Abstract
The aim was to investigate the risk of developing type 2 diabetes according to blood pressure (BP) levels and presence or absence of hypertensive treatment. This 5-year cohort study comprised 3508 Japanese adults aged 30–74 years without diabetes who had undergone a medical checkup including a 75-g oral glucose tolerance test (OGTT) between April 2008 and March 2009 at Saku Central Hospital. Participants receiving antihypertensive treatment were categorized into controlled hypertension ( < 140/90 mmHg) or uncontrolled hypertension ( ≥ 140/90 mmHg) groups. Participants not receiving antihypertensive treatment were categorized: optimal BP ( < 120/80 mmHg), normal BP (120–129/80–84 mmHg), high-normal BP (130–139/85–89 mmHg), grade I hypertension (140–159/90–99 mmHg), and grade II/III hypertension ( ≥ 160/100 mmHg). Hazard ratios and 95% confidence intervals for the incidence of type 2 diabetes as defined by the 75-g OGTT were estimated using multivariable-adjusted Cox proportional hazard models in reference to optimal BP. During an average of 4.4 years of follow-up, 295 participants developed type 2 diabetes. Those with high-normal BP, grade I hypertension, grade II/III hypertension, and uncontrolled hypertension were at significantly higher risk for developing type 2 diabetes, with hazard ratios (95% confidence intervals) of 1.53 (1.03–2.29), 1.53 (1.02–2.32), 2.19 (1.01–4.77), and 1.81 (1.10–2.99), respectively. In conclusion, compared with those with optimal BP, individuals with BP ≥ 130/85 mmHg not receiving antihypertensive treatment and uncontrolled hypertensives with BP ≥ 140/90 mmHg receiving antihypertensive treatment were at a significantly higher risk for developing type 2 diabetes.
Similar content being viewed by others
Introduction
The worldwide prevalence of both hypertension and diabetes are alarmingly high. As of 2015, the age-standard prevalence of hypertension was 24.1% in men and 20.1% in women, and the prevalence of diabetes was 8.8% [1, 2]. Furthermore, although hypertension and diabetes mellitus are characterized by different pathophysiologies, they have much in common [3]. Because both hypertension and type 2 diabetes increase the risk for developing severe conditions such as cardiovascular and kidney disease [3,4,5,6], it is important to avoid risk accumulation.
As reported by several prospective studies, hypertensives who had blood pressure (BP) ≥ 140/90 mmHg or were receiving antihypertensive medication had a higher risk of developing type 2 diabetes than normotensives who had BP < 140/90 mmHg and were not receiving antihypertensive medication [7,8,9,10,11,12,13]. Furthermore, it has been reported that those with prehypertension who had BP 120–139/80–89 mmHg and were not receiving antihypertensive medication had ~ a 1.5- to twofold higher risk of developing type 2 diabetes compared with those who had optimal BP < 120/80 mmHg and were not receiving antihypertensive medication [8, 11, 14]. In a hospital-based study involving patients receiving antihypertensive medication, uncontrolled hypertensives who had BP ≥ 140/90 mmHg had a 2.1-fold higher risk of developing type 2 diabetes compared with controlled patients who had BP < 140/90 mmHg [15]. However, to our knowledge, no studies have compared the risk of developing type 2 diabetes between those with untreated optimal BP and those with untreated high BP (≥ 140/90 mmHg), treated and controlled hypertension, or treated but uncontrolled hypertension.
Therefore, to detect hypertensives at particularly high risk of type 2 diabetes, we conducted a Japanese cohort study to investigate the risk of developing type 2 diabetes according to BP levels and presence or absence of antihypertensive treatment in hypertensives.
Methods
Study participants
The details of this study have been described previously [16,17,18]. The participants in the present study were 4587 individuals aged 30–74 years had undergone comprehensive medical checkups including a 75-g oral glucose tolerance test (OGTT) over 2 days and 1 night between April 2008 and March 2009 (baseline) at Saku Central Hospital. Although these checkups are generally expensive in Japan, those at Saku Central Hospital are either relatively inexpensive or free, owing to subsidization of costs by administrations and employers. As a result, many community residents could undergo these examinations. These subjects might represent a healthier group than the general population because they voluntarily underwent a checkup. Of these individuals, 715 were excluded because of having diabetes at baseline (fasting plasma glucose (FPG) ≥ 7.0 mmol/l and/or 2-h plasma glucose (PG) during a 75-g OGTT ≥ 11.1 mmol/l and/or a history of diabetes). Of these individuals, 3509 underwent at least one follow-up examination before the end of March 2014. After excluding one participant because of missing data, a total of 3508 participants were included in the present analysis. The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Bord of Saku Central Hospital (committee approval number: R201404-02) and the Ethics Committee of Teikyo University (committee approval number:17-040). An opt-out consent procedure was implemented, and the standard questionnaires included opt-out information.
Data collection and definitions at baseline
BP measurement and categorization
BP was measured twice by trained nurses using the ES-H55 device with standard arm cuff (TERUMO Co. Ltd, Tokyo, Japan) [19], a semiautomatic device based on the cuff-oscillometric method, with participants in a seated position after at least a 5-min rest. In the present study, the mean of the two measurement values was used. Participants receiving antihypertensive treatment were categorized into either a controlled hypertension (< 140 mmHg systolic and < 90 mmHg diastolic) or an uncontrolled hypertension (≥ 140 mmHg systolic and/or ≥ 90 mmHg diastolic) group. Participants not receiving antihypertensive treatment were categorized into five groups based on definitions of the Japan Society of Hypertension as follows: optimal BP (< 120 mmHg systolic and < 80 mmHg diastolic); normal BP (120–129 mmHg systolic or 80–84 mmHg diastolic); high-normal BP (130–139 mmHg systolic or 85–89 mmHg diastolic); grade I hypertension (140–159 mmHg systolic or 90–99 mmHg diastolic); and grade II/III hypertension (≥ 160 mmHg systolic or ≥ 100 mmHg diastolic) [20].
75-g OGTT and blood test
During the second morning after an overnight fast (10 h), all participants underwent a standard 75-g OGTT. Blood samples were obtained at 0 (fasting), 30, 60, and 120 min, with blood glucose measured on all four occasions and serum insulin concentrations measured at 0 and 30 min in the clinical laboratory of Saku Central Hospital. Prediabetes was defined as having either impaired fasting glucose (FPG 6.1–6.9 mmol/l and 2-h PG < 11.1 mmol/l) or impaired glucose tolerance (FPG < 6.1 mmol/l and 2-h PG 7.8–11.0 mmol/l). Homeostasis model assessment of insulin resistance (HOMA-IR) was calculated as follows: (fasting glucose (mmol/l) × fasting insulin (μU/ml)/22.5) [21]. The insulinogenic index was calculated as follows: (serum insulin 30 min after OGTT (pmol/l)−fasting serum insulin (pmol/l))/(blood glucose 30 min after OGTT (mmol/l)−fasting blood glucose (mmol/l)) [22]. Dyslipidemia was defined as high-density lipoprotein cholesterol < 1.03 mmol/l and/or low-density lipoprotein cholesterol cholesterol ≥ 3.62 mmol/l and/or triglycerides ≥ 1.69 mmol/l.
Other measurements
Participants completed a questionnaire that included demographic characteristics, medical history, alcohol consumption, physical activity (0, 1–59, or 60 min/week), and smoking habit (never, current, quit). Alcohol consumption was categorized based on the recommended values by the Ministry of Health, Labour and Welfare in Japan: non-drinker (0 g/week), moderate drinker (< 140 g/week in men and < 70 g/week in women), and heavy drinker (≤ 140 g/week in men and ≤ 70 g/week in women) [23]. Height and weight were measured while participants wore a hospital gown, and body mass index (BMI) was calculated as weight (kg) divided by the square of height (m). Obesity was defined as BMI ≥ 25.0 kg/m2.
Type 2 diabetes incidence and follow-up
All participants underwent annual follow-ups at Saku Central Hospital, including comprehensive medical checkups over 2 days and 1 night and a 75-g OGTT. The end of the follow-up period was March 2014. Of 3508 participants, 53.4%, 21.4%, 7.2%, 8.3%, and 9.7% underwent a medical checkup 5, 4, 3, 2, and 1 time, respectively, from baseline to March 2014. The incidence of type 2 diabetes was defined as a first diagnosis of a FPG level ≥ 7.0 mmol/L, a 2-h PG level ≥ 11.1 mmol/L, or receiving medical treatment for type 2 diabetes on the date of the visit. Individuals who did not develop type 2 diabetes during the follow-up period were censored on the date of their last examination.
Statistical analysis
Differences in characteristics according to BP categories were defined by an analysis of variance for normally distributed continuous data and a χ2 test for dichotomous and categorical data. The distributions of triglycerides, HOMA-IR, and insulinogenic index were skewed right, so the Kruskal–Wallis test was performed.
Cox proportional hazard models were used to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) of normal BP, high-normal BP, grade I hypertension, grade II/III hypertension, controlled hypertension, and uncontrolled hypertension for the incidence of type 2 diabetes in reference to optimal BP. The multivariable-adjusted model included age, sex, BMI (< 25 kg/m2 or ≥ 25 kg/m2), dyslipidemia, smoking status (never, current, quit), alcohol consumption (non-, moderate, or heavy), physical activity (0, 1–59, ≥ 60 min/week), family history of diabetes, and FPG at baseline.
The following additional models were analyzed: (1) the model in which the date of event was defined as the midpoint between the date of visit when the diabetes was diagnosed and the date of the previous visit, (2) the model that excluded participants who developed diabetes during the first 1.5 years, (3) the analysis using the same adjusted variables except FPG and included log-transformed HOMA-IR and the insulinogenic index at baseline, (4) the model including change in BMI from baseline to the end point, (5) the stratified analysis by sex, age (< 65 or ≥ 65 years old), BMI (< 25.0 or ≥ 25.0 kg/m2), prediabetes (presence or absence), and the number of visits until March 2014 (1–4 or 5 times) and (6) the model using the systolic BP and diastolic BP categories separately. The likelihood ratio test was used for the tests of interaction of sex, age, BMI, prediabetes, and number of visits. The differences of − 2 logarithm likelihood before and after, including the interaction term in each model, were tested using the χ2-test.
The percentages of prediabetes, impaired fasting glucose, and impaired glucose tolerance were calculated among the participants who developed type 2 diabetes.
All reported P values were two-tailed, and those < 0.05 were considered statistically significant. All data were analyzed using SPSS (version 22.0 J; IBM Japan, Tokyo, Japan).
Results
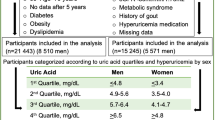
The mean age (standard deviation) of the participants was 58.4 (8.9) years old. Among the 3508 participants, 694 (19.8%) were receiving antihypertensive treatment, among whom, 129 (18.6%) had uncontrolled BP (systolic BP ≥ 140 mmHg and/or diastolic BP ≥ 90 mmHg). The 50th percentiles (25–75th percentiles) of systolic and diastolic BP were 120 (113–128) mmHg and 74 (67–80) mmHg in controlled hypertension, and 144 (140–152) mmHg and 90 (80–94) mmHg in uncontrolled hypertension, respectively. The baseline characteristics according to BP categories are shown in Table 1. All variables except for the percentage of family history of diabetes were significantly different among the BP categories.
During an average of 4.37 years of follow-up (median, 25–75th percentile: 4.97, 4.10–5.04 years), 295 participants developed type 2 diabetes. The adjusted HRs and 95% CIs according to BP categories are shown in Fig. 1. After adjustment for all confounding factors, those with high-normal BP, grade I hypertension, grade II/III hypertension, and uncontrolled hypertension had a significantly higher risk of developing type 2 diabetes, with HRs (95% CIs) of 1.53 (1.03–2.29), 1.53 (1.02–2.32), 2.19 (1.01–4.77), and 1.81 (1.10–2.99), respectively. The HRs and 95% CIs of confounding factors in the adjusted models are shown in Supplement Table 1. Age, smoking status, family history of diabetes, and FPG were significantly associated with the development of type 2 diabetes. In the analysis that defined the date of event as the midpoint between the date of the visit when diabetes was diagnosed and the date of the previous visit, the HRs (95% CIs) in those with optimal BP, normal BP, high-normal BP, grade I hypertension, grade II/III hypertension, controlled hypertension, and uncontrolled hypertension were 1.28 (0.89–1.83), 1.53 (1.02–2.28), 1.51 (1.00–2.28), 2.12 (0.97–4.61), 1.33 (0.95–1.87), and 1.79 (1.09–2.96), respectively. In the same way, the HRs (95% CIs) were 1.29 (0.85–1.95), 1.48 (0.92–2.36), 1.53 (0.94–2.50), 2.23 (0.89–5.60), 1.27 (0.85–1.91), and 1.29 (0.65–2.56), respectively, in the analysis that excluded participants who developed diabetes during first 1.5 years (n = 87).
Multivariable-adjusted hazard ratios and 95% confidence intervals for the development of diabetes according to blood pressure categories. Abbreviations: BP, blood pressure; CI, confidence interval; HR, hazard ratio; IR, incidence rate. Adjusted variables were age, sex, body mass index (< 25 kg/m2 or ≥ 25 kg/m2), dyslipidemia (absence or presence), smoking status (never, current, quit), alcohol consumption (non-, moderate, heavy), physical activity (0, 1–59, ≥ 60 min/week), family history of diabetes, and fasting plasma glucose level. Dyslipidemia was defined as high-density lipoprotein cholesterol < 1.03 mmol/l and/or low-density lipoprotein cholesterol cholesterol ≥ 3.62 mmol/l and/or triglycerides ≥ 1.69 mmol/l. The area of the square was proportional to the number of cases in each category. Incidence rates were per 1000 person years. *P < 0.05
The results of the HRs (95% CIs) adjusted for change in BMI, and log-transformed HOMA-IR and insulinogenic index instead of FPG are shown in Table 2. The risk associated with each BP category did not change notably after adjustment for log-transformed HOMA-IR and insulinogenic index; both were significantly associated with the development of type 2 diabetes, with HRs (95% CIs) of 2.66 (2.15–3.28) and 0.24 (0.20–0.29), respectively. Similarly, the risk associated with each BP category did not change notably, even after adjustment for change in BMI. Change in BMI was significantly associated with the development of type 2 diabetes, with a HR (95% CIs) of 1.25 (1.13–1.38). The results of stratified analyses are shown in Supplement Table 2. Because of small sample size, grade I hypertension and grade II/III hypertension were categorized in the same group. Although the HRs among participants without prediabetes were attenuated remarkably compared with results when participants were not stratified, no significant interaction was observed (all p values > 0.05).
The HRs (95% CIs) for systolic and diastolic BP are shown in Table 3. Both systolic BP and diastolic BP were associated with the development of type 2 diabetes among participants not receiving antihypertensive treatment. Among participants receiving antihypertensive treatment, systolic BP was not associated with the development of type 2 diabetes. The HR of diastolic BP ≥ 90 mmHg compared with < 90 mmHg was 1.75, although this finding was not statistically significant.
The percentages of impaired fasting glucose and impaired glucose tolerance at baseline among those who developed type 2 diabetes are shown in Fig. 2. Except for those with optimal BP and grade II/III hypertension, > 70% of the participants in each of the BP categories had impaired fasting glucose or impaired glucose tolerance at baseline. Participants with uncontrolled hypertension who developed type 2 diabetes (n = 21) had a particularly high percentage of prediabetes at baseline, and 57.1% (n = 12) and 38.1% (n = 8) had impaired fasting glucose and impaired glucose tolerance, respectively.
Discussion
The present study demonstrated that, compared with those with optimal BP and not receiving antihypertensive treatment, participants with high-normal BP, grade I hypertension, grade II/III hypertension, and uncontrolled hypertension, but not those with normal BP and controlled hypertension, were at a significantly higher risk of developing type 2 diabetes. These results were independent of age, sex, smoking status, physical activity, alcohol consumption, family history of diabetes, BMI, change in BMI, dyslipidemia and baseline FPG, HOMA-IR, and insulinogenic index. As a result of the analysis of systolic and diastolic BP separately, both systolic and diastolic BP were associated with the development of type 2 diabetes among those not receiving antihypertensive treatment. In addition, many of the participants who developed type 2 diabetes had impaired fasting glucose or impaired glucose tolerance at baseline, especially those with uncontrolled hyperte+nsion.
In the San Antonio Heart Study, compared with participants who had BP < 120/80 mmHg and were not receiving antihypertensive treatment, the risk of developing type 2 diabetes was 1.31-fold higher (not significant) and 1.69-fold higher (significant) among those with BP 120–129/80–84 mmHg not receiving antihypertensive treatment and those with BP 130–139/85–89 mmHg not receiving antihypertensive treatment, respectively [14]. Comparing with the HRs of normal BP and high-normal BP in the present study, the previous study supports the present results. In the Tehran Lipid and Glucose Study and a Korean study, the risk of developing hypertension, which was defined as BP ≥ 140/90 mmHg or receiving antihypertensive treatment for type 2 diabetes, was estimated as 1.65-fold and 1.51-fold higher (significant) compared with those with BP < 120/80 mmHg, respectively [8, 11]. The results of the present study provides more evidence that hypertensives with controlled BP < 140/90 mmHg who are receiving antihypertensive treatment do not have a significantly higher risk of developing type 2 diabetes compared with those with optimal BP. In the present study, after excluding those who developed type 2 diabetes during the first 1.5 years, the risk of uncontrolled hypertension was attenuated. These patients might have been diagnosed with diabetes based on small increases in blood glucose levels during early follow-up periods.
An unhealthy lifestyle is a common risk factor for both hypertension and type 2 diabetes [24,25,26,27,28,29]. Uncontrolled hypertension may reflect insufficient lifestyle modifications, which are another possible risk factor for type 2 diabetes. In the present study, those with uncontrolled hypertension had high percentages of obesity and alcohol consumption, which are well-known risk factors for treatment-resistant hypertension as well as type 2 diabetes [20, 30]. Although it was confirmed that the risk of uncontrolled hypertension remained significantly higher after adjusting for lifestyle risk factors at baseline, it was difficult to clarify the impact of detailed lifestyle modification during the follow-up period on the development of type 2 diabetes. Therefore, residual effects of these factors could still exist. In addition, it was possible that other lifestyle risk factors that were not be considered in the present study might increase the risk for type 2 diabetes. In the real world, those with high blood pressure have a high prevalence of unhealthy lifestyles, suggesting that lifestyle modification in individuals with BP levels of high normal or more and treated hypertension is important to prevent future occurrences of type 2 diabetes as well as to control blood pressure. In the present study, current smoking and changes in BMI were associated with an increased risk for type 2 diabetes among the lifestyle factors, suggesting that quitting smoking and preventing weight gain might be particularly effective for the prevention of type 2 diabetes.
High BP per se also may increase the risk of developing type 2 diabetes. One possible explanation for high BP increasing the risk of developing type 2 diabetes is insulin resistance [31,32,33]. In brief, high BP damages microvessels, resulting in a reduced capacity for insulin-mediated glucose uptake, that is, insulin resistance.
There are few studies investigating whether systolic BP or diastolic BP is more closely associated with the development of type 2 diabetes. A previous study involving community residents reported that both systolic BP and diastolic BP were associated with the risk for type 2 diabetes [10]. The results in the present study for those not receiving antihypertensive treatment in part support this previous study. However, clear associations were not observed among those receiving antihypertensive treatment. It has been reported that the association between BP levels and cardiovascular disease was weak among those receiving antihypertensive treatment [34]. Because office blood pressure level measured on a single occasion may be influenced by conditions before measurement, such as the time of taking medicine, evaluation of home blood pressure, which better reflects stable blood pressure levels in individuals, may be needed to clarify clear associations between systolic and diastolic BP and the development of type 2 diabetes among those receiving antihypertensive treatment.
To identify individuals at high risk for developing type 2 diabetes, blood glucose levels need to be followed up in those with high BP. In the present study, many of the individuals who developed type 2 diabetes had prediabetes at baseline. Of these, ~ 30% or more had impaired glucose tolerance (FPG < 6.1 mmol/l). Therefore, it is necessary to assess not only FPG, but also post-load glucose levels.
The strengths of the present study were that the participants were screened for type 2 diabetes over a 5-year period using a 75-g OGTT, and that the 10-h overnight fast before the 75-g OGTT was enforced by hospitalizing the participants the day prior to testing. However, this study also had some limitations. First, BP was only measured at the hospital, not in the participants’ homes. It has been reported that individuals with masked hypertension, in which high BP is seen at home, but not at the hospital, had a 1.7-fold higher risk of developing type 2 diabetes compared with individuals without high BP at the hospital or the home (not significant) [9]. Masked hypertension was included in the categories without high BP in the present study, so the risk associated with high BP might have been underestimated. Second, detailed information on antihypertensive treatments, such as types and number of medicines, were not available. Renin–angiotensin system blockers, particularly angiotensin II receptor blockers, were frequently used in Japan around the time of the present study [35]. These drugs have been reported to decrease the risk of developing type 2 diabetes [36, 37], which could be a reason why controlled hypertension was not associated with a high risk of developing type 2 diabetes. Further studies with detailed information regarding antihypertensive treatment are needed to clarify the reason for the difference in the risk for type 2 diabetes between patients with controlled and uncontrolled hypertension. Third, the follow-up period was short. The association between BP and developing type 2 diabetes was attenuated notably among those without prediabetes. A possible explanation was the small number of cases because of the short periods. Further studies with long follow-up periods were needed. Fourth, selection bias was possible because the study participants were individuals who had undergone routine comprehensive medical checkups. As reported by the National Health and Nutrition Survey in Japan in 2008, the prevalences of hypertension, defined as BP ≥ 140/90 mmHg, and of receiving medical treatment for hypertension were 33.4% and 16.8%, respectively, among Japanese adults aged 30–69 years [38]. The same prevalences were 12.3% and 19.9%, respectively, among those aged 30–69 years who had undergone medical checkups at Saku Central Hospital in 2008. Therefore, the participants in the present study were healthier than the general population in Japan.
In conclusion, individuals with BP ≥ 130/85 mmHg who were not receiving antihypertensive treatment and those with BP ≥ 140/90 mmHg who were receiving antihypertensive treatment had a significantly higher risk of developing type 2 diabetes compared with those with optimal BP who were not receiving antihypertensive treatment. These results suggest the importance of preventing hypertension and controlling BP among hypertensives to prevent the development of diabetes, and in turn, cardiovascular disease.
References
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;7:389. 37-355
International Diabetes Federation. IDF Diabetes Atlas 7th edn. http://www.diabetesatlas.org/. Accessed 13 February 2018.
Tatsumi Y, Ohkubo T. Hypertension with diabetes mellitus: significance from an epidemiological perspective for Japanese. Hypertens Res. 2017;40:795–806.
Yamagata K, Ishida K, Sairenchi T, Takahashi H, Ohba S, Shiigai T, et al. Risk factors for chronic kidney disease in a community-based population: a 10-year follow-up study. Kidney Int. 2007;71:159–166.
Hu G, Jousilahti P, Tuomilehto J. Joint effects of history of hypertension at baseline and type 2 diabetes at baseline and during follow-up on the risk of coronary heart disease. Eur Heart J. 2007;28:3059–3066.
Hu G, Sarti C, Jousilahti P, Peltonen M, Qiao Q, Antikainen R, et al. The impact of history of hypertension and type 2 diabetes at baseline on the incidence of stroke and stroke mortality. Stroke. 2005;36:2538–2543.
Waki K, Noda M, Sasaki S, Matsumura Y, Takahashi Y, Isogawa A. et al. JPHC Study Group. Alcohol consumption and other risk factors for self-reported diabetes among middle-aged Japanese: a population-based prospective study in the JPHC study cohort I. Diabet Med. 2005;22:323–331.
Kim MJ, Lim NK, Choi SJ, Park HY. Hypertension is an independent risk factor for type 2 diabetes: the Korean genome and epidemiology study. Hypertens Res. 2015;38:783–789.
Mancia G, Bombelli M, Facchetti R, Madotto F, Quarti-Trevano F, Grassi G, et al. Increased long-term risk of new-onset diabetes mellitus in white-coat and masked hypertension. J Hypertens. 2009;27:1672–1678.
Stahl CH, Novak M, Lappas G, Wilhelmsen L, Björck L, Hansson PO, et al. High-normal blood pressure and long-term risk of type 2 diabetes: 35-year prospective population based cohort study of men. BMC Cardiovasc Disord. 2012;12:89.
Derakhshan A, Bagherzadeh-Khiabani F, Arshi B, Ramezankhani A, Azizi F, Hadaegh F. Different combinations of glucose tolerance and blood pressure status and incident diabetes, hypertension, and chronic kidney disease. J Am Heart Assoc. 2016;5:e003917.
Weycker D, Nichols GA, O’Keeffe-Rosetti M, Edelsberg J, Vincze G, Khan ZM, et al. Excess risk of diabetes in persons with hypertension. J Diabetes Complications. 2009;23:330–336.
Conen D, Ridker PM, Mora S, Buring JE, Glynn RJ. Blood pressure and risk of developing type 2 diabetes mellitus: the Women’s Health Study. Eur Heart J. 2007;28:2937–2943.
Mullican DR, Lorenzo C, Haffner SM. Is prehypertension a risk factor for the development of type 2 diabetes. Diabetes Care. 2009;32:1870–1872.
Izzo R, de Simone G, Chinali M, Iaccarino G, Trimarco V, Rozza F, et al. Insufficient control of blood pressure and incident diabetes. Diabetes Care. 2009;32:845–850.
Morimoto A, Tatsumi Y, Deura K, Mizuno S, Ohno Y, Miyamatsu N, et al. Impact of impaired insulin secretion and insulin resistance on the incidence of type 2 diabetes mellitus in a Japanese population: the Saku study. Diabetologia. 2013;56:1671–1679.
Tatsumi Y, Morimoto A, Miyamatsu N, Noda M, Ohno Y, Deura K. Effect of body mass index on insulin secretion or sensitivity and diabetes. Am J Prev Med. 2015;48:128–135.
Tatsumi Y, Morimoto A, Soyano F, Shimoda T, Miyamatsu N, Ohno Y, et al. Risk of proteinuria among individuals with persistent borderline diabetes: the Saku study. Diabetol Int. 2016;7:181–187.
Tochikubo O, Nishijima K, Ohshige K, Kimura K. Accuracy and applicability of the Terumo ES-H55 double-cuff sphygmomanometer for hospital use. Blood Press Monit. 2003;8:203–9.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M. et al. Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419.
Kosaka K, Ku-zuya T, Yoshinaga H, Haqura R. A prospective study of health check examinees for the development of non-insulin-dependent diabetes mellitus: relationship of the incidence of diabetes with the initial insulinogenic index and degree of obesity. Diabet Med. 1996;13:S120–S126.
Ministry of Health, Labour and Welfare. http://www1.mhlw.go.jp/topics/kenko21_11/b5.html#A52.
Briasoulis A, Agarwal V, Messerli FH. Alcohol consumption and the risk of hypertension in men and women: a systematic review and meta-analysis. J Clin Hypertens. 2012;14:792–798.
Baliunas DO, Taylor BJ, Irving H, Roerecke M, Patra J, Mohapatra S, et al. Alcohol as a risk factor for type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2009;32:2123–2132.
Huai P, Xun H, Reilly KH, Wang Y, Ma W, Xi B. Physical activity and risk of hypertension: a meta-analysis of prospective cohort studies. Hypertension. 2013;62:1021–1026.
Smith AD, Crippa A, Woodcock J, Brage S. Physical activity and incident type 2 diabetes mellitus: a systematic review and dose-response meta-analysis of prospective cohort studies. Diabetologia. 2016;59:2527–2545.
Decoda Study Group., Nyamdorj R, Qiao Q, Lam TH, Tuomilehto J, Ho SY, et al. BMI compared with central obesity indicators in relation to diabetes and hypertension in Asians. Obesity (Silver Spring). 2008;16:1622–1635.
Bell JA, Kivimaki M, Hamer M. Metabolically healthy obesity and risk of incident type 2 diabetes: a meta-analysis of prospective cohort studies. Obes Rev. 2014;15:504–515.
Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51:1403–19.
Feihl F, Liaudet L, Waeber B, Levy BI. Hypertension: a disease of the microcirculation. Hypertension. 2006;48:1012–1017.
Nguyen TT, Wang JJ, Islam FM, Mitchell P, Tapp RJ, Zimmet PZ, et al. Retinal arteriolar narrowing predicts incidence of diabetes: the Australian Diabetes, Obesity and Lifestyle (AusDiab) Study. Diabetes. 2008;57:536–539.
Serné EH, Stehouwer CD, ter Maaten JC, ter Wee PM, Rauwerda JA, Donker AJ, et al. Microvascular function relates to insulin sensitivity and blood pressure in normal subjects. Circulation. 1999;99:896–902.
Izumi M, Suzuki K, Sakamoto T, Hayashi M. Advantages and limitations of antihypertensive treatment for stroke risk in a general population: the Akita Stroke Registry. Acta Cardiol. 2011;66:729–35.
Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M. et al. Japanese Society of Hypertension Committee. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). Hypertens Res. 2009;32:3–107.
Ogihara T, Nakao K, Fukui T, Fukiyama K, Ueshima K, Oba K. et al. Candesartan Antihypertensive Survival Evaluation in Japan Trial Group. Effects of candesartan compared with amlodipine in hypertensive patients with high cardiovascular risks: candesartan antihypertensive survival evaluation in Japan trial. Hypertension. 2008;51:393–398.
NAVIGATOR Study Group, McMurray JJ, Holman RR, Haffner SM, Bethel MA, Holzhauer B, et al. Effect of valsartan on the incidence of diabetes and cardiovascular events. N Engl J Med. 2010;362:1477–1490.
Ministry of Health, Labour and Welfare. http://www.mhlw.go.jp/seisakunitsuite/bunya/kenkou_iryou/kenkou/kenkounippon21/en/eiyouchousa/kekka_shintai_chousa_nendo.html. Accessed 13 February 2018.
Acknowledgements
We thank all of the researchers and co-workers at Saku Central Hospital for their excellent medical examinations and follow-up surveys.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Tatsumi, Y., Morimoto, A., Asayama, K. et al. Risk of developing type 2 diabetes according to blood pressure levels and presence or absence of hypertensive treatment: the Saku study. Hypertens Res 42, 105–113 (2019). https://doi.org/10.1038/s41440-018-0121-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0121-6