Abstract
Patients with kidney disease, especially those with kidney failure, are particularly susceptible to the adverse effects of disasters because their survival depends on functional infrastructure, advanced technology, the availability of specific drugs and well-trained medical personnel. The risk of poor outcomes across the entire spectrum of patients with kidney diseases (acute kidney injury, chronic kidney disease and kidney failure on dialysis or with a functioning transplant) increases as a result of disaster-related logistical challenges. Patients who are displaced face even more complex problems owing to additional threats that arise during travel and after reaching their new location. Overall, risks may be mitigated by pre-disaster preparedness and training. Emergency kidney disaster responses depend on the type and severity of the disaster and include medical and/or surgical treatment of injuries, treatment of mental health conditions, appropriate diet and logistical interventions. After a disaster, patients should be evaluated for problems that were not detected during the event, including those that may have developed as a result of the disaster. A retrospective review of the disaster response is vital to prevent future mistakes. Important ethical concerns include fair distribution of limited resources and limiting harm. Patients with kidney disease, their care-givers, health-care providers and authorities should be trained to respond to the medical and logistical problems that occur during disasters to improve outcomes.
Key points
-
The numbers of man-made and natural disasters are increasing, with the greatest adverse effects in vulnerable populations, including older people, women, children and patients with non-communicable diseases (NCDs).
-
Among patients with NCDs, those with kidney failure require special attention because their survival during disasters depends upon functional infrastructure, advanced technology, the availability of specific drugs and well-trained medical personnel.
-
Although displacement during disasters may be preferred by some patients, additional problems that occur when travelling and/or in the new environment may have a negative impact on their prognosis.
-
Disaster-associated risks for patients with kidney disease may be mitigated by pre-disaster preparedness and training of various stakeholders, including the patients themselves.
-
Patients with acute kidney injury, chronic kidney disease or kidney failure should be evaluated after a disaster to identify any problems that were not detected during the disaster.
-
Retrospective analysis of the disaster response is necessary to identify and learn from mistakes and to avoid these during future events.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
ReliefWeb. Glossary of humanitarian terms. ReliefWeb https://reliefweb.int/sites/reliefweb.int/files/resources/4F99A3C28EC37D0EC12574A4002E89B4-reliefweb_aug2008.pdf (2008).
ReliefWeb. 2021 Disasters in numbers. ReliefWeb https://reliefweb.int/report/world/2021-disasters-numbers (2022).
Our World in Data. State-based conflicts, World, 1946 to 2020, https://ourworldindata.org/grapher/the-number-of-active-state-based-conflicts?country=~OWID_WRL.
World Population Review. Countries currently at war 2022. World Population Review https://worldpopulationreview.com/country-rankings/countries-currently-at-war (2023).
World Health Organization. WHO coronavirus (COVID-19) dashboard. World Health Organization https://covid19.who.int/ (2023).
Collaborators, C.-E. M. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020-21. Lancet 399, 1513–1536 (2022).
Sever, M. S., Remuzzi, G. & Vanholder, R. Disaster medicine and response: optimizing life-saving potential. Am. J. Disaster Med. 13, 253–264 (2018).
Yamanda, S. et al. The impact of the 2011 Great East Japan Earthquake on hospitalisation for respiratory disease in a rapidly aging society: a retrospective descriptive and cross-sectional study at the disaster base hospital in Ishinomaki. BMJ Open https://doi.org/10.1136/bmjopen-2012-000865 (2013).
World Health Organization. COVID-19 significantly impacts health services for noncommunicable diseases. World Health Organization https://www.who.int/news/item/01-06-2020-covid-19-significantly-impacts-health-services-for-noncommunicable-diseases (2020).
Saito, K., Kim, J. I., Maekawa, K., Ikeda, Y. & Yokoyama, M. The great Hanshin-Awaji earthquake aggravates blood pressure control in treated hypertensive patients. Am. J. Hypertens. 10, 217–221 (1997).
Man, R. X., Lack, D. A., Wyatt, C. E. & Murray, V. The effect of natural disasters on cancer care: a systematic review. Lancet Oncol. 19, e482–e499 (2018).
Slama, S. et al. Care of non-communicable diseases in emergencies. Lancet 389, 326–330 (2017).
Murakami, A., Sasaki, H., Pascapurnama, D. N. & Egawa, S. Noncommunicable diseases after the Great East Japan earthquake: systematic review, 2011–2016. Disaster Med. Public Health Prep. 12, 396–407 (2018).
Sever, M. S., Sever, L. & Vanholder, R. Disasters, children and the kidneys. Pediatr. Nephrol. 35, 1381–1393 (2020).
Tanida, N. What happened to elderly people in the great Hanshin earthquake. Br. Med. J. 313, 1133–1135 (1996).
UN Office for Disaster Risk Reduction. Poverty & death: disaster mortality: 1996–2015. UNISDR https://www.preventionweb.net/files/50589_creddisastermortalityallfinalpdf.pdf (2016).
Khanijahani, A., Iezadi, S., Gholipour, K., Azami-Aghdash, S. & Naghibi, D. A systematic review of racial/ethnic and socioeconomic disparities in COVID-19. Int. J. Equity Health 20, 248 (2021).
Prendki, V., Tiseo, G. & Falcone, M., ESCMID Study Group for Infections in the Elderly (ESGIE). Caring for older adults during the COVID-19 pandemic. Clin. Microbiol. Infect. 28, 785–791 (2022).
Knighton, A. J., Brunisholz, K. D. & Savitz, S. T. Detecting risk of low health literacy in disadvantaged populations using area-based measures. EGEMS 5, 7 (2017).
International Union for Conservation of Nature. Disaster and gender statistics. IUCN https://www.unisdr.org/files/48152_disasterandgenderstatistics.pdf.
Baba, S. et al. The Great Hanshin earthquake. Lancet 347, 307–309 (1996).
Kario, K. Measuring the effects of stress on the cardiovascular system during a disaster: the effective use of self-measured blood pressure monitoring. J. Hypertens. 28, 657–659 (2010).
Hassan, S. et al. Management of chronic noncommunicable diseases after natural disasters in The Caribbean: a scoping review. Health Aff. 39, 2136–2143 (2020).
Wakui, T., Agree, E. M., Saito, T. & Kai, I. Disaster preparedness among older Japanese adults with long-term care needs and their family caregivers. Disaster Med. Public Health Prep. 11, 31–38 (2017).
Issa, A. et al. Deaths related to hurricane Irma – Florida, Georgia, and North Carolina, September 4–October 10, 2017. Morb. Mortal. Wkly. Rep. 67, 829–832 (2018).
Sever, M. S. et al. Armed conflicts and kidney patients: a consensus statement from the Renal Disaster Relief Task Force of the ERA. Nephrol. Dial. Transpl. https://doi.org/10.1093/ndt/gfac247 (2022).
Luyckx, V. A., Tonelli, M. & Stanifer, J. W. The global burden of kidney disease and the sustainable development goals. Bull. World Health Organ. 96, 414–422C (2018).
World Health Organization. World health statistics 2022: monitoring health for the SDGs, sustainable development goals. World Health Organization https://www.who.int/publications/i/item/9789240051157 (2022).
Albittar M. The effects of COVID-19 on non-communicable diseases: a case study of six countries. reliefweb https://reliefweb.int/report/bangladesh/effects-covid-19-non-communicable-diseases-case-study-six-countries (2021).
World Kidney Day. 2023 WKD theme. Kidney health for al: preparing for the unexpected, supporting the vulnerable! World Kidney Day https://www.worldkidneyday.org/2023-campaign/2023-wkd-theme/ (2023).
Bywaters, E. G. & Beall, D. Crush injuries with impairment of renal function. Br. Med. J. 1, 427–432 (1941).
Collins, A. J. Kidney dialysis treatment for victims of the Armenian earthquake. N. Engl. J. Med. 320, 1291–1292 (1989).
Solez, K. et al. International dialysis aid in earthquakes and other disasters. Kidney Int. 44, 479–483 (1993).
Vanholder, R., Sever, M. S., Erek, E. & Lameire, N. Acute renal failure related to the crush syndrome: towards an era of seismo-nephrology? Nephrol. Dial. Transpl. 15, 1517–1521 (2000).
Sever, M. S. et al. The Marmara earthquake: epidemiological analysis of the victims with nephrological problems. Kidney Int. 60, 1114–1123 (2001).
Sever, M. S., Lameire, N., Van Biesen, W. & Vanholder, R. Disaster nephrology: a new concept for an old problem. Clin. Kidney J. 8, 300–309 (2015).
Mogul F. The coronavirus crisis: shortage of dialysis equipment leads to difficult decisions in New York ICUs. NPR https://www.npr.org/sections/health-shots/2020/04/19/838103327/shortage-of-dialysis-equipment-leads-to-difficult-decisions-in-new-york-icus (2020).
Jdiaa, S. S. et al. COVID-19 and chronic kidney disease: an updated overview of reviews. J. Nephrol. 35, 69–85 (2022).
Karadag, S. et al. Post-COVID-19 outcomes of non-dialysis dependent chronic kidney disease patients: a national, multicenter, controlled study. Int. Urol. Nephrol. 55, 399–408 (2022).
Goffin, E. et al. COVID-19-related mortality in kidney transplant and haemodialysis patients: a comparative, prospective registry-based study. Nephrol. Dial. Transpl. 36, 2094–2105 (2021).
Sever, M. S., Vanholder, R. & Lameire, N. Acute kidney injury in active wars and other man-made disasters. Semin. Nephrol. 40, 341–353 (2020).
Oda, J. et al. Analysis of 372 patients with crush syndrome caused by the Hanshin-Awaji earthquake. J. Trauma 42, 470–475 (1997).
Gupta, S. et al. AKI treated with renal replacement therapy in critically ill patients with COVID-19. J. Am. Soc. Nephrol. 32, 161–176 (2021).
Sever, M. S. & Vanholder, R., RDRTF of the ISN Work Group on Recommendations for the Management of Crush Victims in Mass Disasters. Recommendation for the management of crush victims in mass disasters. Nephrol. Dial. Transpl. 27, i1–i67 (2012).
Vanholder, R., Sever, M. S., Erek, E. & Lameire, N. Rhabdomyolysis. J. Am. Soc. Nephrol. 11, 1553–1561 (2000).
Sever, M. S., Vanholder, R. & Lameire, N. Management of crush-related injuries after disasters. N. Engl. J. Med. 354, 1052–1063 (2006).
Richards, N. T. et al. Dialysis for acute renal failure due to crush injuries after the Armenian earthquake. Br. Med. J. 298, 443–445 (1989).
Prakash, J. et al. Acute renal failure in Falciparum malaria – increasing prevalence in some areas of India – a need for awareness. Nephrol. Dial. Transpl. 11, 2414–2416 (1996).
Yang, C. W. Leptospirosis renal disease: emerging culprit of chronic kidney disease unknown etiology. Nephron 138, 129–136 (2018).
Hatamizadeh, P. et al. Epidemiologic aspects of the Bam earthquake in Iran: the nephrologic perspective. Am. J. Kidney Dis. 47, 428–438 (2006).
Sever, M. S. et al. Clinical findings in the renal victims of a catastrophic disaster: the Marmara earthquake. Nephrol. Dial. Transpl. 17, 1942–1949 (2002).
Smith, L. H. Jr. et al. Post-traumatic renal insufficiency in military casualties. II. Management, use of an artificial kidney, prognosis. Am. J. Med. 18, 187–198 (1955).
Atef, M. R., Nadjatfi, I., Boroumand, B. & Rastegar, A. Acute renal failure in earthquake victims in Iran: epidemiology and management. Q. J. Med. 87, 35–40 (1994).
Heegard, K. D. et al. Early acute kidney injury in military casualties. J. Trauma Acute Care Surg. 78, 988–993 (2015).
Hwang, S. J., Shu, K. H., Lain, J. D. & Yang, W. C. Renal replacement therapy at the time of the Taiwan Chi-Chi earthquake. Nephrol. Dial. Transpl. 16, 78–82 (2001).
Sever, M. S. et al. Treatment modalities and outcome of the renal victims of the Marmara earthquake. Nephron 92, 64–71 (2002).
van der Tol, A. et al. Impact of local circumstances on outcome of renal casualties in major disasters. Nephrol. Dial. Transpl. 24, 907–912 (2009).
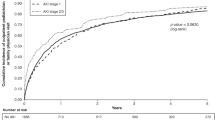
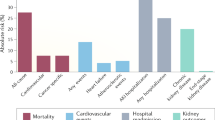
Stewart, I. J. et al. Retrospective analysis of long-term outcomes after combat injury: a hidden cost of war. Circulation 132, 2126–2133 (2015).
Lumlertgul, N. et al. Acute kidney injury prevalence, progression and long-term outcomes in critically ill patients with COVID-19: a cohort study. Ann. Intensive Care 11, 123 (2021).
Geetha, D. et al. Impact of the COVID-19 pandemic on the kidney community: lessons learned and future directions. Nat. Rev. Nephrol. 18, 724–737 (2022).
Vanholder, R. et al. Continuing kidney care in conflicts. Nat. Rev. Nephrol. 18, 479–480 (2022).
Sekkarie, M. et al. End-stage kidney disease in areas of armed conflicts: challenges and solutions. Semin. Nephrol. 40, 354–362 (2020).
Chen, G. et al. When the COVID-19 pandemic changed the follow-up landscape of chronic kidney disease: a survey of real-world nephrology practice. Ren. Fail. 42, 733–739 (2020).
Alasfar S & Trollinger B. Immunosuppression management in conflict zones. NephroWorldCup https://sites.google.com/view/nephroworldcup/extras/westandwithukraine (2022).
Levin, A. & Stevens, P. E. Summary of KDIGO 2012 CKD Guideline: behind the scenes, need for guidance, and a framework for moving forward. Kidney Int. 85, 49–61 (2014).
Zemp, D. D. et al. Gait disorders in CKD patients: muscle wasting or cognitive impairment? A cross-sectional pilot study to investigate gait signatures in stage 1–5 CKD patients. BMC Nephrol. 23, 72 (2022).
Armenian, H. K., Melkonian, A., Noji, E. K. & Hovanesian, A. P. Deaths and injuries due to the earthquake in Armenia: a cohort approach. Int. J. Epidemiol. 26, 806–813 (1997).
American Society of Nephrology, European Renal Association & International Society of Nephrology. More than 850 million worldwide have some form of kidney disease: help raise awareness. International Society of Nephrology https://www.theisn.org/more-than-850-million-worldwide-have-some-form-of-kidney-disease-help-raise-awareness/ (2022).
Abe, M. et al. A massive natural disaster, the Great East Japan Earthquake, and the incidence of dialysis due to end-stage kidney disease. J. Nephrol. 35, 719–724 (2022).
Sever, M. S. et al. Features of chronic hemodialysis practice after the Marmara earthquake. J. Am. Soc. Nephrol. 15, 1071–1076 (2004).
Anderson, A. H. et al. Missed dialysis sessions and hospitalization in hemodialysis patients after Hurricane Katrina. Kidney Int. 75, 1202–1208 (2009).
Kelman, J. et al. Dialysis care and death following Hurricane Sandy. Am. J. Kidney Dis. 65, 109–115 (2015).
Phend C. Dialysis crisis in Texas: ‘catastrophic’. Medpage Today https://www.medpagetoday.com/nephrology/esrd/91258 (2021).
Tannor, E. K. et al. The COVID-19 pandemic identifies significant global inequities in hemodialysis care in low and lower-middle income countries – an ISN/DOPPS survey. Kidney Int. Rep. 7, 971–982 (2022).
Aylward, R. et al. The global impact of the COVID-19 pandemic on in-center hemodialysis services: an ISN-Dialysis Outcomes Practice Patterns Study survey. Kidney Int. Rep. 7, 397–409 (2022).
Council, E.-E. & Group, E. W. Chronic kidney disease is a key risk factor for severe COVID-19: a call to action by the ERA-EDTA. Nephrol. Dial. Transpl. 36, 87–94 (2021).
el-Reshaid, K., Johny, K. V., Georgous, M., Nampoory, M. R. & al-Hilal, N. The impact of Iraqi occupation on end-stage renal disease patients in Kuwait, 1990–1991. Nephrol. Dial. Transpl. 8, 7–10 (1993).
Smith, R. S., Zucker, R. J. & Frasso, R. Natural disasters in the Americas, dialysis patients, and implications for emergency planning: a systematic review. Prev. Chronic Dis. 17, E42 (2020).
Stepanova, N. et al. Lifesaving care for patients with kidney failure during the war in Ukraine 2022. Clin. J. Am. Soc. Nephrol. 17, 1079–1081 (2022).
Krespi, M. R. Psychosocial interventions to improve outcomes among dialysis patients. Semin. Dial. 31, 65–71 (2018).
Kopp, J. B. et al. Kidney patient care in disasters: lessons from the hurricanes and earthquake of 2005. Clin. J. Am. Soc. Nephrol. 2, 814–824 (2007).
Sever, M. S., Ortiz, A., Maggiore, U., Bac-Garcia, E. & Vanholder, R. Mass disasters and burnout in nephrology personnel: from earthquakes and hurricanes to COVID-19 pandemic. Clin. J. Am. Soc. Nephrol. 16, 829–837 (2021).
Mesic, E., Aleckovic-Halilovic, M., Tulumovic, D. & Trnacevic, S. Nephrology in Bosnia and Herzegovina: impact of the 1992–95 war. Clin. Kidney J. 11, 803–809 (2018).
Vanholder, R., Gallego, D. & Sever, M. S. Wars and kidney patients: a statement by the European Kidney Health Alliance related to the Russian–Ukrainian conflict. J. Nephrol. 35, 377–380 (2022).
Sourial, M. Y. et al. Urgent peritoneal dialysis in patients with COVID-19 and acute kidney injury: a single-center experience in a time of crisis in the United States. Am. J. Kidney Dis. 76, 401–406 (2020).
Gorbatkin, C., Finkelstein, F. O. & Kazancioglu, R. T. Peritoneal dialysis during active war. Semin. Nephrol. 40, 375–385 (2020).
Sakai, R. The Japanese experience during the Kobe Earthquake: management of continuous ambulatory peritoneal dialysis patients in a disaster. Ren. Fail. 19, 693–699 (1997).
Ozener, C., Ozdemir, D. & Bihorac, A. The impact of the earthquake in northwestern Turkey on the continuous ambulatory peritoneal dialysis patients who were living in the earthquake zone. Adv. Perit. Dial. 16, 182–185 (2000).
Tzamaloukas, A. H. Risk of extracellular volume expansion in long-term peritoneal dialysis. Adv. Perit. Dial. 21, 106–111 (2005).
Bonilla-Felix, M. & Suarez-Rivera, M. Disaster management in a nephrology service: lessons learned from Hurricane Maria. Blood Purif. 47, 199–204 (2019).
Gray, N. A., Wolley, M., Liew, A. & Nakayama, M. Natural disasters and dialysis care in the Asia-Pacific. Nephrology 20, 873–880 (2015).
Kleinpeter, M. A. End-stage renal disease use in hurricane-prone areas: should nephrologists increase the utilization of peritoneal dialysis? Adv. Chronic Kidney Dis. 14, 100–104 (2007).
Albakr, R. et al. An ISN-DOPPS survey of the global impact of the COVID-19 pandemic on peritoneal dialysis services. Kidney Int. Rep. 7, 2196–2206 (2022).
Alasfar, S., Isreb, M., Kaysi, S. & Hatahet, K. Renal transplantation in areas of armed conflict. Semin. Nephrol. 40, 386–392 (2020).
Salvalaggio, P. R. et al. An international survey on living kidney donation and transplant practices during the COVID-19 pandemic. Transpl. Infect. Dis. 23, e13526 (2021).
Loupy, A. et al. Organ procurement and transplantation during the COVID-19 pandemic. Lancet 395, e95–e96 (2020).
Shimmura, H., Kawaguchi, H., Tokiwa, M. & Tanabe, K. Impact of the Great Eastern Japan Earthquake on transplant renal function in Iwaki city, Fukushima. Transpl. Proc. 46, 613–615 (2014).
Ao, G. et al. The association between severe or death COVID-19 and solid organ transplantation: a systematic review and meta-analysis. Transpl. Rev. 35, 100628 (2021).
Hilbrands, L. B. et al. COVID-19-related mortality in kidney transplant and dialysis patients: results of the ERACODA collaboration. Nephrol. Dial. Transpl. 35, 1973–1983 (2020).
Fishman, J. A. The immunocompromised transplant recipient and SARS-CoV-2 infection. J. Am. Soc. Nephrol. 31, 1147–1149 (2020).
Maggiore, U. et al. How should I manage immunosuppression in a kidney transplant patient with COVID-19? An ERA-EDTA DESCARTES expert opinion. Nephrol. Dial. Transpl. 35, 899–904 (2020).
Lentine, K. L., Mannon, R. B. & Josephson, M. A. Practicing with uncertainty: kidney transplantation during the COVID-19 pandemic. Am. J. Kidney Dis. 77, 777–785 (2021).
Schmidt-Lauber, C., Spoden, M., Huber, T. B., Gunster, C. & Grahammer, F. Increased rejection rates in kidney transplantations during the COVID-19 pandemic. Transpl. Int. 34, 2899–2902 (2021).
World Health Organization. Public health risk assessment and interventions: earthquake: Haiti. World Health Organization https://apps.who.int/iris/bitstream/handle/10665/70221/WHO_HSE_GAR_DCE_2010.1_eng.pdf (2010).
Azzouzi, S. et al. The impact of the COVID-19 pandemic on healthy lifestyle behaviors and perceived mental and physical health of people living with non-communicable diseases: an international cross-sectional survey. Int J. Environ. Res Public Health https://doi.org/10.3390/ijerph19138023 (2022).
Cogley, C., Carswell, C., Bramham, K. & Chilcot, J. Chronic kidney disease and severe mental illness: addressing disparities in access to health care and health outcomes. Clin. J. Am. Soc. Nephrol. 17, 1413–1417 (2022).
Edmondson, D. et al. Association of posttraumatic stress disorder and depression with all-cause and cardiovascular disease mortality and hospitalization among Hurricane Katrina survivors with end-stage renal disease. Am. J. Public Health 103, e130–e137 (2013).
Uemoto, M., Inui, A., Kasuga, M., Shindo, S. & Taniguchi, H. Medical staff suffered severe stress after earthquake in Kobe, Japan. Br. Med. J. 313, 1144 (1996).
Ghahramani, S., Kasraei, H., Hayati, R., Tabrizi, R. & Marzaleh, M. A. Health care workers’ mental health in the face of COVID-19: a systematic review and meta-analysis. Int. J. Psychiatry Clin. Pract. 27, 208–217 (2022).
Agrawal, V. et al. Burnout and emotional well-being among nephrology fellows: a National Online Survey. J. Am. Soc. Nephrol. 31, 675–685 (2020).
Center for Clinical Standards and Quality/Quality, Safety & Oversight Group. State Operations Manual. Appendix Z – Emergency preparedness for all provider and certified supplier types interpretive guidance. Centers for Medicare & Medicaid Services https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/QSO19-06-ALL.pdf (2019).
Adini, B., Goldberg, A., Cohen, R., Laor, D. & Bar-Dayan, Y. Evidence-based support for the all-hazards approach to emergency preparedness. Isr. J. Health Policy Res. 1, 40 (2012).
World Health Organization. Regional Office for Europe. Hospital emergency response checklist: an all-hazards tool for hospital administrators and emergency managers. World Health Organization https://apps.who.int/iris/handle/10665/349374 (2011).
Lameire, N., Sever, M. S., Van Biesen, W. & Vanholder, R. Role of the international and national renal organizations in natural disasters: strategies for renal rescue. Semin. Nephrol. 40, 393–407 (2020).
Sever, M. S., Lameire, N. & Vanholder, R. Renal disaster relief: from theory to practice. Nephrol. Dial. Transpl. 24, 1730–1735 (2009).
Vanholder, R. et al. When the earth trembles in the Americas: the experience of Haiti and Chile 2010. Nephron Clin. Pract. 117, c184–c197 (2011).
Vanholder, R. et al. Earthquakes and crush syndrome casualties: lessons learned from the Kashmir disaster. Kidney Int. 71, 17–23 (2007).
Vanholder, R., Sever, M. S., De Smet, M., Erek, E. & Lameire, N. Intervention of the Renal Disaster Relief Task Force in the 1999 Marmara, Turkey earthquake. Kidney Int. 59, 783–791 (2001).
Neuman, ME. Dialysis providers assess damage from Hurricane Ian. Healio https://www.healio.com/news/nephrology/20221003/dialysis-providers-assess-damage-from-hurricane-ian (2022).
Kadowaki, M. et al. Medication compliance in renal transplant patients during the Great East Japan Earthquake. Transpl. Proc. 46, 610–612 (2014).
Sharief, S., Freitas, D., Adey, D. & Wiley, J. Disaster preparation in kidney transplant recipients: a questionnaire-based cohort study from a large United States transplant center. Clin. Nephrol. 89, 241–248 (2018).
Murakami, N., Siktel, H. B., Lucido, D., Winchester, J. F. & Harbord, N. B. Disaster preparedness and awareness of patients on hemodialysis after Hurricane Sandy. Clin. J. Am. Soc. Nephrol. 10, 1389–1396 (2015).
Foster, M. et al. Personal disaster preparedness of dialysis patients in North Carolina. Clin. J. Am. Soc. Nephrol. 6, 2478–2484 (2011).
Liossatou, A & Golland, E. Disaster preparedness and evacuation plan (DPEP) in haemodialysis units: patients’ emergency self-disconnection through “Clamp and cut” procedure. EDTNA/ERCA https://www.edtnaerca.org/resource/edtna/files/ElectronicLibrary_Managing_5-21%20(2).pdf (2021).
Boyte, E. (National Kidney Foundation). Be prepared: planning for emergencies. Kidney Living https://www.kidney.org/sites/default/files/01-65-7279_EBG_KidneyLiving15.pdf (2016).
Schultz, C. H. & Annas, G. J. Altering the standard of care in disasters – unnecessary and dangerous. Ann. Emerg. Med. 59, 191–195 (2012).
Better, O. S. & Stein, J. H. Early management of shock and prophylaxis of acute renal failure in traumatic rhabdomyolysis. N. Engl. J. Med. 322, 825–829 (1990).
Brown, C. V. et al. Preventing renal failure in patients with rhabdomyolysis: do bicarbonate and mannitol make a difference? J. Trauma 56, 1191–1196 (2004).
Sever, M. S. & Vanholder, R. Management of crush victims in mass disasters: highlights from recently published recommendations. Clin. J. Am. Soc. Nephrol. 8, 328–335 (2013).
Nourse, P. et al. ISPD guidelines for peritoneal dialysis in acute kidney injury: 2020 update (paediatrics). Perit. Dial. Int. 41, 139–157 (2021).
Cullis, B. et al. ISPD guidelines for peritoneal dialysis in acute kidney injury: 2020 update (adults). Perit. Dial. Int. 41, 15–31 (2021).
Lodge, M. D. S. et al. Safely reducing haemodialysis frequency during the COVID-19 pandemic. BMC Nephrol. 21, 532 (2020).
Meyer, T. W., Hostetter, T. H. & Watnick, S. Twice-weekly hemodialysis is an option for many patients in times of dialysis unit stress. J. Am. Soc. Nephrol. 31, 1141–1142 (2020).
Burgner, A., Ikizler, T. A. & Dwyer, J. P. COVID-19 and the inpatient dialysis unit: managing resources during contingency planning pre-crisis. Clin. J. Am. Soc. Nephrol. 15, 720–722 (2020).
Aviles Mendoza, G. J. et al. Observations from the emergency management of dialysis patients evacuated from the US Virgin Islands to Puerto Rico following hurricane Irma. BMC Health Serv. Res. 21, 1239 (2021).
Weinhandl, E. D., Liu, J., Gilbertson, D. T., Wetmore, J. B. & Johansen, K. L. Associations of COVID-19 outcomes with dialysis modalities and settings. Clin. J. Am. Soc. Nephrol. 17, 1526–1534 (2022).
Sever, L. & Balat, A. Renal crisis in children during armed conflict. Semin. Nephrol. 40, 408–420 (2020).
Kleinpeter, M. A., Norman, L. D. & Krane, N. K. Disaster planning for peritoneal dialysis programs. Adv. Perit. Dial. 22, 124–129 (2006).
Sever, M. S. et al. Kidney transplantation during mass disasters – from COVID-19 to other catastrophes: a Consensus Statement by the DESCARTES Working Group and Ethics Committee of the ERA. Nephrol. Dial. Transpl. https://doi.org/10.1093/ndt/gfac251 (2022).
Teoh, C. W. et al. Management of pediatric kidney transplant patients during the COVID-19 pandemic: guidance from the Canadian Society of Transplantation Pediatric Group. Can. J. Kidney Health Dis. 7, 2054358120967845 (2020).
Al Ammary, F., Sidoti, C., Segev, D. L. & Henderson, M. L. Health care policy and regulatory challenges for adoption of telemedicine in kidney transplantation. Am. J. Kidney Dis. 77, 773–776 (2021).
Chan, A. S. W., Ho, J. M. C., Li, J. S. F., Tam, H. L. & Tang, P. M. K. Impacts of COVID-19 pandemic on psychological well-being of older chronic kidney disease patients. Front. Med. 8, 666973 (2021).
Saeed, S. A. & Gargano, S. P. Natural disasters and mental health. Int. Rev. Psychiatry 34, 16–25 (2022).
Momoi, M., Murakami, M., Horikoshi, N. & Maeda, M. Dealing with community mental health post the Fukushima disaster: lessons learnt for the COVID-19 pandemic. QJM 113, 787–788 (2020).
World Health Organization. Mental health in emergencies. World Health Organization https://www.who.int/news-room/fact-sheets/detail/mental-health-in-emergencies (2022).
Gnanapragasam, S., Aitsi-Selmi, A., Rashbrook, E. & Murray, V. Addressing non-communicable diseases in disaster risk reduction – an issue of equity. J. Epidemiol. Glob. Health 6, 119–121 (2016).
US Fire Administration. Operational lessons learned in disaster response. FEMA https://www.usfa.fema.gov/downloads/pdf/publications/operational_lessons_learned_in_disaster_response.pdf (2015).
UN Refugee Agency. Refugee data finder. UNHCR https://www.unhcr.org/refugee-statistics/ (2023).
Barbullushi, M., Koroshi, A. & Tase, M. Albanian contribution to the treatment of refugee renal patients from Kosovo. Nephrol. Dial. Transpl. 15, 1261 (2000).
Balat, A. et al. Kidney disease profile and encountered problems during follow-up in Syrian refugee children: a multicenter retrospective study. Pediatr. Nephrol. 37, 393–402 (2022).
Aoun, M. & Koubar, S. H. Impact of forced human migration on management of end-stage kidney disease in host countries. Semin. Nephrol. 40, 363–374 (2020).
World Health Organization. Guidelines for medicine donations. World Health Organization https://apps.who.int/iris/bitstream/handle/10665/44647/9789241501989_eng.pdf (2010).
McDonald, S., Fabbri, A., Parker, L., Williams, J. & Bero, L. Medical donations are not always free: an assessment of compliance of medicine and medical device donations with World Health Organization guidelines (2009-2017). Int. Health 11, 379–402 (2019).
Slama, S., Lee, J., Aragno, M., Laroche, S. & Hogerzeil, H. The development of the noncommunicable diseases emergency health kit. East. Mediterr. Health J. 24, 92–98 (2018).
Larkin G. L. in Koenig and Schultz’s Disaster Medicine (eds Koenig, K. L. & Schultz, C. H.) 62–74 (Cambridge Univ. Press, 2010).
Lateef, F. Ethical issues in disasters. Prehosp. Disaster Med. 26, 289–292 (2011).
Emanuel, E. J. et al. Fair allocation of scarce medical resources in the time of Covid-19. N. Engl. J. Med. 382, 2049–2055 (2020).
Jobges, S., Vinay, R., Luyckx, V. A. & Biller-Andorno, N. Recommendations on COVID-19 triage: international comparison and ethical analysis. Bioethics 34, 948–959 (2020).
Archard, D. & Caplan, A. Is it wrong to prioritise younger patients with covid-19. Br. Med. J. 369, m1509 (2020).
Martin, D. E., Parsons, J. A., Caskey, F. J., Harris, D. C. H. & Jha, V. Ethics of kidney care in the era of COVID-19. Kidney Int. 98, 1424–1433 (2020).
Antommaria, A. H., Powell, T., Miller, J. E. & Christian, M. D., Task Force for Pediatric Emergency Mass Critical Care. Ethical issues in pediatric emergency mass critical care. Pediatr. Crit. Care Med. 12, S163–S168 (2011).
Barnett, D. J., Taylor, H. A., Hodge, J. G. Jr. & Links, J. M. Resource allocation on the frontlines of public health preparedness and response: report of a summit on legal and ethical issues. Public Health Rep. 124, 295–303 (2009).
Acknowledgements
R.V. is President of the European Kidney Health Alliance (EKHA), which is a not-for-profit organization defending the case of patients with kidney disease and the nephrology community at the level of the European Commission. The EKHA network has five full members (the European Renal Association, the International Society of Nephrology, the European Kidney Patients Federation, the European Dialysis and Transplant Nurses Association/European Renal Care Association and the Dutch Kidney Foundation) as well as 30 national or regional societies that are affiliated members. The EKHA is the recipient of support from the European Union in the context of the Annual Work Programme 2022 on prevention of non-communicable diseases of EU4Health, topic ID EU4H-2022-PJ02, project no. 101101220 PREVENTCKD.
Author information
Authors and Affiliations
Contributions
M.S.S., V.L., M.T., D.R. and R.V. researched data for the article. M.S.S., V.L., M.T., R.K., D.G., S.T. and R.V. contributed substantially to discussion of the content. M.S.S., D.R. and R.V. wrote the article. M.S.S., V.L., M.T., R.K., D.R., S.T. and R.V. reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Nephrology thanks Michiaki Abe, Kent Doi and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Glossary
- Chronic kidney disease
-
Abnormalities of kidney structure or function that are present for longer than 3 months, with implications for health.
- Crush syndrome
-
Crush injury and muscle damage-induced systemic manifestations, which may include, but are not limited to, hypovolaemic shock, acute kidney injury, electrolyte disturbances, sepsis, acute respiratory distress syndrome and disseminated intravascular coagulation.
- Destructive disasters
-
Sudden calamitous events that result in huge amounts of damage, loss or destruction.
- Kidney failure
-
Glomerular filtration rate <15 ml/min/1.73 m2. Kidney failure is characterized by signs and symptoms of uraemia or a requirement to initiate kidney replacement therapy (dialysis or transplantation).
- Primary survey
-
A basic survey to identify and simultaneously treat life-threatening conditions. For pragmatic reasons, the injuries are surveyed in an orderly fashion based on the simple mnemonic, ABCDE (airway, breathing, circulation, disability, exposure).
- Somatic symptoms
-
Subjective distress related to physical symptoms, which may include pain, gastroenterological, cardiovascular, genitourinary, neurological and other symptoms.
- Third spacing
-
Fluid shifts into the interstitial spaces or into a body cavity that normally contain little fluid, such as the muscle compartments.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sever, M.S., Luyckx, V., Tonelli, M. et al. Disasters and kidney care: pitfalls and solutions. Nat Rev Nephrol 19, 672–686 (2023). https://doi.org/10.1038/s41581-023-00743-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41581-023-00743-8
This article is cited by
-
Earthquake victims in focus: a cross-sectional examination of trauma and management in intensive care unit
BMC Emergency Medicine (2024)