Abstract
The purpose of this investigation was to evaluate the influence of hypertension on left atrial (LA) function in patients with moderate and severe AS. This cross-sectional study included 121 patients with moderate and severe AS and preserved left ventricular (LV) ejection fraction ( > 50%) and 79 age-matched controls who underwent a comprehensive echocardiographic examination. LA phasic function was determined by both volumetric and strain methods. Our findings showed that the LV ejection fraction was similar between hypertensive and normotensive AS patients. Maximal, minimal, and pre-A LA volume indexes gradually increased from controls to moderate-to-severe AS patients. The total, passive and active LA emptying fraction (EF) gradually decreased in the same direction. LA phasic function estimated with strain analysis showed that reservoir, conduit, and pump LA phasic functions were lower in all AS patients than in normotensive controls. However, there was no significant difference between moderate and severe AS except in LA pump function, which was lower in severe AS. Differences in LA phasic function were more prominent in volumetric than in strain analyses. Blood pressure, LV mass index, and AS severity were independent of other clinical and echocardiographic parameters associated with LA phasic function in patients with AS. In conclusion, hypertension has an additive impact on LA phasic function in patients with moderate and severe AS. Blood pressure and AS severity were independently associated with LA phasic function parameters in AS patients. Volumetric assessment of LA phasic function should not be completely replaced with strain analysis.
Similar content being viewed by others
Introduction
The importance of left atrial (LA) function was first shown in patients with atrial fibrillation and patients with mitral valve disease (both stenosis and regurgitation) [1]. Only recently was LA phasic function demonstrated in other cardiovascular diseases and even in the global population [2, 3]. Although the significance of LA remodeling is highly appreciated, the only parameter that is validated and widely accepted is maximal LA volume (LAVmax) and its value indexed for body surface area.
Previous studies have shown the importance of LA remodeling in patients with aortic stenosis (AS) and especially its significance in the occurrence of atrial fibrillation [4, 5] and the development of heart failure symptoms in these patients [6]. The reverse remodeling of the LA after transcatheter aortic valve implantation or surgical replacement has received special attention in the last several years [7, 8].
The importance of LA remodeling in arterial hypertension has also been addressed in the last decade. Our study group showed the presence of LA dysfunction in hypertensive patients with different 24-hour blood pressure and LV geometry patterns [9, 10]. Other groups showed that LA volumes have predictive value in the occurrence of atrial fibrillation in the hypertensive population [11].
To our knowledge, no previous study has investigated the influence of hypertension on LA remodeling in patients with moderate and severe AS. The rationales for this study are the fact that hypertension is highly prevalent among AS patients and the finding that it represents a very important comorbidity that could additionally deteriorate LA function in AS patients and provoke the occurrence of atrial fibrillation or earlier heart failure symptom development. This is especially important in patients with moderate AS because the guidelines for the surgical or interventional approach in these patients are still not established, but symptoms in these patients represent an important criterion that favors intervention.
The primary aim of the present study was to investigate LA phasic function using volumetric and strain analyses in patients with moderate and severe AS with and without arterial hypertension. The secondary aim of this investigation was to assess which clinical and echocardiographic parameters were independently associated with LA phasic function in patients with AS.
Methodology
This cross-sectional study included 200 patients: 79 controls without AS, 54 patients with moderate AS and 67 subjects with severe AS and preserved LV ejection fraction ( > 50%).
Exclusion criteria were symptoms or signs of heart failure, coronary artery disease, permanent atrial fibrillation, congenital heart disease, more than mild valvular heart disease (other than aortic stenosis), previous operation of cardiac valves or myocardial revascularization, liver or kidney failure, and poor echocardiographic window. Diabetes was an exclusion criterion only in the normotensive control group.
Arterial pressure was measured in the morning hours as the average value of two consecutive measurements obtained within an interval of 5–10 min. Measurements were obtained with the patient in the sitting position after the subject had rested for at least 5minutes in that position. Blood pressure was obtained by a conventional sphygmomanometer. As stated in the guidelines, arterial hypertension was defined as increased systolic and/or diastolic BP. Anthropometric measures (height, weight) and laboratory analyses (levels of fasting glucose, creatinine, and total cholesterol) were obtained in all the study participants. Data regarding medications were obtained from all the study participants. Body mass index (BMI) and body surface area (BSA) were calculated for each patient. Not all hypertensive patients were treated with antihypertensive therapy because in some, hypertension had been recently discovered and they had not yet started the therapy or they started therapy only a few days or weeks before the echocardiographic examination. Some of the patients were not aware of arterial hypertension and were therefore not treated. The local Ethics Committee approved this study, and informed consent was obtained from all the participants.
Echocardiography
Echocardiographic examinations were performed using a commercially available Vivid 7 (GE Vingmed, Horten, Norway) ultrasound machine.
LV diameters, posterior wall, and septum thickness were measured according to the current recommendations [12]. The LV ejection fraction (EF) was calculated using the biplane Simpson’s method. LV mass was computed using the American Society for Echocardiography formula [12] and indexed for body surface area.
Pulsed-wave Doppler evaluation of transmitral LV flow was obtained in the apical four-chamber view [13]. Tissue Doppler imaging was used to obtain LV myocardial velocities in the apical four-chamber view, with a sample volume placed at the septal and lateral segments of the mitral annulus during early diastole (e´). The average of the peak early diastolic relaxation velocity (e´) of the septal and lateral mitral annulus was calculated, and the E/e´ ratio was analyzed.
A continuous-wave Doppler was used to evaluate the peak aortic velocity and the peak and mean transaortic pressure gradients, which were calculated using the simplified Bernoulli equation [14]. Peak aortic velocity and peak and mean gradients were evaluated in the apical five-chamber or right parasternal view depending on where the highest velocity signal and gradients were obtained. The aortic valve area was computed from the continuity equation according to previously published guidelines [14]. Moderate AS was defined when 1.0 ≤ AVA < 1.5 cm2 and severe AS when AVA < 1 cm2 [14].
2DE assessment of LA volumes and function
LA phasic function was determined by volumetric and strain analyses. LA volumes were obtained in three different parts of the cardiac cycle: maximal LA volume was calculated just before mitral valve opening, pre-A (pre-atrial contraction) LA volume was evaluated at the beginning of atrial systole (peak of the P wave on ECG), and minimal LA volume was assessed at mitral valve closure [15, 16]. All LA volumes were determined according to the biplane method in four- and two-chamber views, and all the values were indexed for BSA. The total emptying volume (an LA reservoir function parameter) was calculated as the difference between the maximum and minimum LA volume; passive emptying volume (an LA conduit function parameter) was computed as the difference between maximum and pre-A LA volume; and active emptying volume (an LA booster function parameter) was calculated as the difference between pre-A and minimum LA volume [16]. The total emptying fraction (EF) was calculated as the ratio between total emptying volume and maximum LA volumes, passive EF was computed as the ratio between passive and maximum, and active EF was evaluated as the proportion between active and pre-A LA volumes.
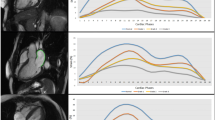
2DE strain imaging was performed in the apical four- and two-chamber views [16] using Echo PAC 201 (GE-Healthcare, Horten, Norway) in the 2DE strain analysis. LA strain was measured from the peak of a P wave to the peak of the P wave in the next cardiac cycle. It was not feasible to perform an LA strain evaluation in seven subjects because > 2 segments were not adequately traced. These subjects were equally distributed among the controls (3) and the AS patients (4). The feasibility in the control group was 96%, whereas that in the AS group was 97%. The LA endocardium was manually traced, and the average longitudinal strain curve was automatically provided by software. This curve included a negative deflection (LASct, a parameter of LA active contraction) and a positive deflection during LA filling (LAScd, a parameter of LA conduit function). Their summation represented LASr, a parameter of the LA reservoir function. LA strains were computed by averaging the values obtained in four- and two-chamber apical views. The software provided six strain curves for six different LA segments in each view (four- and two-chamber views), so that 12 LA segments were explored in each subject. However, to facilitate the calculation of longitudinal strain, the software provided one curve that represented the average longitudinal strain of six segments in the four- and two-chamber views. Figure 1 shows the methodology used for LA longitudinal strain evaluation in the present study. The feasibility of LA strain evaluation was 96% in the control group and 97% in the AS group.
Statistical analysis
All the parameters were tested for normal distribution using the Kolmogorov–Smirnov test. Continuous variables are presented as the mean ± standard deviation and were compared by analysis of variance if they showed a normal distribution. Tukey’s HSD post hoc analysis was used for comparisons between different groups. Differences in proportions were compared using the χ² or the Fischer’s exact test, where appropriate. Univariate and multivariate regression analyses were used to determine the relationships between different clinical and echocardiographic parameters and LA phasic function parameters (volumes and strain). The variable entry into the multivariate analyses required a p value ≤ 0.10 in the univariate analyses. A p value < 0.05 was considered statistically significant.
Results
There were no differences in age, BMI, or gender distribution between the observed groups (Table 1). Plasma glucose, total cholesterol, and creatinine levels were similar between the groups (Table 1). All hypertensive patients (with and without AS) had significantly higher blood pressure values than were found in the normotensive subjects (Table 1). Diabetes was equally distributed in all the groups except the normotensive control group, in which diabetes was excluded by definition. Antihypertensive groups and statins were equally presented in all hypertensive subjects (Table 1).
Echocardiography
There was no difference in LV diameter between the study groups (Table 2). The LV mass index gradually and significantly increased from the controls to moderate AS patients to severe AS patients (Table 2). LV EF was lower in the hypertensive patients with severe AS than in the normotensive controls (Table 2). The parameters related to LV diastolic function (E/A and E/e’) were significantly worse in the hypertensive patients with severe AS than in the controls (normotensive and hypertensive).
By definition, AV gradients significantly increased and AV area significantly decreased from the controls to moderate AS patients to severe AS patients (Table 2). AV gradients and AV area were similar between the normotensive and hypertensive patients with moderate and severe AS (Table 2). Stroke volume was lower in the patients with moderate and severe AS than in the controls. PAP was somewhat higher in the patients with AS than in the control subjects.
LA phasic function
Table 3 summarizes the data on normotensive and hypertensive controls and normotensive and hypertensive patients with moderate and severe AS. Maximal and minimal LA volume indexes were significantly higher in the normotensive and hypertensive patients with AS (moderate and severe) than in the controls (normotensive and hypertensive) (Table 3). The hypertensive AS patients had significantly higher maximal and minimal LA volume indexes than those found in the normotensive AS patients. The pre-A LA volume index and total, passive and active LAEF were significantly lower in all AS patients than in the controls (Table 3). LASr and LAScd were significantly lower in the AS patients than in the controls (Table 3). LASct was lower than in the controls only in the hypertensive AS patients.
Maximal, minimal, and pre-A LA volume indexes gradually increased from the controls, through the moderate AS patients, and then in the severe AS patients (Table 4). Interestingly, the indexed LA volumes in the hypertensive patients with severe AS were significantly higher than those in the other study groups (Table 4). However, among the patients with moderate AS, there was no significant difference between the hypertensive and the normotensive patients (Table 4).
Total, passive and active LAEF gradually decreased from the control group through the moderate AS patients and then to the severe AS patients (Table 4). In hypertensive moderate AS and all severe AS patients, all LA phasic functions (reservoir, conduit and active) were significantly lower than those found in the controls. Active LA function was significantly lower in the hypertensive patients with severe AS than in the controls and moderate AS patients, regardless of their blood pressure status (Table 4).
LA phasic function estimated with strain analysis showed that all three types of LA strains (LASr, LASr, and LASct), which represent the reservoir, conduit and active LA phasic functions, respectively, were lower in all AS patients than in the normotensive controls (Table 3). Reservoir and conduit LA functions were significantly lower in the patients with severe AS than in the controls (normotensive and hypertensive); reservoir LA function was also lower in patients with severe AS than in the normotensive patients with moderate AS (Table 4).
Univariate and multivariate regression analysis
Systolic blood pressure, E/e’, LV mass index, and the mean AV gradient were associated with LA phasic functions (reservoir, conduit, and active) as assessed by the volumetric method (Table 5). The same parameters were related to global LA longitudinal strain. However, for most of the parameters, systolic blood pressure, LV mass index and the mean AV gradient were independently associated with the parameters related to LA phasic function (Table 5).
Discussion
In the following discussion, several important findings from the present investigation will be addressed: (i) all LA volumes that represent LA reservoir and conduit and pump functions gradually increased from the controls across moderate AS subjects to severe AS patients; (ii) the LA EFs that determine LA phasic function gradually decreased in relation to the increases in LA volumes; (iii) volume-derived analysis revealed that there were more pronounced differences than the strain-derived evaluation of LA phasic function; (iv) although there was a trend toward a reduction in LA volume and strain parameters in hypertensive AS patients, there was no statistically significant difference between normotensive and hypertensive AS patients; (v) blood pressure, the LV mass index, and AS severity were independently associated with LA phasic function in patients with moderate and severe AS.
The majority of investigations that have studied LA function in AS have included exclusively severe AS patients or only patients with AS without dividing them into subgroups according to AS severity [5, 6, 17,18,19,20]. There is a lack of investigations that have compared LA phasic function between patients with moderate and severe AS, and the data regarding the influence of hypertension on LA phasic function in AS patients are still missing.
There is agreement among different authors that LA phasic function, when determined by volumes and strain (strain rates), is deteriorated in AS patients [5, 6, 17, 18, 20]. Interestingly, Salas-Pacheco et al. [19] did not find a difference in LA volumes and strains resembling the LA reservoir, conduit and pump function between patients with AS and those with aortic regurgitation. Imanishi et al. [6] divided patients with severe AS into symptomatic and asymptomatic groups and demonstrated that all three LA phasic functions determined based on LA strain and strain rates were significantly lower in symptomatic AS patients. O’Connor et al. [17] used LA strain rates to perform their evaluation and found that LA reservoir dysfunction was associated with LV filling pressure, LA conduit dysfunction was related to LV relaxation, and booster pump LA dysfunction was correlated with the severity of AS and late LV diastolic function.
Our findings also confirm that there is a gradual and significant reduction in LA reservoir, conduit, and pump functions from the controls across moderate AS patients and to severe AS patients, indicating the importance of AS severity in LA remodeling. Despite a trend toward LA function to deteriorate more in hypertensive AS patients than in their normotensive counterparts, we did not find any statistically significant difference in LA function between the normotensive and hypertensive AS patients. The only significant difference was detected in LA booster pump function in the group of patients with severe AS. In this group of patients, the minimal LA volume was significantly higher in hypertensive than in normotensive subjects. However, there was no difference in active LAEF or LASct between these groups. Imanishi et al. [5] found that LA booster pump function was the only independent predictor of postoperative atrial fibrillation in AS patients, and Russo et al. [21] previously demonstrated that minimal LAV was a better predictor than maximal LAV of LV diastolic function. Interestingly, in our previous studies regarding LA function in arterial hypertension, we demonstrated that LA conduit and reservoir functions were lower, whereas LA booster pump function was compensatorily higher in the untreated hypertensive population [9, 10]. This was the rational for conducting the current study. It seems that AS additionally deteriorates LA function and weakens the compensatory mechanism of arterial hypertension, thus, at least at the beginning, improving LA booster function.
The strain evaluation of the LA phasic function is easier and faster to perform than volumetric assessment. This is the reason that researchers usually prefer strain over volumetric LA phasic function assessment. However, observing consistency between volumetric and strain findings is always beneficial. Our study shows that there is a more prominent difference in LA phasic function when it is evaluated with the volumetric method than when the strain method is used, a result that emphasizes the importance of the notion that volumetric assessment should obviously not be completely replaced with the strain approach. Cameli et al. [22] showed that LA longitudinal strain has better sensitivity and specificity for the prediction of adverse cardiovascular outcomes than were achieved by LAVI and LAEF. However, there was no statistically significant difference between the results obtained by LA strain and LAVI. In addition, the authors used population-specific cutoff values for LA parameters, and these could not be interpolated in our investigation.
The effect of arterial hypertension on LA function in AS has not been investigated thus far. Most investigators have not even included blood pressure as a possible predictor in correlation and regression studies [18,19,20], and O’Connor et al. [17] reported that they found no correlation between LA strain rates and blood pressure. The results of our study show that systolic blood pressure was independent of other clinical and echocardiographic parameters associated with LA reservoir and pump function estimated by the volumetric method. However, the correlation between LA phasic function and LV mass index and AS severity were shown in previous studies [17, 18, 20].
The most relevant clinical implication of this study is that LA phasic function showed a trend toward increasing deterioration with increasing AS severity and in the presence of arterial hypertension, and these effects had an additive negative effect on LA remodeling in AS patients. Symptomatic patients with moderate AS could possibly benefit from the evaluation of LA function because their symptoms might be related to arterial hypertension and consequent LA impairment and LV diastolic dysfunction.
Limitations
There are several limitations to the current study. The investigation included a limited number of AS patients, and this could be the main reason for the lack of a statistically significant difference between normotensive and hypertensive AS subjects regardless of the significant trend for LA phasic function to deteriorate in hypertensive participants. The results of echocardiographic evaluation of LA function could be significantly influenced by the acquisition quality, but this is a common limitation for all echocardiographic studies and could not be avoided. The influence of coronary artery disease could not be completely eliminated because coronary angiography was not performed in all patients. The causal relationships among AS, hypertension, and LA phasic function could not be determined due to the cross-sectional nature of this research.
Conclusion
LA phasic function reflects an important set of parameters that are associated with cardiovascular morbidity in AS patients. Our study shows that AS severity and hypertension are related to a worsening of LA function and that hypertension is a relevant factor that could additionally deteriorate LA remodeling in AS patients. The patients with severe AS had significantly more impaired LA phasic function than was found in the subjects with moderate AS. There was also a significant trend for deterioration in LA phasic function to be higher in the hypertensive patients than in the normotensive individuals with both moderate and severe AS. However, this relationship was not significant, probably owing to the small sample size. Future studies should be directed toward determining the influence of arterial hypertension on LA remodeling and particularly the effects of hypertension in patients with moderate AS, in whom there are still many uncertainties regarding the necessity and timing of intervention.
References
Ancona R, Pinto SC, Caso P, D’Andrea A, Di Salvo G, Arenga F, et al. Left atrium by echocardiography in clinical practice: from conventional methods to new echocardiographic techniques. Sci World J. 2014;451042: https://doi.org/10.1155/2014/451042.
Patel DA, Lavie CJ, Milani RV, Ventura HO. Left atrial volume index predictive of mortality independent of left ventricular geometry in a large clinical cohort with preserved ejection fraction. Mayo Clin Proc. 2011;86:730–7.
Gupta S, Matulevicius SA, Ayers CR, Berry JD, Patel PC, Markham DW, et al. Left atrial structure and function and clinical outcomes in the general population. Eur Heart J. 2013;34:278–85.
Pernigo M, Benfari G, Geremia G, Noni M, Borio G, Mazzali G, et al. Atrial function as an independent predictor of postoperative atrial fibrillation in patients undergoing aortic valve surgery for severe aortic stenosis. J Am Soc Echocardiogr. 2017;30:956–65.
Imanishi J, Tanaka H, Sawa T, Motoji Y, Miyoshi T, Mochizuki Y, et al. Left atrial booster-pump function as a predictive parameter for new-onset postoperative atrial fibrillation in patients with severe aortic stenosis. Int J Cardiovasc Imaging. 2014;30:295–304.
Imanishi J, Tanaka H, Sawa T, Motoji Y, Miyoshi T, Mochizuki Y, et al. Association of left atrial booster-pump function with heart failure symptoms in patients with severe aortic stenosis and preserved left ventricular ejection fraction. Echocardiography. 2015;32:758–67.
Spethmann S, Dreger H, Baldenhofer G, Stuer K, Saghabalyan D, Muller E, et al. Short-term effects of transcatheter aortic valve implantation on left atrial mechanics and left ventricular diastolic function. J Am Soc Echocardiogr. 2013;26:64–71.
Lisi M, Henein MY, Cameli M, Ballo P, Reccia R, Bennati E, et al. Severity of aortic stenosis predicts early post-operative normalization of left atrial size and function detected by myocardial strain. Int J Cardiol. 2013;167:1450–5.
Tadic M, Cuspidi C, Pencic B, Celic V, Mancia G. The relationship between nighttime hypertension and left atrial function. J Clin Hypertens. 2017;19:1096–104.
Tadic M, Cuspidi C, Pencic B, Kocijancic V, Celic V. The influence of left ventricular geometry on left atrial phasic function in hypertensive patients. Blood Press. 2015;24:361–8.
Chen Y, Sato H, Watanabe N, Adachi T, Kodani N, Sato M, et al. Factors influencing left atrial volume in treated hypertension. J Cardiol. 2012;60:133–8.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr. 2015;28:1–39.
Quinones MA, Otto CM, Stoddard M, Waggoner A, Zoghbi WA. Doppler Quantification Task Force of the Nomenclature and Standards Committee of the American Society of Echocardiography. Recommendations for quantification of Doppler echocardiography: a report from the Doppler quantification task force of the nomenclature and standards committee of the American Society of Echocardiography. J Am Soc Echocardiogr. 2002;15:167–84.
Baumgartner H, Hung J, Bermejo J, Chambers JB, Edvardsen T, Goldstein S, et al. Recommendations on the echocardiographic assessment of aortic valve stenosis: a focused update from the European association of cardiovascular imaging and the American Society of Echocardiography. J Am Soc Echocardiogr. 2017;30:372–92.
Miglioranza MH, Badano LP, Mihăilă S, Peluso D, Cucchini U, Soriani N, et al. Physiologic determinants of left atrial longitudinal strain: a two-dimensional speckle-tracking and three-dimensional echocardiographic study in healthy volunteers. J Am Soc Echocardiogr. 2016;29:1023–34.
Badano LP, Kolias TJ, Muraru D, Abraham TP, Aurigemma G, Edvardsen T, et al. Industry representatives. Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging. 2018;19:591–600.
O’Connor K, Magne J, Rosca M, Piérard LA, Lancellotti P. Impact of aortic valve stenosis on left atrial phasic function. Am J Cardiol. 2010;106:1157–62.
Rusinarua D, Bohbota Y, Salaunc E, Donald E, Calsatac AC, Galli E, et al. Determinants of left atrial volume index in patients with aortic stenosis: a multicentre pilot study. Arch Cardiovasc Dis. 2017;110:525–33.
Salas-Pacheco JL, Ávila-Vanzzini N, Eugenia RE, Arias-Godínez JA. Left atrium function by 2D speckle tracking in aortic valve disease. Echocardiography. 2016;33:1828–34.
Galli E, Fournet M, Chabanne C, Lelong B, Leguerrier A, Flecher E, et al. Prognostic value of left atrial reservoir function in patients with severe aortic stenosis: a 2D speckle-tracking echocardiographic study. Eur Heart J. 2016;17:533–41.
Russo C, Jin Z, Homma S, Rundek T, Elkind MS, Sacco RL, et al. Left atrial minimum volume and reservoir function as correlates of left ventricular diastolic function: impact of left ventricular systolic function. Heart. 2012;98:813–20.
Cameli M, Lisi M, Focardi M, Reccia R, Natali BM, Sparla S, et al. Left atrial deformation analysis by speckle tracking echocardiography for prediction of cardiovascular outcomes. Am J Cardiol. 2012;110:264–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tadic, M., Cuspidi, C., Pencic, B. et al. Left atrial phasic function in hypertensive patients with significant aortic stenosis and preserved ejection fraction. Hypertens Res 42, 1200–1208 (2019). https://doi.org/10.1038/s41440-019-0256-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0256-0
Keywords
This article is cited by
-
Left atrial stiffness: a novel marker of hypertension-mediated organ damage on the horizon?
Hypertension Research (2021)