodes was 50 Gy (25 fractions x 2 Gy) to the breast over five weeks (5 irradiations/week) with simultaneous integrated boost (SIB) at surgical bed (PTV-boost) of 60 Gy in 25 fractions (25 fractions x 2.4 Gy) after conservative treatment. The goal of the prescription was that 95% of the volume received 95% of the prescribed dose.
The treatment procedure has been described previously17,18.
Endpoints
The primary endpoint of the study was acute (≤90 days after last dose of radiotherapy) and long-term (>90 days) toxicity related to radiotherapy, determined according to NCI-CTCAE v4.0 criteria. Studied toxicities included cutaneous toxicity (described by the terms radiodermatitis, ulceration-necrosis, telangiectasia, atrophy, hyperpigmentation and hypopigmentation), esophageal toxicity, and breast fibrosis. Toxicities were assessed at baseline, during RT (one/week), at 1 and 6 months, and at 1, 2, 3, 4, 5 years post-radiotherapy. Acute toxicity was reported during radiotherapy and at 1-month follow-up. Medium-term toxicity was reported at 6-month follow-up or after. Secondary endpoints were QoL (evaluated by the EORTC QLQ-C30 and BR-23 questionnaires), aesthetic outcomes (coded as poor, medium, good, excellent and collected from the physician and the patient) and recurrence-free survival (RFS).
Instruments for QoL
The EORTC QLQ-C30, is a cancer-specific measure of HRQOL. EORTC QLQ-C30 and QLQ-BR23 scorings were performed according to the EORTC manual19. Scores were linearly transformed to a 0-to-100 scale. A high or healthy level of functioning was represented by a high functional score. A high QoL is represented by a high score for global health status or QoL. More severe symptoms are expressed by higher scores in symptoms scales.
Statistical considerations
Statistical analyses were performed using Stata 13.1 (StataCorp. 2013, College Station, Texas, USA).
Patient characteristics are presented using descriptive variables: frequencies and percentages for categorical variables; medians and ranges, and means and standard deviations (sd) for continuous variables. Cutaneous toxicity and fibrosis were measured per treated breast to include bilateral cancers. Esophageal toxicity was analyzed per patient. Acute toxicity was estimated as frequency and percentages by grade and toxicity type. Cumulative incidence of medium-term toxicity was estimated by the Kaplan-Meier method considering the time-lapse between the end of RT and the occurrence of late toxicity. Patients not presenting any toxicity were censored at the date of last news.
An analysis of the association between clinical and dosimetric characteristics and acute or medium-term cutaneous or esophageal toxicities was performed. Clinical parameters tested for cutaneous toxicity were age, BMI, breast volume, smoking status, diabetes, esthetical results prior to radiotherapy and prior chemotherapy. Dosimetric parameters tested for cutaneous toxicity were mean dose received (Dmean) and dose (Gy) received by 2, 50, 95, 98% of the volume (D2%, D50%, D95%, D98%) for the target volumes (breast, susclavian and subclavian), skin, susclavian and subclavian skin areas; volume (cc) of the target and skin areas, volume (cc) of the breast target volume receiving 95% of the dose (V95%). Clinical parameters tested for esophageal toxicities were age, BMI, smoking status, diabetes and prior chemotherapy. Dosimetric parameters tested for toxicity to the esophagus were volume of the esophagus, Dmean, D2%, D50%, D95%, D98%, volume (cc) of the esophagus that received a dose of 30 or 45 Gray (V30 Gy, V45 Gy). The analysis was performed on the overall population and on the total and partial mastectomy subgroups for cutaneous toxicities.
The association between acute toxicity considered as a binary variable with clinical and dosimetric characteristics was analyzed for qualitative variables with the chi-2 test or the Fisher exact test in case of a small sample. For quantitative variables we used the Student’s t-test if normality of variables or sample ≥30 or the Wilcoxon Mann-Whitney test otherwise. A multivariate analysis was then performed using logistical regression model.
The association between medium-term toxicity, considered as a time-to-event variable, with clinical and dosimetric characteristics was analyzed for qualitative variables with a Logrank test and for quantitative variables with a Cox univariate model. A multivariate analysis was performed using a multivariate Cox model.
For the selection of parameters to include in multivariate logistical and Cox regression models, variables significantly associated to toxicity (p < 0.05), or not significantly associated but with a p < 0.10 in univariate analysis were taken into account. In the case of highly correlated parameters (r² > 0.70), only the one associated to the endpoint with a better Akaike’s information criteria (lower AIC) was included in the multivariate model to avoid collinearity. A multivariate backward stepwise selection procedure was performed to keep only variables associated to toxicity with p < 0.05 and to remove variables insufficiently associated to the endpoint from the final multivariate model.
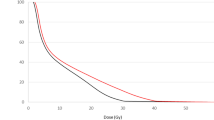
An exploratory analysis was performed to evaluate the association between acute esophageal toxicity and the whole range of dose received by percentage of the esophageal volume (from D1% to D100% (Gy)) using the Wilcoxon Mann-Whitney test.
RFS was estimated using the Kaplan-Meier method and was defined as the time between inclusion and the first sign of disease recurrence or death. Patients alive and recurrence-free at last follow-up were censored at the date of last news.
Scores corresponding to QLQ-C30 and BR23 were described with median, ranges, mean and sd values; score differences between different time-points and inclusion were also calculated. Score changes over time were evaluated with variance analyses variances for repeated measures.
Results
One hundred and nineteen patients were included in Centre Oscar Lambret (Lille, France) between November 2014 and April 2016. Five patients left the study prematurely (n = 2 patient decision, n = 1 decision of the investigator, n = 1 change of RT technique, n = 1 disease progression). Baseline patient and tumor characteristics are presented in Table 1.
The median dose prescribed to the breast/chest wall/axillary nodes PTV was 50 Gy (range, 40.0–50.5 Gy) and a median simultaneous boost to the surgical bed of 10 Gy (range, 9.6–15.0 Gy). Table 2 presents the treatment administered to patients.
Median treatment time was 36 days (range, 21–44 days), and median follow-up 13.1 months (range, 6.5–25.9 months) since the start of RT and 11.9 months (range 5.4–24.7 months) since the end of RT.
Table 3 presents toxicity incidences by maximum grade. Most common acute skin toxicities were radiodermitis (109/121, 90.1%) and hyperpigmentation (82/121, 67.8%), which were mostly grade 1 (80/121, 66.1%). There were two grade 3 acute radiodermitis. Most common medium-term toxicities were hyperpigmentation (9/121, 7.4%), atrophia (8/121, 6.6%) and telangiectasis (8/121, 6.6%). The only case of medium-term grade 3 toxicity was a ulceration-necrosis. The maximum acute esophageal toxicity was grade 1 in 59/114 (51.8%) patients and grade 2 in 9/114 (7.9%) patients. Medium-term esophageal toxicity was rare with 2/114 (1.8%) patients experiencing grade 1 events. Forty-six of 114 (38.0%) patients experienced acute fibrosis, none grade 2. Medium-term fibrosis of grade 2 was reported by 8/114 (6.6%) patients.
One-year cumulative incidences of medium-term grade ≥2 skin and esophageal toxicity, and grade ≥2 fibrosis were 4.1% (95% CI, 1.1–15.6), 8.7% (95% CI, 4.3–17.3) and 0%, respectively.
Multivariate analysis revealed a significant association between skin grade ≥2 acute toxicity and BMI (p = 0.003; OR = 1.14, 95% CI, [1.04–1.24]), dose received by 95% of the skin volume (D95%) (p = 0.033; OR = 1.11, 95% CI, [1.01–1.22]) and susclavian skin D98% (p = 0.034; OR = 1.04, 95% CI [1.003–1.09]) (Table 4). In the total mastectomy sub-group analysis, a higher D98% susclavian skin value was associated with a higher risk of developing skin grade ≥2 acute toxicity (p = 0.013; OR = 1.07, 95% CI [1.016–1.135]). In the partial mastectomy group, skin grade ≥2 acute toxicity was significantly associated with BMI (p = 0.015; OR = 1.17, 95% CI [1.03–1.32]) and chemotherapy (p = 0.001; OR = 0.09, 95% CI [0.02–0.39]). Not enough events were recorded to perform association analyses with skin grade ≥2 medium-term toxicities. Only volume of subclavian skin was associated with skin grade ≥1 medium-term toxicity (p = 0.049; HR = 1.02, 95% CI [1.00–1.05]) (Table 5). In the total and partial mastectomy subgroups, not enough events occurred to perform multivariate analyses.
No factor among those listed in Table 6 was significantly associated to acute grade ≥2 esophageal toxicity in univariate analysis. The percentage of esophagus volume receiving ≥30 Gy (V30) was at the limit of significance (p = 0.055). In univariate analysis, acute grade ≥1 esophageal toxicity was significantly associated to esophageal D2% (p = 0.0004; mean D2% = 43.1 Gy [sd 5.9] in patients with toxicity vs 37.2 Gy [sd 9.3] in patients without toxicity), esophageal mean dose (Dmean) (p = 0.009; mean Dmean = 14.5 Gy [sd 3.2] vs 13.1 Gy [sd 3.0]), esophageal V30 (p = 0.016; mean V30 Gy = 16.5% [sd 8.8] vs 11.1% [sd 9.1]) and esophageal V45 (p = 0.006; mean V45 Gy = 3.0% [sd 3.7] vs 1.5% [sd 2.8]), with a higher dose and a higher volume associated with a higher risk of grade ≥1 toxicity. These parameters were too highly correlated with each other to be included in a multivariate model.
The exploratory analysis for the association between acute esophageal toxicity and the dose received by percentage of the esophageal volume ranging from 1 to 100% (Gy) revealed a significant association between acute grade ≥2 esophageal toxicity and dose ranging from D7% to D36%, and between acute grade ≥1 esophageal toxicity and dose ranging from D1% to D30%.
QoL questionnaires were completed by 84.3% of patients at baseline, 86.8% at 1 month, 79.6% at 6 months and 73.9% at 1 year. Table 7 presents the scores at each time-point and the results for variance analyses for items related to local RT treatment.
Global health status scores at 1-, 6- and 12-month follow-up were significantly higher than at inclusion (p < 0.0001), representing a higher level of QoL. Scores of global health status did not differ significantly during follow-up.
Body image scores improved significantly at 1 month, 6 months and 1 year compared to inclusion, reflecting a better body image. The score at 1 year was significantly higher than that at 1 month.
Score for breast symptoms at 1-month follow-up was significantly higher than that at inclusion, reflecting a worsening of symptoms. Scores at 6 months and 1 year were significantly lower than at 1 month, and did not differ significantly from those at inclusion.
At 1-year post RT, 21/37 patients (56.8%) experienced good aesthetic results, followed by 11/37 (29.7%) experiencing excellent results and 5/37 (13.5%) reporting moderate outcomes. Patient reported outcomes were in line with those reported by the physician (18/34 [52.9%] good outcomes, 10/34 [29.4%] excellent and 6/34 [17.6%] moderate).
The median follow-up (13.1 months) was too short to estimate late toxicity and RFS; only two recurrences and no death were reported.
Discussion
Many have reported on the benefit of using a simultaneous boost to the tumor bed in reducing treatment time without compromising local control20,21,22,23,24. Tomotherapy is an improved radiation technique that allows for a better tumor coverage and sparing normal tissue in lungs and heart from high radiation doses compared to 3D-CRT.
Nevertheless, not many reports exist on the acute and late toxicity profiles of this technique in patients undergoing RT after lumpectomy or mastectomy. To our knowledge, this is one of the largest prospective series assessing the effect of a short strategy of 25 fractions with SIB in the tumor site on acute and medium-term toxicities, and QoL.
This study included patients with complex volumes for which 3D RT does not allow a good coverage of target volumes and sparing OARs. Most of the acute toxicity was cutaneous (95.9%) and oesophageal (59.6%), and mostly grade 1 and 2.
In most breast IMRT studies, lymph node areas and the esophagus were spared, and only a few have reported on oesophageal toxicity. Caudrelier et al. carried out a study of IMRT delivered by helical tomotherapy for locoregional breast radiation. Esophageal toxicity (dysphagia from esophagitis) was found in 37% of the 30 patients and was grade 125. Aoulad et al. have recently reported the acute toxicity profile of intensity modulated helical tomotherapy during breast cancer irradiation after conserving surgery or mastectomy26. Acute grade 1–2 esophageal toxicities occurred in 19.9% of 292 patients. The lower rate in these studies could be attributed to the smaller sample size in the first one and the retrospective character in Aoulad’s study. Retrospective studies are known to minimize toxicity, particularly the low-grade toxicities that are most common in our study.
To our knowledge, this is the first series to describe a correlation between acute esophageal toxicity and dosimetric factors in this setting. In univariate analysis, acute grade ≥1 esophageal toxicity was significantly associated to esophageal D2% (p = 0.0004), Dmean (p = 0.009), V30 (p = 0.016) and V45 (p = 0.006). Only Aoulad et al. performed this analysis, but found no factor associated with acute esophageal toxicity26. In our study no variable was significantly associated with esophageal grade ≥2 toxicity. Esophageal V30 was at the limit of significance (p = 0.055). In light of these results, we are currently trying to minimize the dose to the esophagus.
Concerning acute skin toxicity, results are heterogeneous among studies. In our study, 2/3 of skin toxicities were of grade 1 and 1/3 of grade 2. Three studies reported slightly lower skin toxicity rates. In Franco et al.’s prospective study, 120 early breast cancer patients underwent whole breast IMRT after conserving surgery delivered with static angle tomotherapy27. Maximum detected acute skin toxicity was grade 0 for 22%, grade 1 for 63%, grade 2 for 12% and grade 3 for 3% of patients. Ha et al. retrospectively analyzed 214 patients with early stage breast cancer who were treated with breast conserving surgery followed by forward IMRT and boost to the surgical bed. Most patients had grade 0 or 1 acute toxicity (82.2%). Two patients reported grade 3 skin desquamation and no grade 4 acute toxicity was observed28. In Wojcieszynski et al.’s evaluation of two simultaneous integrated boost treatment planning techniques using helical tomotherapy for breast conserving therapy, 8/16 patients had grade 2 erythema immediately after irradiation24.
Skin toxicity has been shown to be associated with several patient- and treatment-related variables, such as BMI. In our series, median BMI was high, which could explain the higher incidence of acute toxicity. In this series, BMI (p = 0.003), skin D95% (p = 0.033) and susclavian skin D98% (p = 0.034) were associated with skin grade ≥2 acute toxicity. Despite the correlation with skin toxicity, optimizing the dose to the skin is difficult due to its thickness and the necessity of treating the target volume at the prescribed dose. In order to guarantee dose coverage and robustness of the treatment, dose to the skin should not be optimized18.
De Langhe et al. reported that bra cup size ≥ D, BMI, smoking during RT, and the use of concomitant hormone therapy were associated with acute grade ≥2 dermatitis in multivariate analysis29. Furthermore, patients treated with hypofractionated radiotherapy and those treated in prone position developed less dermatitis. In Franco et al.’s study no categorical variable was found to predict acute toxicity, while several continuous variables (volume of WB-PTV minus TB-PTV receiving 105, 110, 115% of prescription dose, whole breast and boost volume, breast thickness and soft tissue thickness) were associated with grade 2 and grade 3 skin acute events27.
Surprisingly, in univariate analysis, absence of chemotherapy was significantly associated with acute skin toxicity on the partial mastectomy subgroup (63 patients). Subclavian skin volume was associated with medium-term skin grade ≥1 toxicity in multivariate analysis, a variable that did not appear as a prognostic factor in other studies. In Florentino et al.’s study grade 2 acute skin toxicity was significantly associated with late grade 1 toxicity30.
Globally, QoL improved throughout the study. To date, few prospective or retrospective studies have reported QoL data in this context, rendering comparison difficult. In Franco et al.’s study, QoL was generally preserved27. Donovan and Pignol explored QoL outcomes in two randomized trials comparing IMRT and conventional RT for the treatment of breast cancer9,10. There was no difference in QoL between the experimental and the standard treatment arm.
In our series, most patients with positive axillary lymph nodes have been treated with chemotherapy. The results cannot therefore be generalized to all breast cancer patients benefiting from adjuvant RT and should be directed to those receiving IMRT. Additionally, the included population was heterogeneous concerning breast and parietal radiotherapy with or without axillary irradiation. Nevertheless, such heterogeneity brings this study closer to a real-life setting. Finally, sub-group analyses did not have enough power, and certain multivariate analyses were not performed.
Compared to 3D-CRT, IMRT provides excellent coverage of the target volume with lower volumes of OAR receiving high doses. IMRT delivers lower doses to larger volumes of the contralateral lung, contralateral breast, and other normal tissues, which could, in some cases, increased the risk of second cancer. Nevertheless, the risk-benefit ratio could be in favour of IMRT in complex target volumes [14]. This must be confirmed in large prospective series.
In conclusion, there were few statistically significant declines in QoL scores, and aesthetic outcomes were good. Based on these data, tomotherapy may be a favorable alternative to other techniques in patients needing a complex irradiation of the breast and lymph node volumes. Our study is ongoing and further studies will focus on longer follow-up in order to confirm these results.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available due to the clinical and confidential nature of the material but can be made available from the corresponding author on reasonable request.
References
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 378, 1707–1716 (2011).
Hidding, J. T., Beurskens, C. H. G., van der Wees, P. J. & van Laarhoven, H. W. M. & Nijhuis-van der Sanden, M. W. G. Treatment related impairments in arm and shoulder in patients with breast cancer: a systematic review. PLoS ONE 9, e96748 (2014).
Chandra, R. A. et al. Radiation therapy risk factors for development of lymphedema in patients treated with regional lymph node irradiation for breast cancer. Int. J. Radiat. Oncol. Biol. Phys. 91, 760–764 (2015).
Blom Goldman, U., Svane, G., Anderson, M., Wennberg, B. & Lind, P. Long-term functional and radiological pulmonary changes after radiation therapy for breast cancer. Acta Oncol 53, 1373–1379 (2014).
Darby, S. C. et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N. Engl. J. Med. 368, 987–998 (2013).
Grantzau, T. & Overgaard, J. Risk of second non-breast cancer among patients treated with and without postoperative radiotherapy for primary breast cancer: A systematic review and meta-analysis of population-based studies including 522,739 patients. Radiother Oncol 121, 402–413 (2016).
Riou, O., Fenoglietto, P., Lemanski, C. & Azria, D. Intensity modulated radiotherapy for breast cancer. Cancer Radiother 16, 479–484 (2012).
Vicini, F. A. et al. Optimizing breast cancer treatment efficacy with intensity-modulated radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 54, 1336–1344 (2002).
Donovan, E. et al. Randomised trial of standard 2D radiotherapy (RT) versus intensity modulated radiotherapy (IMRT) in patients prescribed breast radiotherapy. Radiother Oncol 82, 254–264 (2007).
Pignol, J.-P. et al. A multicenter randomized trial of breast intensity-modulated radiation therapy to reduce acute radiation dermatitis. J. Clin. Oncol. 26, 2085–2092 (2008).
Barnett, G. C. et al. Randomized controlled trial of forward-planned intensity modulated radiotherapy for early breast cancer: interim results at 2 years. Int. J. Radiat. Oncol. Biol. Phys. 82, 715–723 (2012).
Barnett, G. C. et al. A randomised controlled trial of forward-planned radiotherapy (IMRT) for early breast cancer: baseline characteristics and dosimetry results. Radiother Oncol 92, 34–41 (2009).
Mukesh, M. B. et al. Patient reported outcome measures (PROMs) following forward planned field-in field IMRT: results from the Cambridge Breast IMRT trial. Radiother Oncol 111, 270–275 (2014).
Arsene-Henry, A., Fourquet, A. & Kirova, Y. M. Evolution of radiation techniques in the treatment of breast cancer (BC) patients: From 3D conformal radiotherapy (3D CRT) to intensity-modulated RT (IMRT) using Helical Tomotherapy (HT). Radiother Oncol 124, 333–334 (2017).
Hartford, A. C. et al. American College of Radiology (ACR) and American Society for Radiation Oncology (ASTRO) Practice Guideline for Intensity-modulated Radiation Therapy (IMRT). Am. J. Clin. Oncol. 35, 612–617 (2012).
Offersen, B. V. et al. ESTRO consensus guideline on target volume delineation for elective radiation therapy of early stage breast cancer. Radiother Oncol 114, 3–10 (2015).
Crop, F. et al. Surface imaging, laser positioning or volumetric imaging for breast cancer with nodal involvement treated by helical TomoTherapy. J Appl Clin Med Phys 17, 200–211 (2016).
Crop, F., Heckel, R., Pasquier, D., Lartigau, E. & Reynaert, N. EP-1617: Optimal skin retraction for Helical Tomotherapy breast planning ñ robustness vs skin dose. Radiotherapy and Oncology 111, S211 (2014).
Fayers, P. M. et al. EORTC QLQ-C30 Scoring Manual. (EORTC, 2001).
van der Laan, H. P. et al. Three-dimensional conformal simultaneously integrated boost technique for breast-conserving radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 68, 1018–1023 (2007).
Hurkmans, C. W., Meijer, G. J., van Vliet-Vroegindeweij, C., van der Sangen, M. J. & Cassee, J. High-dose simultaneously integrated breast boost using intensity-modulated radiotherapy and inverse optimization. Int. J. Radiat. Oncol. Biol. Phys. 66, 923–930 (2006).
Smitt, M. C., Li, S. D., Shostak, C. A., Chang, W. & Boyer, A. L. Breast-conserving radiation therapy: potential of inverse planning with intensity modulation. Radiology 203, 871–876 (1997).
Singla, R., King, S., Albuquerque, K., Creech, S. & Dogan, N. Simultaneous-integrated boost intensity-modulated radiation therapy (SIB-IMRT) in the treatment of early-stage left-sided breast carcinoma. Med Dosim 31, 190–196 (2006).
Wojcieszynski, A. P., Olson, A. K., Rong, Y., Kimple, R. J. & Yadav, P. Acute Toxicity From Breast Cancer Radiation Using Helical Tomotherapy With a Simultaneous Integrated Boost. Technol. Cancer Res. Treat. 15, 257–265 (2016).
Caudrelier, J.-M. et al. IMRT sparing of normal tissues in locoregional treatment of breast cancer. Radiat Oncol 9, 161 (2014).
Aoulad, N. et al. Acute toxicity of breast cancer irradiation with modulated intensity by tomotherapy®. Cancer Radiother 21, 180–189 (2017).
Franco, P. et al. Intensity-modulated adjuvant whole breast radiation delivered with static angle tomotherapy (TomoDirect): a prospective case series. J. Cancer Res. Clin. Oncol. 139, 1927–1936 (2013).
Ha, B. et al. Long-term results of forward intensity-modulated radiation therapy for patients with early-stage breast cancer. Radiat Oncol J 31, 191–198 (2013).
De Langhe, S. et al. Factors modifying the risk for developing acute skin toxicity after whole-breast intensity modulated radiotherapy. BMC Cancer 14, 711 (2014).
Fiorentino, A. et al. Intensity modulated radiation therapy with simultaneous integrated boost in early breast cancer irradiation. Report of feasibility and preliminary toxicity. Cancer Radiother 19, 289–294 (2015).
Acknowledgements
We thank Ms J Iriondo for writing assistance.
Author information
Authors and Affiliations
Contributions
Conception and design: D.P., E.L. Data acquisition: D.P., F.T., R.B., A.J., S.H., A.E. Data analysis and interpretation: D.P., R.B., M.C., A.M., F.C., X.M. Statistical analysis: E.T. Manuscript preparation: D.P.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pasquier, D., Le Tinier, F., Bennadji, R. et al. Intensity-modulated radiation therapy with simultaneous integrated boost for locally advanced breast cancer: a prospective study on toxicity and quality of life. Sci Rep 9, 2759 (2019). https://doi.org/10.1038/s41598-019-39469-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-39469-8
This article is cited by
-
Correlation between toxicity and dosimetric parameters for adjuvant intensity modulated radiation therapy of breast cancer: a prospective study
Scientific Reports (2021)
-
Impact of guideline changes on adoption of hypofractionation and breast cancer patient characteristics in the randomized controlled HYPOSIB trial
Strahlentherapie und Onkologie (2021)
-
Acute toxicity of normofractionated intensity modulated radiotherapy with simultaneous integrated boost compared to three-dimensional conformal radiotherapy with sequential boost in the adjuvant treatment of breast cancer
Radiation Oncology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.