Abstract
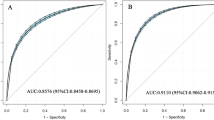
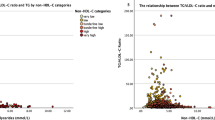
Remnant cholesterol (RC) has been associated with atherosclerotic cardiovascular disease, but its relationship with hypertension remains unclear. This prospective cohort study aimed to investigate the association between RC and subsequent hypertension risk. Data from the UK Biobank, comprising 295,062 participants initially free of hypertension, were analyzed. Cox proportional hazards regression assessed the association between RC quartiles and hypertension risk. Discordance analysis evaluated the risk of hypertension in discordant/concordant groups of RC and low-density lipoprotein cholesterol (LDL-C) using the difference in percentile units (>10 units). Restricted cubic spline curves were used to model the relationship between RC and hypertension risk. The mean ± SD age of participants was 55.1 ± 8.1 years, with 40.6% being men and 94.7% White. During a median follow-up of 12.8 years, 39,038 participants developed hypertension. Comparing extreme quartiles of RC, the hazard ratio (HR) for incident hypertension was 1.20 (95% CI: 1.17–1.24). After adjusting for traditional risk factors, each 1 mmol/L increase in RC levels was associated with a 27% higher risk of incident hypertension (HR: 1.27; 95% CI: 1.23–1.31). The discordant group with high RC/low LDL-C exhibited a higher risk of incident hypertension compared to the concordant group (HR: 1.06; 95% CI: 1.03–1.09). Spline curves further demonstrated a positive association between RC and the risk of incident hypertension. We concluded that elevated RC emerged as an independent risk factor of incident hypertension, extending beyond traditional risk factors. Monitoring RC levels and implementing interventions to lower RC may have potential benefits in preventing hypertension.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16:223–37.
Brouwers S, Sudano I, Kokubo Y, Sulaica EM. Arterial hypertension. Lancet. 2021;398:249–61.
Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–8.
Danaei G, Finucane MM, Lin JK, Singh GM, Paciorek CJ, Cowan MJ, et al. National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5·4 million participants. Lancet. 2011;377:568–77.
Wang TJ, Gona P, Larson MG, Levy D, Benjamin EJ, Tofler GH, et al. Multiple biomarkers and the risk of incident hypertension. Hypertension. 2007;49:432–8.
Halperin RO, Sesso HD, Ma J, Buring JE, Stampfer MJ, Gaziano JM. Dyslipidemia and the risk of incident hypertension in men. Hypertension. 2006;47:45–50.
Otsuka T, Takada H, Nishiyama Y, Kodani E, Saiki Y, Kato K, et al. Dyslipidemia and the risk of developing hypertension in a working-age male population. J Am Heart Assoc. 2016;5:e003053.
Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: A meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–81.
Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017;38:2459–72.
Quispe R, Martin SS, Michos ED, Lamba I, Blumenthal RS, Saeed A, et al. Remnant cholesterol predicts cardiovascular disease beyond LDL and ApoB: A primary prevention study. Eur Heart J. 2021;42:4324–32.
Langsted A, Madsen CM, Nordestgaard BG. Contribution of remnant cholesterol to cardiovascular risk. J Intern Med. 2020;288:116–27.
Varbo A, Nordestgaard BG. Remnant cholesterol and triglyceride-rich lipoproteins in atherosclerosis progression and cardiovascular disease. Arterioscler Thromb Vasc Biol. 2016;36:2133–5.
Hao QY, Gao JW, Yuan ZM, Gao M, Wang JF, Schiele F, et al. Remnant cholesterol and the risk of coronary artery calcium progression: Insights from the CARDIA and MESA study. Circ Cardiovasc Imaging. 2022;15:e014116.
Castañer O, Pintó X, Subirana I, Amor AJ, Ros E, Hernáez Á, et al. Remnant cholesterol, not LDL cholesterol, is associated with incident cardiovascular disease. J Am Coll Cardiol. 2020;76:2712–24.
Wang J, Sun Q, An Y, Liu J, Leng S, Wang G. The association of remnant cholesterol (RC) and interaction between RC and diabetes on the subsequent risk of hypertension. Front Endocrinol. 2022;13:951635.
Li K, Fan F, Zheng B, Jia J, Liu B, Liu J, et al. Associations between remnant lipoprotein cholesterol and central systolic blood pressure in a Chinese community-based population: A cross-sectional study. Lipids Health Dis. 2021;20:60.
Kasahara A, Adachi H, Hirai Y, Enomoto M, Fukami A, Yoshikawa K, et al. High level of plasma remnant-like particle cholesterol may predispose to development of hypertension in normotensive subjects. Am J Hypertens. 2013;26:793–8.
Chen MM, Huang X, Xu C, Song XH, Liu YM, Yao D, et al. High remnant cholesterol level potentiates the development of hypertension. Front Endocrinol (Lausanne). 2022;13:830347.
Bernelot Moens SJ, Verweij SL, Schnitzler JG, Stiekema LCA, Bos M, Langsted A, et al. Remnant cholesterol elicits arterial wall inflammation and a multilevel cellular immune response in humans. Arterioscler Thromb Vasc Biol. 2017;37:969–75.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779.
Elliott P, Peakman TC. The UK Biobank sample handling and storage protocol for the collection, processing and archiving of human blood and urine. Int J Epidemiol. 2008;37:234–44.
Varbo A, Benn M, Tybjærg-Hansen A, Jørgensen AB, Frikke-Schmidt R, Nordestgaard BG. Remnant cholesterol as a causal risk factor for ischemic heart disease. J Am Coll Cardiol. 2013;61:427–36.
Varbo A, Benn M, Smith GD, Timpson NJ, Tybjaerg-Hansen A, Nordestgaard BG. Remnant cholesterol, low-density lipoprotein cholesterol, and blood pressure as mediators from obesity to ischemic heart disease. Circ Res. 2015;116:665–73.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Elliott P, Stamler J, Nichols R, Dyer AR, Stamler R, Kesteloot H, et al. Intersalt revisited: further analyses of 24 h sodium excretion and blood pressure within and across populations. Intersalt Cooperative Research Group. BMJ. 1996;312:1249–53.
Thadhani R, Camargo CA Jr., Stampfer MJ, Curhan GC, Willett WC, Rimm EB. Prospective study of moderate alcohol consumption and risk of hypertension in young women. Arch Intern Med. 2002;162:569–74.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr., et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52.
Wang NY, Young JH, Meoni LA, Ford DE, Erlinger TP, Klag MJ. Blood pressure change and risk of hypertension associated with parental hypertension: the Johns Hopkins Precursors Study. Arch Intern Med. 2008;168:643–8.
Leggio M, Lombardi M, Caldarone E, Severi P, D’Emidio S, Armeni M, et al. The relationship between obesity and hypertension: An updated comprehensive overview on vicious twins. Hypertens Res. 2017;40:947–63.
Oparil S, Acelajado MC, Bakris GL, Berlowitz DR, Cífková R, Dominiczak AF, et al. Hypertension. Nat Rev Dis Prim. 2018;4:18014.
Zhao YC, Zhao GJ, Chen Z, She ZG, Cai J, Li H. Nonalcoholic fatty liver disease: An emerging driver of hypertension. Hypertension. 2020;75:275–84.
Matsubara K, Yamamoto Y, Sonoyama K, Igawa G, Furuse M, Yatsuhashi T, et al. Current status of lipid management of hypertensive patients. Hypertens Res. 2003;26:699–704.
Park C, Fang J, Hawkins NA, Wang G. Comorbidity status and annual total medical expenditures in U.S. hypertensive adults. Am J Prev Med. 2017;53:S172–S81.
Machlin SR, Soni A. Health care expenditures for adults with multiple treated chronic conditions: Estimates from the Medical Expenditure Panel Survey, 2009. Prev Chronic Dis. 2013;10:E63.
Garg PR, Salam K, Saraswathy KN. Nonhigh-density lipoprotein cholesterol: A better marker of risk for hypertension than the low-density lipoprotein cholesterol. Int J Stroke. 2014;9:E33.
Lu K, Ding R, Wang L, Wu S, Chen J, Hu D. Association between prevalence of hypertension and components of metabolic syndrome: The data from Kailuan community. Clin Exp Hypertens. 2015;37:303–7.
Lin YH, Liu YH, Wu DW, Su HM, Chen SC. Dyslipidemia increases the risk of incident hypertension in a large Taiwanese population follow-up study. Nutrients. 2022;14:3277.
Varbo A, Benn M, Tybjærg-Hansen A, Nordestgaard BG. Elevated remnant cholesterol causes both low-grade inflammation and ischemic heart disease, whereas elevated low-density lipoprotein cholesterol causes ischemic heart disease without inflammation. Circulation. 2013;128:1298–309.
Zhang K, Jiang Y, Wang Y, Suo C, Xu K, Zhu Z, et al. Associations of arterial stiffness and carotid atherosclerosis with cerebral small vessel disease in a rural community-based population. J Atheroscler Thromb. 2020;27:922–33.
Xing Y, Rainey WE, Apolzan JW, Francone OL, Harris RB, Bollag WB. Adrenal cell aldosterone production is stimulated by very-low-density lipoprotein (VLDL). Endocrinology. 2012;153:721–31.
Saha S, Bornstein SR, Graessler J, Kopprasch S. Very-low-density lipoprotein mediates transcriptional regulation of aldosterone synthase in human adrenocortical cells through multiple signaling pathways. Cell Tissue Res. 2012;348:71–80.
Huh JH, Roh E, Lee SJ, Ihm SH, Han KD, Kang JG. Remnant cholesterol is an independent predictor of type 2 diabetes: A nationwide population-based cohort study. Diabetes Care. 2022;46:305–12.
Hu X, Liu Q, Guo X, Wang W, Yu B, Liang B, et al. The role of remnant cholesterol beyond low-density lipoprotein cholesterol in diabetes mellitus. Cardiovasc Diabetol. 2022;21:117.
Quispe R, Martin SS, Jones SR. Triglycerides to high-density lipoprotein-cholesterol ratio, glycemic control and cardiovascular risk in obese patients with type 2 diabetes. Curr Opin Endocrinol Diabetes Obes. 2016;23:150–6.
Acknowledgements
We would like to express our gratitude to the investigators, staff, and participants of the UK Biobank study for their valuable contributions to this research.
Funding
This work was supported by grants from the National Natural Science Foundation of China (82170457, 82371573, 82200306); Guangdong Basic and Applied Basic Research Foundation (2023A1515011730, 2022A1515011920, 2021A1515111092).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guo, DC., Gao, JW., Wang, X. et al. Remnant cholesterol and risk of incident hypertension: a population-based prospective cohort study. Hypertens Res 47, 1157–1166 (2024). https://doi.org/10.1038/s41440-023-01558-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01558-7
Keywords
This article is cited by
-
Is remnant cholesterol a new therapeutic target for preventing hypertension?
Hypertension Research (2024)