Abstract
Objective
We aimed to compare visual and anatomical outcome in subretinal aflibercept vs. intravitreal aflibercept in the context of Pars Plana Vitrectomy (PPV), pneumatic displacement with subretinal air and subretinal tPA in patients with naïve submacular haemorrhage (SMH) secondary to neovascular age-related macular degeneration (nAMD).
Design
Retrospective interventional cohort study.
Participants
80 patients treated with subretinal aflibercept vs. intravitreal aflibercept in the context of PPV, subretinal air and subretinal tPA in patients with SMH secondary to naïve nAMD.
Methods
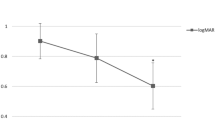
Records were reviewed. Best corrected visual acuity (BCVA), central subfoveal thickness (CST), and intraocular pressure (IOP) were recorded at baseline and 24 months after treatment.
Main outcome measures
BCVA, CST, and number of anti VEGF treatment over follow-up period.
Results
The average duration from onset of symptoms to surgery was 1.26 days (range 0–3 days). Based on review of OCT images, SMH was subretinal in all 80 patients (100%), and sub-RPE in 29 patients (36.3%). Forty-one patients (51.25%) were treated with subretinal aflibercept (“subretinal group”), and 39 patients (48.75%) were treated with intravitreal aflibercept injections (“intravitreal group”). The groups were well balanced for age and gender p = 0.6588, and p = 0.263, respectively). Both groups showed statistically significant improvement in BCVA and CST (for all groups: p < 0.001). The mean number of anti VEGF given during follow-up period was statistically significantly lower in the “subretinal group” (p < 0.0001).
Conclusion
This study shows better management of the CNV, with a statistically significant lower need for anti-VEGF injections when treated with subretinal aflibercept compared to intravitreal application.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Toth CA, Morse LS, Hjelmeland LM, Landers MB. Fibrin directs early retinal damage after experimental subretinal hemorrhage. Arch. Ophthalmol. 1991;109:723-9. https://pubmed.ncbi.nlm.nih.gov/2025175/. Accessed 18 Dec 2021.
Scupola A, Coscas G, Soubrane G, Balestrazzi E. Natural history of macular subretinal hemorrhage in age-related macular degeneration. Ophthalmologica. 1999;213:97–102. https://pubmed.ncbi.nlm.nih.gov/9885385/ Accessed December 18, 2021.
Glatt H, Machemer R. Experimental subretinal hemorrhage in rabbits. Am J Ophthalmol. 1982;94:762–73.
Hanscom TA, Diddie KR. Early surgical drainage of macular subretinal hemorrhage. Arch Ophthalmol. 1987;105:1722–3. Chicago, Ill. 1960.
Vander JF, Federman JL, Greven C, Slusher MM, Gabel VP. Surgical removal of massive subretinal hemorrhage associated with age-related macular degeneration. Ophthalmology. 1991;98:23–27.
Toth CA, Benner JD, Hjelmeland LM, Landers MB 3rd, Morse LS. Ultramicrosurgical removal of subretinal hemorrhage in cats. Am J Ophthalmol. 1992;113:175–82.
Chen CY, Hooper C, Chiu D, Chamberlain M, Karia N, Heriot WJ. Management of submacular hemorrhage with intravitreal injection of tissue plasminogen activator and expansile gas. Retina. 2007;27. https://journals.lww.com/retinajournal/Fulltext/2007/03000/MANAGEMENT_OF_SUBMACULAR_HEMORRHAGE_WITH.7.aspx.
Tsai S-C, Lin J-M, Chen H-Y. Intravitreous recombinant tissue plasminogen activator and gas to treat submacular hemorrhage in age-related macular degeneration. Kaohsiung J Med Sci. 2003;19:608–15. Available at https://doi.org/10.1016/S1607-551X(09)70514-5.
Moriarty AP, McAllister IL, Constable IJ. Initial clinical experience with tissue plasminogen activator (tPA) assisted removal of submacular haemorrhage. Eye. 1995;9:582–8. Available at https://doi.org/10.1038/eye.1995.144.
Kamei M, Tano Y, Maeno T, Ikuno Y, Mitsuda H, Yuasa T. Surgical removal of submacular hemorrhage using tissue plasminogen activator and perfluorocarbon liquid. Am J Ophthalmol. 1996;121:267–75.
Claes C, Zivojnovic R. Efficacy of tissue plasminogen activator (t-PA) in subretinal hemorrhage removal. Bull Soc Belg Ophtalmol. 1996;261:115–8.
Haupert CL, McCuen BW 2nd, Jaffe GJ, Steuer ER, Cox TA, Toth CA, et al. Pars plana vitrectomy, subretinal injection of tissue plasminogen activator, and fluid-gas exchange for displacement of thick submacular hemorrhage in age-related macular degeneration. Am J Ophthalmol. 2001;131:208–15.
Olivier S, Chow DR, Packo KH, MacCumber MW, Awh CC. Subretinal recombinant tissue plasminogen activator injection and pneumatic displacement of thick submacular hemorrhage in age-related macular degeneration. Ophthalmology. 2004;111:1201–8.
Martel JN, Mahmoud TH. Subretinal pneumatic displacement of subretinal hemorrhage. JAMA Ophthalmol. 2013;131:1632–5.
Kadonosono K, Arakawa A, Yamane S, Inoue M, Yamakawa T, Uchio E, et al. Displacement of submacular hemorrhages in age-related macular degeneration with subretinal tissue plasminogen activator and air. Ophthalmology. 2015;122:123–8.
Chang W, Garg SJ, Maturi R, Hsu J, Sivalingam A, Gupta SA, et al. Management of thick submacular hemorrhage with subretinal tissue plasminogen activator and pneumatic displacement for age-related macular degeneration. Am J Ophthalmol. 2014;157:1250–7.
Stopa M, Lincoff A, Lincoff H. Analysis of forces acting upon submacular hemorrhage in pneumatic displacement. Retina. 2007;27:370–4.
Treumer F, Roider J, Hillenkamp J. Long-term outcome of subretinal coapplication of rtPA and bevacizumab followed by repeated intravitreal anti-VEGF injections for neovascular AMD with submacular haemorrhage. Br J Ophthalmol. 2012;96:708–13. https://pubmed.ncbi.nlm.nih.gov/22174095/ Accessed December 18, 2021.
Avcı R, Yıldız AM, Çınar E, Yılmaz S, Küçükerdönmez C, Akalp FD. et al. Subretinal coapplication of tissue plasminogen activator and bevacizumab with concurrent pneumatic displacement for submacular hemorrhages secondary to neovascular age-related macular degeneration. Turk J Ophthalmol.2021;51:38 https://pmc/articles/PMC7931654/. Accessed 18 Dec 2021.
Matsuoka M, Ogata N, Otsuji T, Nishimura T, Takahashi K, Matsumura M. Expression of pigment epithelium-derived factor and vascular endothelial growth factor in choroidal neovascular membranes and polypoidal choroidal vasculopathy. Br J Ophthalmol. 2004;88:809–15.
Lüke M, Januschowski K, Warga M, Beutel J, Leitritz M, Gelisken F, et al. The retinal tolerance to bevacizumab in co-application with a recombinant tissue plasminogen activator. Br J Ophthalmol. 2007;91:1077–82. https://bjo.bmj.com/content/91/8/1077 Accessed December 18, 2021.
Klettner A, Grotelüschen S, Treumer F, Roider J, Hillenkamp J. Compatibility of recombinant tissue plasminogen activator (rtPA) and aflibercept or ranibizumab coapplied for neovascular age-related macular degeneration with submacular haemorrhage. Br J Ophthalmol. 2015;99:864–9.
Jackson TL, Bunce C, Desai R, Hillenkamp J, Lee CN, Lois N, et al. Vitrectomy, subretinal tissue plasminogen activator and Intravitreal Gas for submacular haemorrhage secondary to Exudative Age-Related macular degeneration (TIGER): study protocol for a phase 3, pan-European, two-group, non-commercial, active-control, observer-masked, superiority, randomised controlled surgical trial. Trials. 2022;23:99.
Gros-Otero J, Benítez-Herreros J, Beckford-Torngren C, Cámara-González C, Castro-Rebollo M.Management of subretinal hemorrhage with r-TPA, SF-6 and ranibizumab.Arch Soc Esp Oftalmol.2010;85:114–7.
Chalam KV, Gasparian S. Successful delivery of subretinal aflibercept (new surgical technique) for the treatment of submacular hemorrhage in idiopathic polypoidal choroidal vasculopathy. J. Surg. Case Rep. 2021; 2021. https://pubmed.ncbi.nlm.nih.gov/34408845/ Accessed 9 Jul 2022.
Broadhead GK, Keenan TDL, Chew EY, Wiley HE, Cukras CA.Comparison of agents using higher dose anti-VEGF therapy for treatment-resistant neovascular age-related macular degeneration.Graefe’s Arch. Clin. Exp. Ophthalmol.2022;260:2239–47.
Sharma S, Kumar JB, Kim JE, Thordsen J, Dayani P, Ober M, et al. Pneumatic displacement of submacular hemorrhage with subretinal air and tissue plasminogen activator: initial united states experience. Ophthalmol Retin. 2018;2:180–6. Available at https://doi.org/10.1016/j.oret.2017.07.012.
Sacu S, Stifter E, Vécsei-Marlovits PV, Michels S, Schütze C, Prünte C, et al. Management of extensive subfoveal haemorrhage secondary to neovascular age-related macular degeneration. Eye. 2009;23:1404–10.
de Silva SR, Bindra MS. Early treatment of acute submacular haemorrhage secondary to wet AMD using intravitreal tissue plasminogen activator, C3F8, and an anti-VEGF agent. Eye. 2016;30:952–7.
Meyer CH, Scholl HP, Eter N, Helb H-M, Holz FG. Combined treatment of acute subretinal haemorrhages with intravitreal recombined tissue plasminogen activator, expansile gas and bevacizumab: a retrospective pilot study. Acta Ophthalmol. 2008;86:490–4.
Iglicki M, Busch C, Lanzetta P, Sarao V, Veritti D, Rassu N, et al. Vitrectomized vs non-vitrectomized eyes in DEX implant treatment for DMO-Is there any difference? the VITDEX study. Eye (Lond). 2022. https://doi.org/10.1038/s41433-022-01931-9. [Epub ahead of print].
Avery RL, Fekrat S, Hawkins BS, Bressler NM. Natural history of subfoveal subretinal hemorrhage in age-related macular degeneration. Retina. 1996;16:183–9.
Acknowledgements
Javier Ignacio Melamud MD. Head of external Emergency room at the Medical intitute of investigation “ Alfredo Lanari “, University of Buenos Aires. General pactitiones and Legal medical specialst, Univesity of Buenos Aires, Argentina. Marina Koury MD. consultant in methodology, epidemiologic, and research from the teaching and investigation department at medical institute of investigation “Alfredo Lanari“, Univestity of Buenos Aires, Argentina.
Author information
Authors and Affiliations
Contributions
MI, DJQ, MK—Substantial contributions to the conception or design of the work; the acquisition, analysis, and interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published; ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. JIM, LD, AB, AL, DZ—Substantial contributions to the conception or design of the work and interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published; ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submit- ted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethics
As this was a retrospective study, participants’ informed consent was not needed, in compliance with the Institutional review board (IRB) approval. This study protocol was reviewed and approved by the local IRB. The research adhered to the tenets of the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Iglicki, M., Khoury, M., Melamud, J.I. et al. Naïve subretinal haemorrhage due to neovascular age-related macular degeneration. pneumatic displacement, subretinal air, and tissue plasminogen activator: subretinal vs intravitreal aflibercept-the native study. Eye 37, 1659–1664 (2023). https://doi.org/10.1038/s41433-022-02222-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02222-z
This article is cited by
-
Comparison of subretinal aflibercept vs ranibizumab vs bevacizumab in the context of PPV, pneumatic displacement with subretinal air and subretinal tPA in naïve submacular haemorrhage secondary to nAMD. “The Submarine Study”
Eye (2024)
-
Accuracy of biomicroscopy, ultrasonography and spectral-domain OCT in detection of complete posterior vitreous detachment
BMC Ophthalmology (2023)
-
Vitreoretinale Chirurgie bei altersabhängiger Makuladegeneration
Die Ophthalmologie (2023)