Abstract
Background
Dysregulation of endocrine pathways related to steroid and growth hormones may modify endometrial cancer risk; however, prospective data on testosterone, sex hormone-binding globulin (SHBG) and insulin-like growth factor (IGF)−1 are limited. To elucidate the role of these hormones in endometrial cancer risk we conducted complementary observational and Mendelian randomization (MR) analyses.
Methods
The observational analyses included 159,702 women (80% postmenopausal) enrolled in the UK Biobank. Hazard ratios (HRs) and 95% confidence intervals (CIs) were estimated using Cox proportional hazards models. For MR analyses, genetic variants associated with hormone levels were identified and their association with endometrial cancer (12,906 cases/108,979 controls) was examined using two-sample MR.
Results
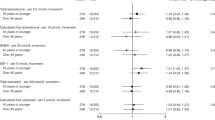
In the observational analysis, higher circulating concentrations of total (HR per unit inverse normal scale = 1.38, 95% CI = 1.22–1.57) and free testosterone (HR per unit log scale = 2.07, 95% CI = 1.66–2.58) were associated with higher endometrial cancer risk. An inverse association was found for SHBG (HR per unit inverse normal scale = 0.76, 95% CI = 0.67–0.86). Results for testosterone and SHBG were supported by the MR analyses. No association was found between genetically predicted IGF-1 concentration and endometrial cancer risk.
Conclusions
Our results support probable causal associations between circulating concentrations of testosterone and SHBG with endometrial cancer risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data used in the MR analyses can be found in supplementary material. Researchers can apply to use the UK Biobank dataset by registering and applying at http://ukbiobank.ac.uk/register-apply/.
References
Allen NE, Key TJ, Dossus L, Rinaldi S, Cust A, Lukanova A, et al. Endogenous sex hormones and endometrial cancer risk in women in the European Prospective Investigation into Cancer and Nutrition (EPIC). Endocr Relat Cancer. 2008;15:485–97.
Brinton LA, Trabert B, Anderson GL, Falk RT, Felix AS, Fuhrman BJ, et al. Serum estrogens and estrogen metabolites and endometrial cancer risk among postmenopausal women. Cancer Epidemiol Biomark Prev. 2016;25:1081–9.
Gunter MJ, Hoover DR, Yu H, Wassertheil-Smoller S, Manson JE, Li J, et al. A prospective evaluation of insulin and insulin-like growth factor-I as risk factors for endometrial cancer. Cancer Epidemiol Biomark Prev. 2008;17:921–9.
Lukanova A, Lundin E, Micheli A, Arslan A, Ferrari P, Rinaldi S, et al. Circulating levels of sex steroid hormones and risk of endometrial cancer in postmenopausal women. Int J Cancer. 2004;108:425–32.
Zeleniuch-Jacquotte A, Akhmedkhanov A, Kato I, Koenig KL, Shore RE, Kim MY, et al. Postmenopausal endogenous oestrogens and risk of endometrial cancer: results of a prospective study. Br J Cancer. 2001;84:975–81.
Clendenen TV, Hertzmark K, Koenig KL, Lundin E, Rinaldi S, Johnson T, et al. Premenopausal circulating androgens and risk of endometrial cancer: results of a prospective study. Hormones Cancer. 2016;7:178–87.
Michels KA, Brinton LA, Wentzensen N, Pan K, Chen C, Anderson GL, et al. Postmenopausal androgen metabolism and endometrial cancer risk in the women’s health initiative observational study. JNCI Cancer Spectr. 2019;3:pkz029.
Fortunati N, Catalano MG. Sex hormone-binding globulin (SHBG) and estradiol cross-talk in breast cancer cells. Horm Metab Res. 2006;38:236–40.
Pollak M. Insulin and insulin-like growth factor signalling in neoplasia. Nat Rev Cancer. 2008;8:915–28.
Samani AA, Yakar S, LeRoith D, Brodt P. The role of the IGF system in cancer growth and metastasis: overview and recent insights. Endocr Rev. 2007;28:20–47.
Mynarcik DC, Williams PF, Schaffer L, Yu GQ, Whittaker J. Identification of common ligand binding determinants of the insulin and insulin-like growth factor 1 receptors. Insights into mechanisms of ligand binding. J Biol Chem. 1997;272:18650–5.
Yu H, Rohan T. Role of the insulin-like growth factor family in cancer development and progression. J Natl Cancer Inst. 2000;92:1472–89.
Augustin LS, Dal Maso L, Franceschi S, Talamini R, Kendall CW, Jenkins DJ, et al. Association between components of the insulin-like growth factor system and endometrial cancer risk. Oncology. 2004;67:54–9.
Lacey JV Jr, Potischman N, Madigan MP, Berman ML, Mortel R, Twiggs LB, et al. Insulin-like growth factors, insulin-like growth factor-binding proteins, and endometrial cancer in postmenopausal women: results from a U.S. case-control study. Cancer Epidemiol Biomark Prev. 2004;13:607–12.
Lukanova A, Zeleniuch-Jacquotte A, Lundin E, Micheli A, Arslan AA, Rinaldi S, et al. Prediagnostic levels of C-peptide, IGF-I, IGFBP -1, −2 and −3 and risk of endometrial cancer. Int J Cancer. 2004;108:262–8.
Oh JC, Wu W, Tortolero-Luna G, Broaddus R, Gershenson DM, Burke TW, et al. Increased plasma levels of insulin-like growth factor 2 and insulin-like growth factor binding protein 3 are associated with endometrial cancer risk. Cancer Epidemiol Biomark Prev. 2004;13:748–52.
Petridou E, Koukoulomatis P, Alexe DM, Voulgaris Z, Spanos E, Trichopoulos D. Endometrial cancer and the IGF system: a case-control study in Greece. Oncology. 2003;64:341–5.
Weiderpass E, Brismar K, Bellocco R, Vainio H, Kaaks R. Serum levels of insulin-like growth factor-I, IGF-binding protein 1 and 3, and insulin and endometrial cancer risk. Br J Cancer. 2003;89:1697–704.
Hosgood HD, Gunter MJ, Murphy N, Rohan TE, Strickler HD. The relation of obesity-related hormonal and cytokine levels with multiple myeloma and non-Hodgkin lymphoma. Front Oncol. 2018;8:103.
Ogo Y, Taniuchi S, Ojima F, Hayashi S, Murakami I, Saito Y, et al. IGF-1 gene expression is differentially regulated by estrogen receptors alpha and beta in mouse endometrial stromal cells and ovarian granulosa cells. J Reprod Dev. 2014;60:216–23.
Neale Lab. UK Biobank GWAS Results. 2019. http://www.nealelab.is/uk-biobank. Accessed 30 Sept 2019.
Ruth KS, Day FR, Tyrrell J, Thompson DJ, Wood AR, Mahajan A, et al. Using human genetics to understand the disease impacts of testosterone in men and women. Nat Med. 2020;26:252–8.
O’Mara TA, Glubb DM, Amant F, Annibali D, Ashton K, Attia J, et al. Identification of nine new susceptibility loci for endometrial cancer. Nat Commun. 2018;9:3166.
UK-Biobank. Protocol for a large-scale prospective epidemiological resources. https://www.ukbiobank.ac.uk/ 2010.
Fry A, Littlejohns TJ, Sudlow C, Doherty N, Adamska L, Sprosen T, et al. Comparison of sociodemographic and health-related characteristics of UK Biobank participants with those of the general population. Am J Epidemiol. 2017;186:1026–34.
Elliott P, Peakman TC, Biobank UK. The UK Biobank sample handling and storage protocol for the collection, processing and archiving of human blood and urine. Int J Epidemiol. 2008;37:234–44.
UK-Biobank. UK Biobank Biomarker Project—companion document to accompany serum biomarker data. https://biobank.ndph.ox.ac.uk/showcase/showcase/docs/serum_biochemistry.pdf 2019.
Sodergard R, Backstrom T, Shanbhag V, Carstensen H. Calculation of free and bound fractions of testosterone and estradiol-17 beta to human plasma proteins at body temperature. J Steroid Biochem. 1982;16:801–10.
Watts EL, Appleby PN, Perez-Cornago A, Bueno-de-Mesquita HB, Chan JM, Chen C, et al. Low free testosterone and prostate cancer risk: a collaborative analysis of 20 prospective studies. Eur Urol. 2018;74:585–94.
Townsend P. Deprivation. J Soc Policy. 1987;16:125–46.
MacMahon S, Peto R, Cutler J, Collins R, Sorlie P, Neaton J, et al. Blood pressure, stroke, and coronary heart disease. Part 1, Prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet. 1990;335:765–74.
Clarke R, Emberson JR, Breeze E, Casas JP, Parish S, Hingorani AD, et al. Biomarkers of inflammation predict both vascular and non-vascular mortality in older men. Eur Heart J. 2008;29:800–9.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B (Methodol.). 1995;57:289–300.
Schoenfeld D. Partial residuals for the proportional hazards regression model. Biometrika. 1982;69:239–41.
Murphy N, Knuppel A, Papadimitriou N, Martin RM, Tsilidis KK, Smith-Byrne K, et al. Insulin-like growth factor-1, insulin-like growth factor-binding protein-3, and breast cancer risk: observational and Mendelian randomization analyses with approximately 430 000 women. Ann Oncol. 2020;31:641–9.
Day FR, Loh PR, Scott RA, Ong KK, Perry JR. A robust example of collider bias in a Genetic Association Study. Am J Hum Genet. 2016;98:392–3.
Bowden J, Del Greco MF, Minelli C, Davey Smith G, Sheehan N, Thompson J. A framework for the investigation of pleiotropy in two-sample summary data Mendelian randomization. Stat Med. 2017;36:1783–802.
Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol. 2013;37:658–65.
Burgess S, Scott RA, Timpson NJ, Davey Smith G, Thompson SG. Using published data in Mendelian randomization: a blueprint for efficient identification of causal risk factors. Eur J Epidemiol. 2015;30:543–52.
Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10:101–29.
Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44:512–25.
Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 2016;40:304–14.
Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. 2018;50:693–8.
Haas ME, Aragam KG, Emdin CA, Bick AG, International Consortium for Blood Pressure, Hemani, G, et al. Genetic association of albuminuria with cardiometabolic disease and blood pressure. Am J Hum Genet. 2018;103:461–73.
Hemani G, Tilling K, Smith, GD. Correction: Orienting the causal relationship between imprecisely measured traits using GWAS summary data. PLoS Genet. 2017;13:e1007149.
Yavorska OO, Burgess S. MendelianRandomization: an R package for performing Mendelian randomization analyses using summarized data. Int J Epidemiol. 2017;46:1734–9.
Ito K, Miki Y, Suzuki T, McNamara KM, Sasano H. In situ androgen and estrogen biosynthesis in endometrial cancer: focus on androgen actions and intratumoral production. Endocr Relat Cancer. 2016;23:R323–335.
Larsson SC, Carter P, Vithayathil M, Kar S, Mason AM, Burgess S. Insulin-like growth factor-1 and site-specific cancers: a Mendelian randomization study. Cancer Med. 2020;9:6836–42.
Murphy LJ, Ghahary A. Uterine insulin-like growth factor-1: regulation of expression and its role in estrogen-induced uterine proliferation. Endocr Rev. 1990;11:443–53.
Clarke R, Shipley M, Lewington S, Youngman L, Collins R, Marmot M, et al. Underestimation of risk associations due to regression dilution in long-term follow-up of prospective studies. Am J Epidemiol. 1999;150:341–53.
Rauh M. LC-MS/MS for protein and peptide quantification in clinical chemistry. J Chromatogr B Anal Technol Biomed Life Sci. 2012;883-4:59–67.
Burgess S, Davies NM, Thompson SG. Bias due to participant overlap in two-sample Mendelian randomization. Genet Epidemiol. 2016;40:597–608.
Acknowledgements
This work has been conducted using the UK Biobank Resource under Application Numbers 8294, and we express our gratitude to the participants and those involved in building the resource. UK Biobank is an open access resource. Bona fide researchers can apply to use the UK Biobank dataset by registering and applying at http://ukbiobank.ac.uk/register-apply/.
Funding
This work was supported by the French National Cancer Institute (INCa SHSESP17, grant no. 2017–127) and by Cancer Research UK (C18281/A29019).
Author information
Authors and Affiliations
Contributions
AM, ND, MJG and NM: Designed the study and developed the methodology, analysed the data, interpreted the results, drafted the paper and approved the final version. NA and TO’M: Interpreted the results, edited the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
UK Biobank has approval from the North-West Multi-Centre Research Ethics Committee, the National Information Governance Board for Health & Social Care in England and Wales and the Community Health Index Advisory Group in Scotland. Written informed consent was provided by all participants.
Consent to publish
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Mullee, A., Dimou, N., Allen, N. et al. Testosterone, sex hormone-binding globulin, insulin-like growth factor-1 and endometrial cancer risk: observational and Mendelian randomization analyses. Br J Cancer 125, 1308–1317 (2021). https://doi.org/10.1038/s41416-021-01518-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-021-01518-3
This article is cited by
-
Postmenopausal onset of androgen excess: a diagnostic and therapeutic algorithm based on extensive clinical experience
Journal of Endocrinological Investigation (2024)
-
UK Biobank: a globally important resource for cancer research
British Journal of Cancer (2023)
-
Identifying molecular mediators of the relationship between body mass index and endometrial cancer risk: a Mendelian randomization analysis
BMC Medicine (2022)
-
Androgens in endometrial carcinoma: the killer or helper?
Journal of Endocrinological Investigation (2022)