Abstract
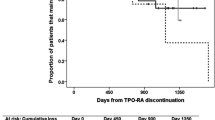
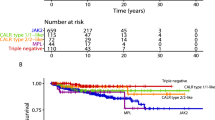
Persistent thrombocytopenia (PT) has an unsatisfactory response to therapy after haploidentical haematopoietic stem cell transplantation (haplo-HSCT). We retrospectively evaluated the safety and efficacy of avatrombopag treatment in 69 patients with PT following haplo-HSCT and assessed whether baseline thrombopoietin (TPO) levels could predict treatment response. Overall response (OR) and complete response (CR) were defined as increased platelet levels to over 20 × 109/L or 50 × 109/L independent of platelet transfusion during or within 7 days of the end of avatrombopag treatment, respectively. The incidences of OR and CR were 72.5% and 58.0%, with a median of 11 and 29 days to OR and CR, respectively. ROC analysis suggested that the optimally discriminant baseline TPO level threshold for both OR and CR to avatrombopag was ≤ 1714 pg/mL. In multivariate analysis, a lower baseline TPO level (P = 0.005) was a significant independent factor of response to avatrombopag. For patients resistant to other TPO receptor agonists (TPO-RAs), 9/16 (56.3%) exhibited a response after switching to avatrombopag. Avatrombopag was well tolerated, and responders achieved improved overall survival (79.0% vs. 91.1%, P = 0.001). In conclusion, avatrombopag is a potential safe and effective treatment for PT after haplo-HSCT, and lower baseline TPO levels predicted a better response.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
References
Tang FF, Sun YQ, Mo XD, Lv M, Chen YH, Wang Y, et al. Incidence, Risk Factors, and Outcomes of Primary Prolonged Isolated Thrombocytopenia after Haploidentical Hematopoietic Stem Cell Transplant. Biol Blood Marrow Transpl. 2020;26:1452–8.
Zhao X, Zhao X, Huo M, Fan Q, Pei X, Wang Y, et al. Donor-Specific Anti-Human Leukocyte Antigen Antibodies Predict Prolonged Isolated Thrombocytopenia and Inferior Outcomes of Haploidentical Hematopoietic Stem Cell Transplantation. J Immunol Res. 2017;2017:1043836.
Akahoshi Y, Kimura SI, Gomyo A, Hayakawa J, Tamaki M, Harada N, et al. Delayed platelet recovery after allogeneic hematopoietic stem cell transplantation: Association with chronic graft-versus-host disease and survival outcome. Hematol Oncol. 2018;36:276–84.
Labrador J, Lopez-Corral L, Vazquez L, Sanchez-Guijo F, Guerrero C, Sanchez-Barba M, et al. Incidence and risk factors for life-threatening bleeding after allogeneic stem cell transplant. Brit J Haematol. 2015;169:719–25.
Akahoshi Y, Kanda J, Gomyo A, Hayakawa J, Komiya Y, Harada N, et al. Risk Factors and Impact of Secondary Failure of Platelet Recovery After Allogeneic Stem Cell Transplantation. Biol Blood Marrow Transpl. 2016;22:1678–83.
Stasia A, Ghiso A, Galaverna F, Raiola AM, Gualandi F, Luchetti S, et al. CD34 selected cells for the treatment of poor graft function after allogeneic stem cell transplantation. Biol Blood Marrow Transpl. 2014;20:1440–3.
Sun YQ, Wang Y, Wang FR, Yan CH, Cheng YF, Chen YH, et al. Graft Failure in Patients With Hematological Malignancies: A Successful Salvage With a Second Transplantation From a Different Haploidentical Donor. Front Med-lausanne. 2021;8:604085.
de Sauvage FJ, Villeval JL, Shivdasani RA. Regulation of megakaryocytopoiesis and platelet production: lessons from animal models. J Lab Clin Med. 1998;131:496–501.
Kaushansky K, Lok S, Holly RD, Broudy VC, Lin N, Bailey MC, et al. Promotion of megakaryocyte progenitor expansion and differentiation by the c-Mpl ligand thrombopoietin. Nature. 1994;369:568–71.
Gurney AL, Carver-Moore K, de Sauvage FJ, Moore MW. Thrombocytopenia in c-mpl-deficient mice. Science. 1994;265:1445–7.
Fu H, Zhang X, Xu L, Liu K, Huang X. Characterization of thrombopoietin kinetics within 60 days after allogeneic hematopoietic stem cell transplantation and its correlation with megakaryocyte ploidy distribution. Clin Transplant. 2016;30:170–8.
Zhang X, Fu H, Xu L, Liu D, Wang J, Liu K, et al. Prolonged thrombocytopenia following allogeneic hematopoietic stem cell transplantation and its association with a reduction in ploidy and an immaturation of megakaryocytes. Biol Blood Marrow Transplant. 2011;17:274–80.
Erickson-Miller CL, Delorme E, Tian SS, Hopson CB, Landis AJ, Valoret EI, et al. Preclinical activity of eltrombopag (SB-497115), an oral, nonpeptide thrombopoietin receptor agonist. Stem Cells. 2009;27:424–30.
Bento L, Bastida JM, Garcia-Cadenas I, Garcia-Torres E, Rivera D, Bosch-Vilaseca A, et al. Thrombopoietin Receptor Agonists for Severe Thrombocytopenia after Allogeneic Stem Cell Transplantation: Experience of the Spanish Group of Hematopoietic Stem Cell Transplant. Biol Blood Marrow Transplant. 2019;25:1825–31.
Fu H, Zhang X, Han T, Mo X, Wang Y, Chen H, et al. Eltrombopag is an effective and safe therapy for refractory thrombocytopenia after haploidentical hematopoietic stem cell transplantation. Bone Marrow Transpl. 2019;54:1310–8.
Sun YQ, Kong Y, Zhang XH, Wang Y, Shi MM, Song Y, et al. A novel recombinant human thrombopoietin for treating prolonged isolated thrombocytopenia after allogeneic stem cell transplantation. Platelets. 2019;30:994–1000.
Jurczak W, Chojnowski K, Mayer J, Krawczyk K, Jamieson BD, Tian W, et al. Phase 3 randomised study of avatrombopag, a novel thrombopoietin receptor agonist for the treatment of chronic immune thrombocytopenia. Brit J Haematol. 2018;183:479–90.
Wang Y, Liu QF, Xu LP, Liu KY, Zhang XH, Ma X, et al. Haploidentical vs identical-sibling transplant for AML in remission: a multicenter, prospective study. Blood. 2015;125:3956–62.
Xiao-Jun H, Lan-Ping X, Kai-Yan L, Dai-Hong L, Yu W, Huan C, et al. Partially matched related donor transplantation can achieve outcomes comparable with unrelated donor transplantation for patients with hematologic malignancies. Clin Cancer Res. 2009;15:4777–83.
Bashey A, Zhang X, Sizemore CA, Manion K, Brown S, Holland HK, et al. T-cell-replete HLA-haploidentical hematopoietic transplantation for hematologic malignancies using post-transplantation cyclophosphamide results in outcomes equivalent to those of contemporaneous HLA-matched related and unrelated donor transplantation. J Clin Oncol. 2013;31:1310–6.
Sun YQ, He GL, Chang YJ, Xu LP, Zhang XH, Han W, et al. The incidence, risk factors, and outcomes of primary poor graft function after unmanipulated haploidentical stem cell transplantation. Ann Hematol. 2015;94:1699–705.
Xu L, Chen H, Chen J, Han M, Huang H, Lai Y, et al. The consensus on indications, conditioning regimen, and donor selection of allogeneic hematopoietic cell transplantation for hematological diseases in China-recommendations from the Chinese Society of Hematology. J Hematol Oncol. 2018;11:33.
Zhang XH, Chen J, Han MZ, Huang H, Jiang EL, Jiang M, et al. The consensus from The Chinese Society of Hematology on indications, conditioning regimens and donor selection for allogeneic hematopoietic stem cell transplantation: 2021 update. J Hematol Oncol. 2021;14:145.
Chang YJ, Luznik L, Fuchs EJ, Huang XJ. How do we choose the best donor for T-cell-replete, HLA-haploidentical transplantation? J Hematol Oncol. 2016;9:35.
Shi MM, Kong Y, Song Y, Sun YQ, Wang Y, Zhang XH, et al. Atorvastatin enhances endothelial cell function in posttransplant poor graft function. Blood. 2016;128:2988–99.
Qin XY, Li GX, Qin YZ, Wang Y, Wang FR, Liu DH, et al. Quantitative assessment of hematopoietic chimerism by quantitative real-time polymerase chain reaction of sequence polymorphism systems after hematopoietic stem cell transplantation. Chinese Med J-Peking. 2011;124:2301–8.
Markham A. Avatrombopag: A Review in Thrombocytopenia. Drugs. 2021;81:1905–13.
Zhou M, Qi J, Gu C, Wang H, Zhang Z, Wu D, et al. Avatrombopag for the treatment of thrombocytopenia post hematopoietic stem-cell transplantation. Ther Adv Hematol. 2022;13:20406207221127532.
de Graaf CA, Metcalf D. Thrombopoietin and hematopoietic stem cells. Cell Cycle. 2011;10:1582–9.
Sungaran R, Chisholm OT, Markovic B, Khachigian LM, Tanaka Y, Chong BH. The role of platelet alpha-granular proteins in the regulation of thrombopoietin messenger RNA expression in human bone marrow stromal cells. Blood. 2000;95:3094–101.
Lok S, Kaushansky K, Holly RD, Kuijper JL, Lofton-Day CE, Oort PJ, et al. Cloning and expression of murine thrombopoietin cDNA and stimulation of platelet production in vivo. Nature. 1994;369:565–8.
Kuter DJ, Beeler DL, Rosenberg RD. The purification of megapoietin: a physiological regulator of megakaryocyte growth and platelet production. P Natl Acad Sci USA. 1994;91:11104–8.
Shinjo K, Takeshita A, Nakamura S, Naitoh K, Yanagi M, Tobita T, et al. Serum thrombopoietin levels in patients correlate inversely with platelet counts during chemotherapy-induced thrombocytopenia. Leukemia. 1998;12:295–300.
Goldberg MA, Gaut CC, Bunn HF. Erythropoietin mRNA levels are governed by both the rate of gene transcription and posttranscriptional events. Blood. 1991;77:271–7.
Stoffel R, Wiestner A, Skoda RC. Thrombopoietin in thrombocytopenic mice: evidence against regulation at the mRNA level and for a direct regulatory role of platelets. Blood. 1996;87:567–73.
Geddis AE, Fox NE, Kaushansky K. The Mpl receptor expressed on endothelial cells does not contribute significantly to the regulation of circulating thrombopoietin levels. Exp Hematol. 2006;34:82–6.
Debili N, Wendling F, Cosman D, Titeux M, Florindo C, Dusanter-Fourt I, et al. The Mpl receptor is expressed in the megakaryocytic lineage from late progenitors to platelets. Blood. 1995;85:391–401.
Katayama N, Itoh R, Kato T, Sugawara T, Mahmud N, Ohishi K, et al. Role for C-MPL and its ligand thrombopoietin in early hematopoiesis. Leukemia Lymphoma. 1997;28:51–6.
Buza-Vidas N, Antonchuk J, Qian H, Mansson R, Luc S, Zandi S, et al. Cytokines regulate postnatal hematopoietic stem cell expansion: opposing roles of thrombopoietin and LNK. Gene Dev. 2006;20:2018–23.
Emmons RV, Reid DM, Cohen RL, Meng G, Young NS, Dunbar CE, et al. Human thrombopoietin levels are high when thrombocytopenia is due to megakaryocyte deficiency and low when due to increased platelet destruction. Blood. 1996;87:4068–71.
Kuter DJ, Gernsheimer TB. Thrombopoietin and platelet production in chronic immune thrombocytopenia. Hematol Oncol Clin North Am. 2009;23:1193–211.
Zeigler FC, de Sauvage F, Widmer HR, Keller GA, Donahue C, Schreiber RD, et al. In vitro megakaryocytopoietic and thrombopoietic activity of c-mpl ligand (TPO) on purified murine hematopoietic stem cells. Blood. 1994;84:4045–52.
Alexander WS, Roberts AW, Nicola NA, Li R, Metcalf D. Deficiencies in progenitor cells of multiple hematopoietic lineages and defective megakaryocytopoiesis in mice lacking the thrombopoietic receptor c-Mpl. Blood. 1996;87:2162–70.
Carver-Moore K, Broxmeyer HE, Luoh SM, Cooper S, Peng J, Burstein SA, et al. Low levels of erythroid and myeloid progenitors in thrombopoietin-and c-mpl-deficient mice. Blood. 1996;88:803–8.
Ghanima W, Cooper N, Rodeghiero F, Godeau B, Bussel JB. Thrombopoietin receptor agonists: ten years later. Haematologica. 2019;104:1112–23.
Qi J, Zheng L, Hu B, Zhou H, He Q, Liu H, et al. Pharmacokinetics, Safety, and Pharmacodynamics of Romiplostim in Chinese Subjects With Immune Thrombocytopenia: A Phase I/II Trial. Clin Pharm Drug Dev. 2022;11:379–87.
Di Buduo CA, Currao M, Pecci A, Kaplan DL, Balduini CL, Balduini A. Revealing eltrombopag’s promotion of human megakaryopoiesis through AKT/ERK-dependent pathway activation. Haematologica. 2016;101:1479–88.
Al-Samkari H, Kuter DJ. Relative potency of the thrombopoietin receptor agonists eltrombopag, avatrombopag and romiplostim in a patient with chronic immune thrombocytopenia. Brit J Haematol. 2018;183:168.
Lakhwani S, Perera M, Fernandez-Fuertes F, Rios DPM, Torres M, Raya JM, et al. Thrombopoietin receptor agonist switch in adult primary immune thrombocytopenia patients: A retrospective collaborative survey involving 4 Spanish centres. Eur J Haematol. 2017;99:372–7.
Al-Samkari H, Jiang D, Gernsheimer T, Liebman H, Lee S, Wojdyla M, et al. Adults with immune thrombocytopenia who switched to avatrombopag following prior treatment with eltrombopag or romiplostim: A multicentre US study. Brit J Haematol. 2022;197:359–66.
Kuter DJ, Mufti GJ, Bain BJ, Hasserjian RP, Davis W, Rutstein M. Evaluation of bone marrow reticulin formation in chronic immune thrombocytopenia patients treated with romiplostim. Blood. 2009;114:3748–56.
Brynes RK, Orazi A, Theodore D, Burgess P, Bailey CK, Thein MM, et al. Evaluation of bone marrow reticulin in patients with chronic immune thrombocytopenia treated with eltrombopag: Data from the EXTEND study. Am J Hematol. 2015;90:598–601.
Acknowledgements
We appreciate the participating investigators and patients.
Funding
This work was supported by National Key Research and Development Program of China (No. 2021YFC2500304), Key Program of National Natural Science Foundation of China (No. 82230004), National Natural Science Foundation of China (No. 81970113), Beijing Natural Science Foundation (No.7232188) and the Capital Health Research and Development of Special (No. 2022-1-4082) and MOE Engineering Center of Hematological Disease, Soochow University.
Author information
Authors and Affiliations
Contributions
XHZ contributed to the study design. HXF contributed to the data analysis and manuscript writing. HXL contributed to data analysis. All authors contributed to the study execution and data collection. All authors provided a full review of the article and are fully responsible for all content and editorial decisions, were involved in all stages of manuscript development, and have approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
All authors read and approved the final version of this manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fu, H., Lv, M., Liu, H. et al. Thrombopoietin level predicts the response to avatrombopag treatment for persistent thrombocytopenia after haploidentical haematopoietic stem cell transplantation. Bone Marrow Transplant 58, 1368–1376 (2023). https://doi.org/10.1038/s41409-023-02100-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-02100-6