Abstract
Background
Idiopathic scleroma (previously coined solitary idiopathic choroiditis or focal scleral nodule) is an innocuous lesion affecting the sclera with intraocular manifestations. It is often the basis of many misdiagnoses such as amelanotic choroidal melanoma, osteoma or metastatic lesions. Patients are often asymptomatic and the course is benign. With increasing use of community based imaging, more of such cases are being identified. This paper is a retrospective case series investigating the multi-modal imaging findings of idiopathic scleroma.
Methods
A retrospective analysis of prospectively collected data were analysed. Over the course of January 2008–January 2022, 44 patients diagnosed with idiopathic scleroma and imaged with wide-field colour fundus photography, fundus autofluorescence, ocular coherence tomography (OCT) and B-scan ultrasonography. Due to a poor image, only 43 images were included for OCT review. We also reviewed our patient’s demographics, symptoms and baseline ophthalmic characteristics upon presentation.
Results
The mean age was 52 years (range 32–79) and there was no predilection towards gender. All lesions were post equatorial with the most common location being inferotemporal (n = 16, 36%); 32 lesions (73%) were yellow on fundus photography. 82% (n = 36/44) of lesions exhibited hyperautoflourescence and 43 lesions (98%) showed hyperechogenicity on B-scan ultrasonography. 100% of lesions originated from the sclera with no lesions showing active inflammation. 20 (47%) lesions had associated blood vessels overlying them on OCT.
Discussion
Idiopathic scleroma is a yellow, hyperautofluorescent, hyperechogeneic scleral lesion that has no signs of active inflammation. These characteristics help define them from other more sinister cause of amelanotic fundal lesions.
Similar content being viewed by others
Introduction
In 1997, a unifocal, yellow-white granuloma-like mass was first described by Hong et al. in six patients using fundus photography. This atypical mass was initially termed “unifocal helioid choroiditis” due to its sun like appearance [1]. Shields et al. subsequently renamed the lesion as a ‘solitary idiopathic choroiditis’ (SIC) based on their findings of a solitary choroidal mass associated with features of inflammation, including subretinal fluid (SRF) and leakage on fluorescein angiography (FA) [2]. Fung et al. noted that these lesions demonstrated focal scleral thickening with associated overlying choroidal thinning [3, 4]. It was therefore recommended that clinicians refer to this condition as “Focal Scleral Nodule’. Similar findings were demonstrated by Duignan et al., who also identified a non-inflammatory lesion clearly arising from the sclera but rather suggested a nomenclature change to ‘Idiopathic Scleroma’ [5].
Progression in ocular imaging in oncology settings, most notably the use of Ocular Coherence Tomography (OCT) in particular, enhanced depth imaging OCT (EDI-OCT), has recently resulted in a shift of our understanding and awareness of this condition leading to higher rates of diagnosis of this lesion. Since the beginning of 2020, our tertiary eye unit at Liverpool Ocular Oncology Centre (LOOC) has diagnosed 20 patients with this lesion despite only diagnosing 24 patients with this lesion since the first diagnosis in 2008. Despite this, there remains a scarcity of research defining the imaging characteristics of this lesion.
This retrospective series, the largest in Europe to date, aims to assess multi-modal imaging findings of patients who have been diagnosed with the condition now labelled as idiopathic scleroma. We aim to provide further insight into imaging characteristics of this condition and review if patients diagnosed within our tertiary ocular oncology centre share characteristics to the aforementioned.
Methods
A retrospective review was performed on all patients who had been diagnosed with scleroma at LOOC, between Jan 2008 and Jan 2022. Patient’s demographics and baseline ophthalmic assessment including presence or absence of symptoms and visual acuity were obtained from electronic patient records. All patients referred for assessment at LOOC undergo routine ophthalmic examination, including EDI-OCT imaging, wide-field imaging and Ultrasound assessment. OCT was performed by a Spectralis OCT (Heidelberg Engineering, Heidelberg, Germany) with 19-line volume scan with a setting of 9 ART (automatic real time) over the lesion and fovea. The wide-field imaging was a 200-degree colour photo and autofluorescence obtained from an Optos California (Optos, Dunfermline, Scotland).
Risk assessment for systemic disease known to be associated with choroiditis was discussed during the clinical assessment, including Mycobacterium Tuberculosis, Toxoplasmosis and Sarcoidosis. Serological testing was not performed unless clinically indicated.
Evaluation of Optos wide-field imaging included lesion borders and regularity, colour, autofluorescence, orange pigment and drusen were noted, alongside the location of the lesion relative to the optic disc. Further measurements on Optos imaging included maximal transverse diameter, maximal longitudinal diameter, distance to the fovea and distance to the optic disc. B-scan ultrasound assessment included echogenicity of the lesion, presence of acoustic shadow and lesion thickness.
EDI-OCT images were analysed at the apex of the lesion and the margin of the lesion and the lesion’s thickness and diameter were also measured. Thickness was measured from the apex of the lesion to the visualised posterior margin with the apex being defined as the highest point of elevation of the scleroma as located on the EDI-OCT. The lesion was categorised based on its shape (dome or volcanic). An independent ophthalmologist also assessed all layers of the overlying neurosensory retina, retinal pigment epithelium (RPE), choroid and sclera, including presence of retinal fluid and hyper/hypo-reflective deposits. Association with overlying blood vessels was also commented on. All images were reviewed by an independent ophthalmologist sub-specialising in Ocular Oncology, and uncertainties were referred to a second independent ophthalmologist, also an Ocular Oncology specialist.
OCT angiography and FA were not routinely performed in assessment of such patients and were therefore not included. Typically, patients diagnosed with scleroma are discharged to their local hospital for follow up—it was therefore not reasonable to include follow up data within this assessment.
Informed patient consent was obtained for image use, data collection and analysis. Ethics committee approval was not required for this retrospective data analysis. The study adheres to the tenants of the Declaration of Helsinki.
Results
Demographics
A total of 44 eyes from 44 patients diagnosed with idiopathic scleroma were included in the study. The lesions were uniquely noted in Caucasians with the mean age of diagnosis being 52, with no discernible difference in gender. Although the majority of patients were asymptomatic, a small proportion were symptomatic with photopsia (n = 5/44, 11%), floaters (n = 1/44, 2%) and blurred vision (n = 2/44, 5%). One patient had a history of previous childhood squint surgery, another had amblyopia and two patients had a choroidal naevus in the affected eye whereas the rest had no known significant past ophthalmic history. Table 1 summarises patient characteristics upon diagnosis.
Tumour features on clinical examination & colour imaging
Idiopathic scleroma tends to be a yellow (n = 32/44, 73%), well defined lesion (n = 25/44, 57%) located post-equatorially (n = 44/44, 100%) along the inferotemporal (n = 16/44, 36%) aspect of the posterior pole. Scleroma lesions do not typically demonstrate orange pigment (n = 4/44, 9%) or drusen (n = 2/44, 5%). Mean dimensions were 2.8 mm (longitudinal) × 2.7 mm (90 degrees perpendicular to this). These findings were obtained from clinical examination, and measurements were obtained from wide-field Optos colour photos. Clinical features on examination are summarised in Table 2.
Appearance on Imaging
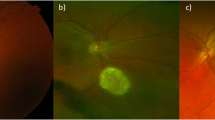
On autofluorescence imaging, the majority of lesions were either hyper-autofluorescent (n = 36/44, 81.8%) or iso-autofluorescent (n = 6/44, 13.6%) in the centre. The remaining two lesions were hypo-autofluorescent (4.5%). At the lesion margin, the majority of lesions were iso-autofluorescent (n = 23/44, 52.3%) or hyper-autofluorescent (n = 18/44, 40.9%). The other three lesions were hypo-autofluorescent (6.8%). Typical imaging features of a scleroma can be seen in Fig. 1.
B-scan ultrasonography (n = 44) demonstrated a mean lesion thickness of 1.06 mm (median = 1.05, range 0.22–1.72). 43 lesions demonstrated hyper-echogenicity (97.7%). Six lesions (n = 6/44, 13.6%) demonstrated notable acoustic shadowing.
OCT was performed on all 44 patients. In one case, the quality of the OCT scan was not appropriate for assessment. Table 3 summarises OCT features of the lesion at the apex (n = 43).
On OCT analysis of our 43 images, the mean diameter was 3.25 mm and the mean thickness was 0.80 mm. Overall, 76.7% (n = 33/43) of images exhibited a dome shaped lesion and 23.3% (n = 10/44) exhibited a volcanic shaped lesion, as seen in Fig. 2. In addition, we identified that 100% of lesions (n = 43/43) arose from the sclera. None of the 43 (n = 0/43, 0%) images analysed by EDI-OCT had an epiretinal membrane (ERM) whilst the majority of the outer retina layers were normal including the nerve fibre layer (NFL) (n = 30/43, 69.8%), the ganglion cell layer (GCL) (n = 38/43, 88.4%), the inner plexiform layer (IPL) (n = 39/43, 90.7%), the inner nuclear layer (INL) (n = 36/43, 83.7%) and the outer plexiform layer (OPL) (n = 35/43, 81.4%). The outer nuclear layer (ONL) was normal in 30 of our patients (n = 30/43) 69.8%), however in 11 patients (25.6%) this layer was thinned whilst the external limiting membrane (ELM) (n = 31/43, 72.1%) was also largely normal. Of the inner layers of the retina, the inner photoreceptor segment (IPS) (n = 22/43, 51.2%) and the outer photoreceptor segment (OPS) (n = 17/43, 39.5%) in our study were largely unaffected, however there was a significant proportion of patients with an absent OPS (n = 15/43, 34.9%). This is in contrast to the RPE where, although nearly fifty percent of patients exhibited a normal RPE (n = 19/43, 44.2%), 10 patients (23.3%) patients had a thinned RPE whilst 13 of 43 patients (23%) had a thickened layer. In our analysis, the choroid exhibited the most pronounced change of all the layers with only one patient (2%) having a normal choroid whilst the majority had a thinned choroid (n = 24, 55.8%) with 16 (n = 16/43, 37.2%) having an absent choroid. Of our 43 patients, it also was found on OCT that 20 of the lesions (n = 20/43, 46.5%) had overlying blood vessels, thought to be retinal vasculature rather than choroidal vasculature. In addition, 14 patients (n = 25/43, 58.1%) exhibited an irregular RPE configuration whilst eight patients exhibited overlying drusen (19%) and four patients had SRF associated with the lesion (9%). Two of the lesions (4.7%) we analysed demonstrated intraretinal fluid. Of the four patients who had associated SRF, three had a thinned or absent choroid whilst one of the patients had a thickened choroid.
Discussion
Idiopathic scleroma comprise of a group of relatively small, benign, non-pigmented fundus lesions of unknown aetiology. They typically occur near the posterior pole in Caucasians in their fifth decade. There seems to be an increase in the number of referrals of these lesions to specialised centres and certainly more published literature on this topic. This could either be caused by an increase in the incidence or an increased use of retinal imaging in the community, which will lead to an increase in the number of previously undetected lesions. The clinical importance of establishing the correct diagnosis through a variety of imaging techniques lies in differentiating it from other potentially malignant small non-pigmented subretinal lesions with a similar clinical presentation, i.e. non-pigmented choroidal melanoma and choroidal metastasis.
This study performed at LOOC is the largest current European study evaluating the multi-modal imaging characteristics of this lesion and provides some insight for researchers and clinicians about this newly described lesion.
Main findings and comparison with previous literature
Our study of 44 patients found that the demographics of individuals diagnosed with this lesion were consistent with previous reports [3, 4]; patients were generally asymptomatic and generally had no past ophthalmic or retinal history. There was no predilection towards gender, all of our patients were Caucasians, the age at presentation ranged from 32 to 79 years.
Also consistent with previous publications were our findings on fundus photography and FAF. We found that the lesions were well-defined, hyperautofluorescent lesions measuring on average 2.8 × 2.7 mm with the majority of lesions occurring inferotemporally to the optic disc. In addition, the majority of our lesions were yellow (n = 32) which appears similar to the yellow-white lesions seen in previous publications [3, 4, 6, 7]. Despite this, the variations in the colours seen on optos are likely due to varying degrees of RPE atrophy and choroidal thinning as a result of compression from the lesion.
Results in the literature regarding the nature of autofluorescence with SIC lesions is variable [2, 4]; we found that 81.8% of our lesions were hyperautofluorescent with 93% of lesions having with a thinned or absent choroid. Our results align with evidence from previous publications stating that SIC/scleroma lesions are primarily hyperautofluorescent which one paper postulating that this could be due to scleral unmasking as a result of thinning of the overlying choroid and subsequent impedance of choroidal blood flow to overlying layers [3]. The more choroidal thinning there is, the higher the levels of autofluorescence. Another theory is that the hyperautofluorescence is due to lipofuscin accumulation in diseased RPE.
However, we found that 8 lesions (18%) were either iso or hypoautofluorescent. This has been postulated to be caused by complete choroidal thinning with varying degrees of disruption to choroidal blood flow [2]. We also found that a significant number (n = 20/43, 46.5%) had overlying retinal blood vessels, something that has not been noted by previous publications. Previous publications have, however, noticed clear choroidal flow voids overlying the lesion something that is in-keeping with choroidal compression from the underlying scleral lesion. This being said, we do not routinely perform angiography on our patients in clinic and we are unable to comment further on the significance of overlying blood vessels.
Due to the advent of more novel imaging techniques, more recent publications have shown that scleroma/SIC lesions seem to originate from the sclera, rather than being choroidal in nature as early publications on this lesion indicated. Fung et al., utilised swept source OCT to fully delineate the location of the posterior margin of these lesions stating these lesions were scleral in nature, something that was reaffirmed by Duignan et al., despite the latter not utilising swept source OCT. Our paper found that all lesions were scleral in origin with varying degrees of choroid compression (93% had absent or thinned choroid). Duignan et al., also found that 100% of lesions were scleral in nature. We also found that the RPE varied in its presentation with 57% being regular and 43% being irregular. Despite only finding two patients with drusen on fundus photography, we found that 8 patients had drusen on EDI-OCT which may contribute to the irregularity of the RPE. We believe this to be a concomitant finding and not related to the lesion.
Before the advent of detailed imaging, it was postulated that these lesions had two phases, an active phase whereby the lesion was ill-defined with signs of inflammation such as SRF and retinal haemorrhages and an inactive phase with a well-defined margin lacking signs of inflammation [2, 7]. Shields found that ~30% of their patients had inflammatory signs, however this study was prior to the advent of OCT [3]. Fung et al. [4], found that their lesions were not associated with any signs of active inflammation such as choroidal thickening, leakage on angiography, vitritis or any signs of systemic inflammation and this bought about a nomenclature change from SIC to focal scleral nodule, based also on the fact that the lesion appears to originate from the sclera, not the choroid. This being said, they did find 9 patients with SRF, a known but not exclusive sign of inflammation and they did not comment upon the regularity of the lesion on fundoscopy. An image of a scleroma with SRF can be seen in Fig. 2.
As with previous publications including Fung et al., we also found that our lesions lacked many of the signs of choroiditis such as retinal vascular dilation or any systemic symptoms on examination. However, 19 (n = 19/44, 43.2%) of our lesions had an ill-defined margin on fundoscopy and four (n = 4/44, 9.1%) presented with SRF despite only two (n = 2/44, 4.5%) having intraretinal fluid. It has been suggested that, although there may be an inflammatory process which occurs to produce the lesions, when these lesions become clinically apparent, they appear inactive [4].The presence of SRF in the absence of inflammatory signs has been thought to be due to RPE thinning which disrupts the pumping ability of the RPE allowing fluid to accumulate, rather than an inflammatory process, particularly in the absence of any other signs of inflammation. It must also be noted that only two of the four patients who presented with SRF had concurrent thinned RPEs and one patient had a thickened RPE. Our study findings align with this concept and show that this lesion is not associated with active inflammation.
Furthermore, it was interesting to note that 8 of our patients were symptomatic upon presentation to our clinic, a similar number found compared to previous publications. Only one of the symptomatic patients, who presented with floaters, had SRF which could contribute towards visual disturbance. It was also found that the location of the lesion of another symptomatic patient was overlying the optic disc suggesting that the location and the presence of associated features can both contribute to the clinical presentation of a patient. It must be highlighted though that both our results and the literature find that most patients with this condition are asymptomatic. None of the symptomatic patients in our cohort were treated.
Clinical implications
More clinically relevant, the multi-modal imaging techniques of this lesion are able to differentiate idiopathic scleroma from more sight and even life-threatening lesions such as choroidal melanoma and choroidal metastases. Idiopathic scleroma is scleral in origin and exhibits intrinsic autofluorescence whilst melanoma and metastases are choroidal in origin and lack autofluorescence (although associated lipofuscin and exudation may give rise to hyperfluorescence. Amelanotic choroidal melanomas tend to have more irregular borders, exhibit more lipofuscin and angiogenesis than idiopathic scleromas. Metastases tend to be duller in their colour are associated with another primary. Idiopathic scleromas are stable over time in their appearance whilst the aforementioned conditions are progressive in nature. The hardest to differentiate lesion to a scleroma is certainly sclerochoroidal calcification as they share many similar imaging features such as hyperreflectivity on US. However, schlerochoroidal calcification is echodense in nature finding due to the calcium deposits and it is frequently seen with metabolite abnormalities in biochemical investigations. Subsequently, this makes it an important differential to exclude.
Strength and weaknesses
The main strength of this study was the cohort size; 44 patients is currently the largest cohort in Europe and we performed a wide variety of imaging techniques. There are a few limitations to this study. Unlike previous publications, we were unable to analyse any lesions with swept-source OCT which has been shown to be more detailed and more sensitive. Our clinic does not routinely perform FA, indocyanine green angiography or infra-red reflectance on these lesions, so we are unable to fully elucidate these characteristics, particularly the associated inflammatory signs. Our clinic, as aforementioned, does not routinely follow up patients with a diagnosis of scleroma so we are unable to comment upon how these lesions progress in the long term. We also did not treat any of our cohort who were symptomatic from their lesion. However, it has been published that idiopathic scleroma is stable in nature [1]; generally, if patients discharged from LOOC require further input they are likely re-referred to us later down the line. In fact, the biggest limitation to this study, as with previous studies, is the inability to fully comment upon the aetiology of this lesion due to the lack of histopathological analysis. Currently, there is no treatment required for this lesion so barring a concomitant pathology which requires globe removal, histopathological investigation of this lesion remains a key barrier to truly understanding the aetiology and origin of this lesion.
Conclusion
In conclusion, our study aligns with the current literature published on this lesion. We found that idiopathic scleroma is a hyperautofluorescent lesion which originates from the sclera and lacks features of active inflammation. We described a lesion with distinct differences to other, more serious, choroidal conditions and how clinicians can utilise simple OCT imaging to differentiate scleroma from said lesions. Future research needs to focus on more widespread use of swept source OCT and OCT angiography to fully delineate the characteristics of this lesion whilst finding ways to analyse the lesion histopathologically.
Summary
What was known before
-
Idiopathic scleroma (previously coined solitary idiopathic choroiditis or focal scleral nodule) is an innocuous lesion affecting the sclera with intraocular manifestations. It is often the basis of many misdiagnoses such as amelanotic choroidal melanoma, osteoma or metastatic lesions.
What this study adds
-
Idiopathic scleroma is a yellow, hyperautofluorescent, hyperechogeneic scleral lesion that has no signs of active inflammation. These characteristics help define them from other more sinister cause of amelanotic fundal lesions.
Data availability
Data utilised for this study is stored on a secure database accessible to treating physicians within the ocular oncology unit in Liverpool. Raw anonymised data are available on request data utilised for this study is stored on a secured database accessible to treating physicians within the ocular oncology unit in Liverpool. Raw anonymised data are available on request.
References
Hong PH, Jampol LM, Dodwell DG, Hrisomalos NF, Lyon AT. Unifocal Helioid Choroiditis. Arch Ophthalmol. 1997;115:1007–13. https://doi.org/10.1001/archopht.1997.01100160177006.
Shields JA, Shields CL, Demirci H, Hanovar S. Solitary Idiopathic Choroiditis. Arch Ophthalmol. 2002;120:311–9. https://doi.org/10.1001/archopht.120.3.311.
Fung AT, Kaliki S, Shields CL, Mashayekhi A, Shields JA. Solitary Idiopathic Choroiditis. Ophthalmology. 2013;120:852–8. https://doi.org/10.1016/j.ophtha.2012.09.017.
Fung AT, Waldstein SM, Gal-Or O, Pellegrini M, Preziosa C, Shields JA, et al. Focal Scleral Nodule. Ophthalmology. 2020;127:1567–77. https://doi.org/10.1016/j.ophtha.2020.04.018.
Duignan E, O’Day R, Moloney T, Rahman W, Damato B. A Case Series of “Solitary Idiopathic Choroiditis” and Proposal of a Nomenclature Change to “Idiopathic Scleroma.”. Ocul Oncol Pathol. 2020;7:48–6. https://doi.org/10.1159/000509942. Published online November 10.
Delich CB, Shields CL. Ocular oncology case study CASE PRESENTATION. Retina Today. April 2009. p. 84.
Kohne KD, Malinovsky VE, Gao H. Solitary idiopathic choroiditis. Optometry 2007;78:176–80. https://doi.org/10.1016/j.optm.2006.10.018.
Acknowledgements
The authors would like to acknowledge everyone involved in the care of patients at LOOC, including medical photography for their reliable and professional images.
Author information
Authors and Affiliations
Contributions
JP–Primary corresponding author involved with leading all aspects of the publication from data collection to paper writing. HS–Mr HS was involved heavily with data collection and image interpretation being a driving force for the results section. Mr HS also provided invaluable advice during the manuscript writing. AD–Mr AD was also involved with data collection and image interpretation, providing much valued insight into the results section. RH–Ms RH provided invaluable support and advice throughout the entire publication, most noticeably aiding with the paper writing. Ms RH also acted as the independent ophthalmologist if there were any queries with our images. HH–Professor HH was involved in helping with the paper writing and was a valuable source of advice throughout the writing of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pearman, J., Shah, H., Diafas, A. et al. Imaging characteristics of idiopathic scleroma: a retrospective case series and review of the literature. Eye 37, 1026–1032 (2023). https://doi.org/10.1038/s41433-022-02161-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02161-9