Abstract
Background/objectives
Strabismus surgery training has historically focussed on the “see one, do one and teach one” approach. Simulation training offers an alternative to practice surgical skills without direct patient involvement. However, current simulation models for strabismus surgery are limited due to concerns regarding use of animal or human tissue and financial cost limiting practice. Our aim was to build and validate a low-cost model for obtaining the core skills required in strabismus surgery.
Subjects/methods
A low-cost strabismus model was developed using commercially available materials. Ophthalmic trainees, fellows and consultants were surveyed using a questionnaire to assess the realism and training utility of the model using a five-point Likert scale (1 = unacceptable, 2 = poor, 3 = acceptable, 4 = favourable and 5 = excellent) whilst simulating a horizontal muscle resection task.
Results
Forty-two ophthalmologists completed the questionnaire. The model scored highly for muscle securing and suturing (median: 4.00) and suturing. Muscle dissection and conjunctiva were considered poor (median: 3.00, 2.50, respectively). Overall, participants felt that the model simulated strabismus surgery well (median: 4.00) and was comparable to other dry simulation models (median: 4.00).
Conclusion
Our study describes a favourable training model that can be used for independent practice of core strabismus surgical techniques. However, it remains a technical challenge to replicate certain ocular anatomy using commercially available materials.
Similar content being viewed by others
Introduction
Ophthalmic surgical training programmes aim to develop trainees’ level of proficiency within the various subspecialties of ophthalmic surgery. These include extraocular muscle surgery, primarily for strabismus correction, but also as part of enucleation, retinal detachment and repair of globe trauma. The ophthalmic speciality training curriculum in the United Kingdom requires trainees to have completed 20 surgical strabismus procedures by time of completion of training [1]. Of these five may be simulated as long as they are observed.
Surgical training has evolved within the last few decades from the traditional Halstead's approach; “see one, do one and teach one” [2], to a competency-based framework [3] in recognition of the learning curve of skills acquisition. However, acquiring the required competencies within the postgraduate training programme remains a challenge. This is due to legislative and regulatory contractual changes in favour of minimising fatigue and improving patient care [4]. Perhaps reflected in current training, there is a declining trend in speciality surgical experience at time of completion of training [5].
The challenge of any learning curve is to allow development of skills during the novice phase, which is prone to greater risks, without compromising outcome, e.g., inadvertently perforating the globe in cases of strabismus surgery. There is sparsity of published data on the strabismus surgery learning curve. Kim et al. report that 20–40 cases are required to obtain efficiency and proficiency of performing horizontal single muscle surgery [6], however, this is related to the learning curve of an established ophthalmic surgeon that has acquired technical skills in ophthalmic surgery. This is further compounded by the emotional state of the trainee; one survey of ophthalmology residents found poor recall of learning due to anxiety from conventional operative strabismus surgery teaching experience, which resulted in a negative performance (24% reporting tremor, 11% had tachycardia, 10% moments of absence and 34% felt nervous) [7].
Simulation training has shown promise in technical and non-technical skills training [8,9,10,11] to bridge the learning curve. Selvander et al. have shown improved performance on tissue treatment, efficiency, microscope and instrument handling following virtual reality capsulorhexis training. In particular, a subgroup of medical students underwent previous virtual reality navigation training and was found to have consistent overall higher scores and shorter learning curves for capsulorhexis performance on the simulator. Furthermore, Belyea et al. assessed 592 consecutive phacoemulsification in 42 residents of which half underwent simulation training. They reported significant improvement in time, intraoperative complication rate and amount of power used by phacoemulsification in residents that had underwent previous cataract virtual reality simulation training [11].
Despite the proven benefits, very few simulation models have been formally validated in ophthalmology [12]. Current high-fidelity simulation training in strabismus surgery is available with the use of cadaveric tissue (human, rabbits or porcine) [13]. However, this is expensive, provides single on-off simulation experience or requires specialist licencing for training. This is not ideal, as it creates an elite model for training limited to centres that can provide the necessary resources.
Aim
Our aim was to develop and validate an alternative simulation model using low-cost materials to allow practice of basic surgical skills required for strabismus surgery.
Method
Low-cost strabismus model
Preparation
Various commercially available craft materials (silicone and rubber) were tried and tested by the authors. The following materials (Table 1) were considered to provide the adequate feel of the ocular tissue being simulated.
Foam will provide a base to practice scleral suturing. For the model, we advise cutting out two strips of foam measuring 7 cm (length) × 1.5 cm (width) × 0.5 mm (thickness) foam. Furthermore, divide one of the strips in half. Next for muscle, we found felt to be a realistic material as it is easily friable if not handled correctly. To prepare, we advise cutting out four strips of felt 10 cm (length) × 1 cm (width) × 0.5 mm (thickness).
Construction of low-cost strabismus model
An instructional video on the construction of this model has been made freely available on social media platform, YouTube [14] (see Fig. 1).
Full guide on making the model can be found on the following link: https://www.youtube.com/watch?v=PHGZnPZDdEY or by searching “Jain Eye model” on YouTube. Assembly. Step 1: fix a pin to base of the table tennis ball using hot glue, this enables the base of the model to stay stable during practice on a work (cork) board. Step 2: fix the strips of foam onto the table tennis ball forming a cross on the marked centre of the table tennis ball using hot glue. Step 3: mark centre of the cross with a pen or “googly eye” to form a reference point for the cornea. Step 4: measure 6 mm from the limbus, and mark the foam. This can be varied to replicate anatomically correct distances. Step 5: apply thin strip of glue to the tip of each felt strip, then attach these to the areas marked in step 4. Step 6: fix the tail end of the felt strips to the work (cork) board using pins.
Survey design
Previously validated questionnaire design assessing face, content validation of simulation training model [15] was modified to assess the utility of the proposed strabismus model (Appendix 1). Questionnaires were distributed at a regional and international strabismus workshop to assess face, content validation and utility of the eye model. Whilst simulating horizontal muscle recession, we asked our participants (speciality trainee year (ST): 3–7, fellows and consultants) to rate the following items using a five-point Likert scale; 1 being poor agreeability and 5 scoring highly favourable opinion. All participants surveyed agreed to take part in the study through informed consent.
Face validity measures the resemblance of the simulation to real life surgical procedure. We performed this by assessing the feedback from our participants on the realism of the tissue simulated by the model, in particular focussing on conjunctiva, muscle, sclera and overall experience.
Content validity assesses a specific skill being developed during the simulation. This is in contrast to construct validation, which tests the ability of a simulation to distinguish between skill levels, e.g., novice versus expert. We surveyed our participants on their beliefs of how useful the model was in teaching specific aspects of strabismus surgery; muscle dissection, securing muscle, suturing muscle, developing hand–eye coordination and maintaining hand–eye coordination.
We further assessed the utility of the model based on cost and experience, and its comparison with other dry and wet simulation models.
Statistical analysis was performed on SPSS version 23. A score of 3.3 for a given domain was considered to be adequate. Scores >3.5 were considered favourable and <3.0 were considered inadequate, based on previous studies on face and content validation [9].
Results
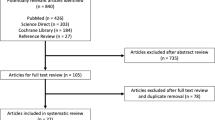
We had a total of 26 participants from the regional workshop across different grades: junior trainee (ST: 3–4, n = 8) median of 13 surgical strabismus cases performed (range: 1–25), senior trainee (ST: 5–7, n = 15) median of 24 (range: 17–30) and expert (consultant, n = 3) with over 75 cases performed. In addition, we had 16 residents from the International workshop in Nairobi, Kenya with variable levels of training (ST1—consultant), that had performed median 0 cases (range: 0–2).
Face validity
Overall, our participants reported that the model replicated the eye accurately for training (median: 4.00, IQR: 0.75), in particular for simulated strabismus surgery (mean: 4.00, IQR: 2.00) (Fig. 2).
Suturing and securing muscles felt realistic and both scored highly (medians: 4.00, IQR: 0.75 and 4.00, IQR: 1.00, respectively). The feel of muscle dissection was considered to be adequately simulated (median: 3.00, IQR: 1.00).
With regards to the feel of the tissue; sclera was considered to feel the most realistic (median: 4.00, IQR: 0.75), whilst muscle felt adequate with the given material (median: 3.00, IQR: 1.00). Conjunctiva on the other hand was considered inadequate (median: 2.50, IQR: 1.00).
Content validity
Participants reported the model to be adequate for training in muscle identification (median: 3.00, IQR: 1.00) (Fig. 3). Moreover, the model was reported as more useful for practicing securing and suturing muscle (median: 4.00, IQR: 1.00).
It was considered an excellent model for developing and maintaining skills in strabismus surgery (median: 4.00, IQR: 0.75 and 4.00, IQR: 1.00).
Utility
Respondents were favourable in recommending the model for training (median: 4.00, IQR: 1.00), particularly due to the low cost and realism offered (median: 4.00, IQR: 1.00).
Twenty-four out of the 42 participants have had prior experience with simulation models for strabismus surgery. Participants reported that our low-cost model was comparable with other dry models (median: 4.00, IQR: 0.50), and considered adequate compared with wet lab experiences (median: 3.00, IQR: 1.00).
Discussion
Our model was met with high satisfaction from our sampled cohort. Current commercially available strabismus training models with refined materials are available [16] at a cost between £33 and 49 per eye. This is a substantial cost to training, as practice is limited to four recti muscles and/or two oblique muscles. In contrast, our self-developed model allows more practice by rejoining the recti onto the globe for a considerably lower cost (<£1–5). Furthermore, more experienced participants (senior trainees and consultants) reported that our low-cost model was comparable and favourable with other dry models they had used, and felt it adequately compared with cadaveric high-fidelity simulation, which is supportive of this model compared with other commercially available models.
Alterative descriptions of a low-cost model have been proposed, initially by Metz et al., who described a simple model using tennis ball (globe) and rubber band (rectus muscle) [17]. However, due to the density of the materials, Metz et al. advised practice of figure-of-eight sutures with 2-0 silk. This is an appreciably larger suture size than typically used in strabismus surgery where 6-0 vicryl is routinely employed. A recent modification by Adebayo et al. demonstrated that 6-0 polyglactin is also possible with alterative soft rubber band and ball model [18].
Adebayo et al. further performed construct validity by comparing single wet lab biological training to non-biological home training model and found comparable results at the end of a 1-month training exercise [18]. The demonstrated non-inferiority of non-biological wet lab training is further evidence that despite the limitation perceived, they can perform expensive wet lab training without use of animal tissue and cost constraints. Furthermore, they offer a deliberate distributed form of practice compared with single high-fidelity training, which has been shown to be more developmental towards learning [19].
The identified limitation of our model, replication of conjunctiva and feel of muscle dissection, is not unique to our model but can be applied to all non-biological models. Biological tissue planes and structures are difficult to replicate due to the level of hydration, thickness and variations in anatomy. The muscles were easily identified and therefore did not pose a challenge, when compared with biological models in which muscle-tenon fibre separation can prove far more difficult. White et al. evaluated composite simulated model using bacon acquired from local supermarket to simulate extraocular muscle surgery. This was found to be constructive to learning as the biological tissue offered a realistic approach to extraocular muscle tissue dynamics [12] with a relatively inexpensive cost. However, the Styrofoam base was a less favourable scleral substitute. Using composite biological tissue (e.g., bacon, chicken skin for conjunctiva) may therefore overcome some of the issues with non-biological materials, however, this requires further evaluation.
Generally, there was an agreement between our participants in their rating for each domain. Our model was commended by our 16 participants (3rd year ophthalmology trainees to consultants) that were surveyed in a low income economic country. The use of simulation models was not available due to cost and lack of commercial availability, and thus the participants reported the model as a useful tool to practice and visualise key stages of strabismus surgery.
Our expert group scored overall simulation, anatomy and feel of muscle securing and suturing higher than all our other participants. This is perhaps due to the general validity and applicability of the model to basic skills required in strabismus surgery from experience of surgery and training. However, there are elements of recall bias with our senior and expert participants, as we did not directly compare live surgery or other dry models during the time of the testing. Further sampling of experts is desirable to ascertain the likelihood of this effect but is difficult to assess in a single ophthalmic unit.
Conclusion
Our proposed low-cost accessible strabismus model scored positively in our survey. In particular, the model scored highly for muscle securing and suturing which we believe are the most challenging aspects of the surgical learning curve. The muscle dissection and conjunctival simulation were considered less realistic. Overall, participants felt that the model simulated horizontal muscle surgery well and was comparable to other dry simulation models.
Summary
What was known before
-
Ophthalmic surgical training has evolved to focus on key competency acquisition, with minimum procedural numbers required by completion of training.
-
Extraocular muscle surgery is an important multi-disciplinary skill for ophthalmic trainees for strabismus correction and other procedures, e.g., orbital surgery, scleral buckling, enucleation and globe repair.
-
Simulation training with models shows promise in aiding surgical skill acquisition.
-
There are limited data published on strabismus surgery training and model validity.
What this study adds
-
We present a low-cost strabismus surgical training model, easily constructed with commercially available materials.
-
Our model performed especially well for muscle securing and suturing which are the most critical steps in strabismus surgery.
-
This model can be created at home to allow flexible training suited to the individual trainee to practise and develop core strabismus surgical techniques.
References
Royal College of Ophthalmology Ophthalmic Specialist Training Curriculum. https://www.rcophth.ac.uk/curriculum/ost/faqs/. Accessed 16 Jul 2019.
Kotsis SV, Chung KC. Applications of see one, do one, teach one concept in surgical training. Plast Reconstr Surg. 2013;131:1194–201.
Royal College of Ophthalmology Ophthalmic Specialist Training Assessments. https://www.rcophth.ac.uk/curriculum/ost/assessments/. Accessed 16 Jul 2019.
Hoffman J, Spencer F, Ezra D, Day AC. Changes in UK Ophthalmology Surgical training: analysis of cumulative surgical experience 2009-2015. BMJ Open. 2017;7:e018526.
Ezra DG, Chandra A, Okhravi N, Sullivan P, McDonnel P, Lee J. Higher surgical training in ophthalmology: trends in cumulative surgical experience 1993–2008. Eye. 2010;24:1466–73.
Kim Y, Kim YG, Kim HJ, Shin JH, Han SB, Lee SJ, et al. Learning curves for strabismus surgery in two ophthalmologists. Indian J Ophthalmol. 2015;63:821–4.
Crespi-Flores VG, Minguini N, Temporini ER, De Carvalho KM. Strabismus surgery learning for ophthalmology resident of university service. Arq Bras Oftalmol. 2012;75:188–91.
McCannel CA. Simulation surgical teaching in ophthalmology. Ophthalmology. 2015;122:2371–2.
Schout BMA, Hendrikx AJM, Scheele F, Bemelmans BLH, Scherpbier AJJA. Validation and implementation of surgical simulators: a critical review of present, past and future. Surg Endosc. 2010;24:536–46.
Selvander M, Åsman P. Virtual reality cataract surgery training: learning curves and concurrent validity. Acta Ophthalmol. 2012;90:412–7.
Belyea DA, Brown SE, Rajjoub LZ. Influence of surgery simulator training on ophthalmology resident phacoemulsification performance. J Cataract Refract Surg. 2011;37:1756–61.
Thomsen AS, Subhi Y, Kiilgaard JF, Cour ML, Konge L. Update on simulation-based surgical training and assessment in ophthalmology. Ophthalmology. 2015;122:1111–30.
White CA, Wrzosek JA, Chesnutt DA, Enyedi LB, Cabrera MT. A Novel method for teaching key steps of strabismus surgery in the wet lab. J AAPOS. 2015;19:470–3.
M Malik, et al. Jain Free Eye Model, YoutTube. 2018. https://www.youtube.com/watch?v=PHGZnPZDdEY.
Gavazzi A, Bahsoun AN, Haute WV, Ahmed K, Elhage O, Jaye P, et al. Face, content and construct validity of a virtual reality simulator for robotic surgery (SEP Robot). Ann R Coll Surg Engl. 2011;93:15426–60.
Simulated Ocular Surgery. http://simulatedocularsurgery.com/product/strabismus-eye-basic/. Accessed 16 Jul 2019.
Metz HS, Aquaella JV, Sgabelloni CE. A model for eye muscle surgery. Arch Ophthalmol. 1980;98:117–8.
Adebayo T, Abendroth M, Elera GG, Kunselman A, Sinz E, Ely A, et al. Developing and validating a simple and cost-effective strabismus surgery simulator. J AAPOS. 2018;22:85–8.
Bjerrum F, Thomsen ASS, Nayahangan LJ, Konge L. Surgical simulation: current practices and future prospectives for technical skills training. Med Teach. 2018;40:668–75.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Malik, M., Shah, N., Kit, V. et al. Development of a low-cost strabismus surgery simulation model. Eye 35, 805–810 (2021). https://doi.org/10.1038/s41433-020-0966-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-0966-1
This article is cited by
-
An automated process for bulk downloading optical coherence tomography scans
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Quality assessment of polymer materials for human model eye development
International Ophthalmology (2023)