Abstract
The raphe nuclei comprise nearly all of 5-hydroxytryptaminergic (5-HTergic) neurons in the brain and are widely acknowledged to participate in the modulation of neural excitability. “Excitability-inhibition imbalance” results in a variety of brain disorders, including epilepsy. Epilepsy is a common neurological disorder characterized by hypersynchronous epileptic seizures accompanied by many psychological, social, cognitive consequences. Current antiepileptic drugs and other therapeutics are not ideal to control epilepsy and its comorbidities. Cumulative evidence suggests that the raphe nuclei and 5-HTergic system play an important role in epilepsy and epilepsy-associated comorbidities. Seizure activities propagate to the raphe nuclei and induce various alterations in different subregions of the raphe nuclei at the cellular and molecular levels. Intervention of the activity of raphe nuclei and raphe 5-HTergic system with pharmacological or genetic approaches, deep brain stimulation or optogenetics produces indeed diverse and even contradictory effects on seizure and epilepsy-associated comorbidities in different epilepsy models. Nevertheless, there are still many open questions left, especially regarding to the relationship between 5-HTergic neural circuit and epilepsy. Understanding of 5-HTergic network in a circuit- and molecule-specific way may not only be therapeutically relevant for increasing the drug specificity and precise treatment in epilepsy, but also provide critical hints for other brain disorders with abnormal neural excitability. In this review we focus on the roles of the raphe 5-HTergic system in epilepsy and epilepsy-associated comorbidities. Besides, further perspectives about the complexity and diversity of the raphe nuclei in epilepsy are also addressed.
Similar content being viewed by others
Introduction
Epilepsy is one of the most common serious neurological disorders afflicting nearly 1% of people worldwide. It is caused by aberrant synchronized firing of neuronal populations primarily due to an “excitation-inhibition imbalance” in both cellular and circuit level [1]. Epilepsy is now recognized as a brain disorder not only by an enduring predisposition to generate epileptic seizures, but also by the psychological, social, and cognitive consequences. Notably, mood disorders such as depression and anxiety are the most frequent psychiatric comorbidities in patients with epilepsy [2]. Unfortunately, currently no available antiepileptic drugs (AEDs) or other therapeutic interventions are able to control epilepsy and its comorbidities. Numerous researches have shown that the raphe nuclei 5-hydroxytryptamine (5-HT)ergic system plays an important role not only in many physiological functions such as mood regulation, but also in epileptic seizures, which make it an attractive target from the perspective view of therapeutic significance. In this review, we will focus on role of the raphe 5-HTergic system in epilepsy and epilepsy-associated comorbidities. Besides, further perspectives about the complexity and diversity of the raphe nuclei in epilepsy are proposed at the end of the review.
Characteristics of the raphe 5-HTergic system and its role in neural excitability
The raphe nuclei are positioned midline in the brainstem along the rostro-caudal extension (Fig. 1a). The raphe nuclei are categorized, on the ground of their distributions and major projections, in one of two clusters: the rostral group which includes the dorsal raphe nucleus (DR), the median raphe nucleus (MR), and the caudal linear nucleus (CLi), and the caudal group which is divided into the raphe magnus (RMg), the nucleus raphe pallidus (RPa) and the nucleus raphe obscurus (ROb) [3]. The rostral group (also called the midbrain raphe) develops from mesopontine and mainly projects to the forebrain, while the caudal group (also called the medullary raphe) develops from medullary primordia and mainly projects to the caudal brainstem and the spinal cord. The midbrain raphe especially the DR and MR are functionally associated with sensory processing, cognition, emotional states, circadian rhythms, food intake, and reproduction [4, 5]. They have dense interconnections to the limbic system and may contribute to the generation and propagation of seizure in temporal lobe epilepsy (TLE) as well as the comorbidity of epilepsy [6, 7]. The medullary raphe participates in the regulation of autonomic and somatomotor responsiveness, particularly in respiratory control and pain control [8, 9]. They are considered to play a critical role in sudden unexpected death in epilepsy (SUDEP).
a Subregions of the raphe nuclei. The midbrain raphe includes the dorsal raphe nucleus (DR), the median raphe nucleus (MR) and the caudal linear nucleus (CLi). The medullary raphe includes the raphe magnus (RMg), the nucleus raphe pallidus (RPa), and the nucleus raphe obscurus (ROb). b Type and percentage of the MR neurons. VGLUT3, vesicular glutamate transporter 3. VGAT, vesicular GABA transporter. c The synthesis, release, reuptake, and degradation process of 5-HT and the signaling pathway of 5-HT receptors. BBB, blood-brain barrier. DAG, diacylglycerol. DDC, aromatic L-amino-acid decarboxylase. IP, inositol phosphates. MAOA and MOAB, metabolic enzymes monoamine oxidase A and B. PKC, protein kinase C. PKA, protein kinase A. SERT, 5-HT reuptake transporter. TPH2, tryptophan 5-hydroxylase 2. VMAT2, vesicular monoamine transporter 2.
The neuronal constituents of the raphe nuclei are heterogeneous: apart from large amounts of 5-HTergic neurons, they also contain glutamatergic neurons, GABAergic (gamma-aminobutyric acid) neurons, dopaminergic neurons and diverse peptidergic neurons (Fig. 1b) [10]. In the central nervous system, nearly all of the 5-HTergic neurons are distributed in the raphe nuclei, which release 5-HT as their main neurotransmitter and are implicated in many physiological functions (Fig. 1c). In this process, tryptophan is firstly transported across the blood-brain barrier (BBB) by the large neutral amino acid transporter and converted into 5-HT through a biosynthesis pathway including the enzymes tryptophan 5-hydroxylase 2 (TPH2) and aromatic L-amino-acid decarboxylase (DDC). Then, 5-HT is packaged into the vesicles by vesicular monoamine transporter 2 and released to specific postsynaptic targets or broadly to distant targets via volume transmission. Extracellular 5-HT can be transported across the plasma membrane by the 5-HT reuptake transporter (SERT) and broken down by the metabolic enzyme monoamine oxidase A and B.
The functions of 5-HT are mediated by at least 14 classes of receptors which are currently divided into seven families (5-HT1 to 5-HT7) according to their structural, functional, and pharmacological characteristics (Fig. 1c) [11]. 5-HT1 and 5-HT5 receptors families negatively coupled to adenylate cyclase via G-protein αi subunit (Gi/Go), thereby inhibiting the conversion of ATP to cAMP. Contrary to it, 5-HT4, 5-HT6 and 5-HT7 receptors families stimulate adenylate cyclase through the G-protein αs subunit (Gs). Then, cAMP acts an intracellular second messenger that interacts with many targets including cyclic nucleotide-gated ion channels and the phosphorylation of protein kinase A, contributing to the regulation of gene expression in many biological responses. In addition, 5-HT1a autoreceptor uses Gβγ subunit to directly activate Kir.3 K+ channels (GIRK) and inhibit (N and P/Q-type) Ca2+ channels, which lead to the inhibition of serotoninergic perikarya. Conversely, 5-HT1b autoreceptor makes an inhibition on serotoninergic terminals by potentiating Ca2+ dependent K+ channels. 5-HT2a–c receptors families recruit phospholipase C via the G-protein αq/11 subunit (Gq/G11), resulting in the formation of diacylglycerol and inositol phosphates, which then activate protein kinase C and elevate intracellular calcium. 5-HT3 receptor is a serotonin-gated cation channel, and its activation can cause membrane depolarization.
Different 5-HT receptors are distributed diversely in the brain and play important but diverse roles in the balance of neural excitability. The 5-HT1a receptor is expressed in the most 5-HTergic neurons of the raphe nuclei acting as a presynaptic inhibitory autoreceptor. It is also distributed postsynaptically in the forebrain including in cholinergic neurons of the septum and glutamatergic neurons in the hippocampus and neocortex. The 5-HT3 receptor is densely expressed in the brainstem and spinal cord, as well as has lower expressions in the cortex and limbic regions. Activation of the raphe neurons produced a rapid activation of dorsal CA1 interneurons via 5-HT3 receptor and AMPA/NMDA receptors, and also induced slow hyperpolarization of pyramidal neurons via 5-HT1a receptor [12]. Besides, optogenetic activation of serotoninergic fibers in the CA1 elicited long-lasting potentiation of the CA3-CA1 synaptic transmission, which was blocked by 5-HT4 receptor antagonist [13]. However, in the prefrontal cortex, 5-HT1a receptor agonist preferentially inhibited GABAergic interneurons, and thereby increased the firing rate of pyramidal neuron [14]. In subthalamic nucleus, 5-HT application principally increased neuronal firing rate through 5-HT2c and 5-HT4 receptors, and inhibited a minor of neurons by 5-HT1a receptors [15]. Furthermore, 5-HT receptors are engaged in modulating various neurochemical transmission, e.g., glutamate, GABA, dopamine, acetylcholine, and norepinephrine. For example, 5-HT2a receptor activation induced increase in firing frequency of ventral tegmental area dopamine neurons, and thereby elicited dopamine release in the prefrontal cortex [16]. Apart from 14 complicated receptors, a large number of studies have shown that the 5-HT neurons are diverse in anatomy, morphology, hodology, developmental lineage, gene expression, and electrophysiology [17]. It suggests that the raphe 5-HTergic system is composed of different subsystems which may be functionally heterogeneous. Abnormal neural excitability in the brain could lead to many common and severe brain disorders, among which epilepsy is one typical disorder traditionally considered to be caused by hyper-excitation. In the following part, we summary diverse roles of the raphe 5-HTergic system in epilepsy, which also have critical hints for studying its role in other diseases like depression, anxiety, and schizophrenia.
What happened to the raphe nuclei in epilepsy?
Vulnerability of the raphe nuclei in epilepsy
The raphe nuclei show vulnerability in epilepsy. Pentylenetetrazol (PTZ)-induced status epilepticus (SE) significantly increased the BBB permeability in rats at postnatal age 10 or 21 days [18]. The highest increasement of permeability happened in the raphe nuclei, the interpeduncular nucleus, and the trigeminal nerve tractus. In addition, volume loss was reported in patients with TLE in the mesencephalon encompassing the raphe nuclei [19]. In patients with TLE, the connectivities of ascending reticular activating system including connections from the DR and the MR to the limbic structures, thalamus, and certain neocortical areas were significantly lower than those in healthy controls [20]. These results all indicate vulnerability of the raphe nuclei and their diminished connections with other structures in epilepsy.
Neuronal activities of the raphe nuclei in epilepsy
The most direct evidence which proves the participation of the raphe nuclei in epilepsy is the seizure-induced change of neuronal activities in the raphe nuclei during epileptogenesis (Table 1). Researchers performed multi-unit and single-unit recordings in the medullary raphe and midbrain raphe in an established hippocampal seizure model in rats [21]. Multi-unit recording demonstrated that population firing of the neurons in the medullary raphe and midbrain raphe was markedly decreased during ictal and post-ictal period. Single-unit recording of the identified 5-HTergic neurons in the medullary raphe showed consistent decreased firing rate, but the firing of the midbrain raphe 5-HTergic neurons was complex including both increase and decrease. In rat amygdala rapid kindling model, the number of Fos-immunoreactive neurons in the RMg was also reduced after kindling [22]. It is believed that the decreased brainstem raphe neuronal activities may be associated with the simultaneously impaired cardiorespiratory function. However, the midbrain raphe may play a different role. In an experimental absence epilepsy, the spike and wave discharges (SWDs), which may be associated with the impairment of consciousness, propagated to the DR with a short delay as well as the firing rate of the DR neurons evidently increased throughout the whole paroxysm and returned to baseline levels afterwards [23]. Same situation occurred in mice hippocampal kindling seizures, in which the calcium activities of the DR 5-HTergic neurons were significantly increased [24]. In a word, most seizure activities can quickly spread to the raphe nuclei, but the neural activities of the raphe nuclei are interfered diversely in different types of epilepsy. Research on the neuronal activities of the midbrain raphe, specially the MR, in TLE is very limited, but the mixed activities of them are very interesting and worthy of future research.
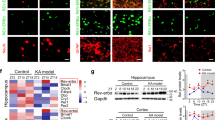
Epilepsy related alterations of the raphe 5-HTergic system
The 5-HTergic system is easily to be affected by epilepsy. The number of 5-HTergic neurons are also altered diversely in different subregions of the raphe (Table 1). In pilocarpine model of TLE, the number of tryptophan hydroxylase (TPH) positive neurons significantly decreased both in the DR and MR in rats 28 days after SE [25]. In kainic acid (KA) model of epilepsy, 5-HT-immunoreactive neurons were only reduced (approximately 35%) in the interfascicular part of the DR (DRI) but not in the other subregions of the raphe nuclei in rats 3 months after SE [26]. Similar results were discovered in another research with the same model, four months after SE, epileptic rats had approximately 30% less 5-HT-stained cells in the DRI, but had twice as many 5-HT-stained cells in the MR as the control rats [27]. In another study of pilocarpine model, the number of MR neurons which project to the CA3 increased 60 days after SE [28]. In summary, the number of 5-HTergic neurons in the DR was consistently decreased in different models of epilepsy and mostly happened in the DRI, while the number of MR 5-HTergic neurons was altered differently which may be associated with the different time point after SE, but the underlying mechanism of the increased number of 5-HT+ neurons in the MR has remained to be known.
The synthesis, release and transport of 5-HT are also influenced by epilepsy. For example, TPH-immunoreactivity in the medullary raphe was reduced in infantile spasm cases of perinatal hypoxic ischemic encephalopathy [29]. But the endogenous 5-HT level is altered differently in the acute and chronic stages of chronic epilepsy model. 5-HT level was dramatically increased in the hippocampus within the 30 min following pilocarpine induced SE, but reversed to basal level by 4 days after SE and continued to drop to 48% at 7 days and 28% of the basal level 14 days after SE [25]. Meanwhile, matched with the change curve of 5-HT levels, its main metabolite 5-hydroxyindoleacetic acid (5-HIAA) strikingly increased 2 days after SE, then gradually declined to levels below baseline. During the chronic period that 3 months after pilocarpine induced SE, 5-HT concentrations and turnover and 5-HT release in response to raphe stimulation were also decreased in the hippocampus in rats [30]. In Scn1a+/– mouse model of dravet syndrome, the endogenous 5-HT level in the midbrain raphe modestly decreased at an age before seizures appear, but back to normal as adults [31]. The SERT expression in the raphe is also altered diversely in different types of epilepsy. In seizure-naïve genetically epilepsy-prone (GEPR) rats, SERT expression in the raphe was reduced [32]. But in pilocarpine model of epilepsy, SERT expression was not altered in the raphe but only decreased in the hippocampus 4 weeks following SE in rats [33]. Meanwhile, four months after KA-induced SE, the areal density of the SERT-stained small-sized varicosities was decreased in the dentate gyrus (DG), infralimbic cortex (IL), and medial septum (MS), while that of the large-sized varicosities was increased in epileptic rats [27]. In general, the synthesis, release, and transport of 5-HT were attenuated in most epilepsy models, but altered differently in particular epilepsy period and particular brain regions.
In 5-HT receptor level, positron emission tomography (PET) imaging using the radioligand [18F]FCWAY, a 5-HT1a receptor antagonist, shows lower [18F]FCWAY volume of distribution in the raphe nuclei of TLE patients, which suggested reduced 5-HT1a receptor binding. Lower [18F]FCWAY volume of distribution was also found ipsilateral than contralateral to the epileptic focus in inferior medial and lateral temporal regions of patients [34]. In addition, reduced 5-HT1a receptors binding potential was discovered in the raphe nuclei, the epileptogenic hippocampus, amygdala and ipsilateral limbic cortex in TLE patients [35, 36]. Similarly, in juvenile myoclonic epilepsy which was classified as primarily generalized epilepsy, the binding potential of 5-HT1a receptors was reduced in the raphe nuclei, the dorsolateral prefrontal cortex and hippocampus [37]. However, in the supragranular layers of middle temporal gyrus, 5‐HT1a receptors were up-regulated in patients with pharmacoresistant focal TLE and their density correlated negatively with seizure frequency which might act as a compensatory mechanism through inhibiting glutamatergic neurotransmission [38]. Similarly, in amygdala-kindled rats, 5-HT1a receptor binding and mRNA expression were significantly increased in the dentate gyrus [39]. In addition to 5‐HT1a receptors, 5-HT2 receptors and 5-HT7 receptors were also implicated in epilepsy [40]. In the cerebral cortex, 5-HT2c receptor mRNA and binding potential were increased in epileptic rats of pilocarpine model [41]. In the hippocampus, 5-HT7 mRNA was significantly decreased in mice 40 min after the application of PTZ [42]. But in temporal neocortex of intractable epilepsy patients and epileptic rats of chronic pilocarpine model, 5-HT7 receptors expression was higher than in controls [43].
In general, the serotoninergic system is affected by epilepsy which gives rise to multifarious changes in the raphe serotoninergic system.
How do the raphe nuclei participate in epilepsy?
Genetic factors
Early in 1995, it was found that mutant mice lacking 5-HT2c receptor were prone to sudden death from seizure in Metrazol-induced epilepsy model [44]. Further researches discovered that lacking of 5-HT2c receptor resulted in the mice being extremely susceptible to audiogenic seizures in adulthood [45] and showing global increases in seizure susceptibility in olfactory bulb kindling model, corneal kindling model and flurothyl model of epilepsy [46]. Similarly, 5-HT1a receptor and 5-HT7 receptor deficient mice displayed generalized lower seizure threshold and higher lethality in various models of epilepsy [47, 48]. In addition, C allele of 5-HT1A C-1019G polymorphism acts as an independent risk factor for anxiety disorders in patients with TLE [49]. Lmx1bf/f/p mice, with genetically deleted nearly all the central 5-HTergic neurons, had a lower seizure threshold and increased mortality in maximal electroshock seizure and pilocarpine induced seizures, which can be partly rescued by pretreatment with 5-HT2a receptor agonist [50]. And male mice that lacking serotonin transporter were less vulnerable to PTZ-induced seizures than control mice, but this phenomenon did not exist in female SERT–/– mice [51]. In patients with TLE, polymorphisms of SERT gene, with 10-repear allele of 5-HTTVNTR, are associated with TLE susceptibility [52]. Mutations in SCN1A gene encoding the Nav1.1 sodium channel induced several models of epilepsy. In Scn1a+/– mouse model of dravet syndrome, the response to 5-HT1a receptors agonist was reduced before the age of seizure, but it became hypersensitive to both 5-HT1a and 5-HT2a/2c receptors agonists after the age of seizure development [31]. And systemic injection of 5-HT1d but not 5-HT2a/2c receptor agonist significantly ameliorated hyperthermia-induced seizure [53]. These studies all suggest that the 5-HTergic system is closely involved in the pathogenesis of epilepsy.
Lesion and transplant modulation
Early studies took neurochemical or electrolytic lesions to investigate the role of the raphe nuclei in epilepsy (Table 2). Electrolytic lesion of the midbrain raphe and system injections of p-chlorophenylalanine (pCPA), a 5-HT synthesis inhibitor, in rats enhanced the epileptiform activity in epilepsy induced by repeated electrical stimulation of the dorsal hippocampus [54]. Meanwhile, systemic injection of 5-hydroxytryptophan (5-HTP), which induced an increase of 5-HT synthesis and release, significantly reduced the epileptic susceptibility. Specific neurotoxins such as 5,6 or 5,7 dihydroxytryptamine (DHT) was used to destroy serotoninergic neurons. In pilocarpine model of epilepsy, a major number of 5,7-DHT pre-treated rats progressed to motor limbic seizures evolving to SE than the control rats, and the frequency of seizures significantly increased after the treatment of 5,7-DHT in the MR in the chronic period [55]. Either specific lesions of the midbrain raphe with DHT or specific lesions of serotoninergic terminals in the epileptic focus facilitated olfactory bulb kindling in rats [56]. Contrarily, transplantation of fetal raphe cells into the olfactory bulb of adult rats before kindling increased the afterdischarge threshold. Same results were got in genetically epilepsy-prone rats (GEPR-3s) that microinjection of 5,7-DHT into the lateral ventricle increased seizure severity and subsequent reduced seizure severity as a result of transplantation of fetal raphe cells [57, 58]. In conclusion, electrolytic lesion of the raphe nuclei or chemical lesion of the 5-HTergic system significantly elevated the severity of epilepsy, indicating that the intrinsic 5-HTergic system may function as a protective mechanism.
Brain stimulation modulation
Vagal nerve stimulation (VNS) has been approved by the Food and Drug Administration for treatment of refractory epilepsy and refractory depression. But the mechanisms that VNS produces its beneficial clinical effects are still unknown. Several studies found that chronic VNS has effects on the central 5-HTergic activity. In conscious rats, VNS with clinical parameters (one burst of 20 Hz, 250 μs pulse width, 0.25 mA stimulation for 30 s every 5 min) for 3 weeks significantly increased DeltaFosB and c-Fos staining in the DR, whereas acute VNS for 2 h had no effect [59]. Electrophysiological recordings showed that chronic VNS with the parameter (0.25 mA, 20 Hz, 500 µs, 30 s ON/5 min OFF) produced an optimal activation of 5-HT neurons in the DR [60]. In addition, less stimulation (30-s stimulation every 10 or 15 min) is sufficient to achieve the same VNS efficacy on 5-HT neuronal firing [61]. In conclusion, chronic VNS activated the raphe 5-HT neurons. Furthermore, long-term VNS also produced tonic activation of postsynaptic 5-HT1a receptors in the hippocampus and increased extracellular 5-HT levels in the dorsal raphe [62, 63]. It indicates that the therapeutic effect of the VNS may be partly mediated by modulating the brain 5-HTergic system.
Deep brain stimulation (DBS) has becoming an alternative and effective therapy for chronic brain disease, such as refractory epilepsy and major depressive disorder (MDD). Electrical stimulation of the raphe nuclei promotes the release of 5-HT in the brain, while central serotonergic activity is associated with cortical and subcortical neural excitability. Electrical stimulation of the raphe nuclei for 20 min (1200 square-wave pulses, 100 mA, 1 ms duration, and 1 Hz) or subcutaneous injection of SSRI decreased cortical spreading depression (CSD) and increased duration of the negative DC-shift of CSD, whereas low-tryptophan diet significantly accelerated CSD propagation and shortened DC-shift of CSD in male Wistar rats [64]. These results indicated that central serotonergic activity negatively modulated CSD propagation in the rat cortex. Raphe stimulation has also been proved to inhibit epilepsy in experimental models. Pre-stimulation of the MR for 1 h (8–10 pulse/s, 1 ms duration, 0.2–0.24 mA) and maintenance for 5 min after seizure induction significantly inhibited convulsions in Metrazol model and amygdala kindling model of epilepsy as compared to those stimulation of non-raphe areas of the midbrain in rats [65]. In epilepsy induced by locally applied sodium penicillin in hippocampus, stimulation of the MR (0.5–0.1 ms duration, 5–30 Hz, 0.1–0.7 mA, 5–30 s train duration) also decreased hippocampal spike frequency in cats [66]. Intra-MR muscimol, a GABA receptor agonist, enhanced hippocampal-based epilepsy. After muscimol, MR stimulation at the same threshold parameters failed to affect hippocampal activity. They also found a disinhibitory habenlo-raphe-hippocampal circuit in epilepsy [67]. In a word, current studies show that DBS of the raphe nuclei generally has anti-epileptic effects, but the optimal parameter of DBS is unknown and to what degree the 5-HTergic system is involved still needs more investigations. Besides, these above non-specific modulations, including lesion and DBS approaches, may also affect other neural systems.
Pharmacological modulation
A number of pharmacological studies investigated the role of 5-HTergic system in clinical epilepsy and experimental model of epilepsy [68, 69]. Most of the them found that enhancing the level of 5-HT in the brain had an anti-seizure effect, but exceptions that had no effect or proconvulsant effect in some cases were not uncommon (Table 3). These results suggest that the central 5-HTergic system is complicated and more specific researches about functions of 5-HTergic neurons need to be done. However, region-specific studies about functions of 5-HTergic neurons in different subregions of the raphe nuclei are limited. Only one study found that implants RMg with Progesretone P(4) or its metabolite in female Long-Evans rats significantly reduced the incidence of myoclonic seizures and EEG activity after PTZ administration in rats, but the participation of 5-HTergic system in this function is unknown [70]. Limbic systems like the hippocampus and entorhinal cortex (EC) receive a high density of fibers originating from the raphe nuclei. Serotonin (100 μM) application induced 5-HT1a-receptor-mediated hyperpolarization and decrease of input resistance of granular neurons in the dentate gyrus both in control and pilocarpine-treated Wistar rats [40]. Application of 5-HT in the brain slice of female Wistar rats has predominately inhibitory effects on epileptiform activity in the subiculum induced by lowering of Mg2+, but in some cases also has disinhibitory effect at higher concentrations [71]. Electrophysiological results showed that 5-HT2c receptors reduced bursting activity of principal cells of the subiculum by inhibiting a T-type Ca2+ channels mediated low-threshold calcium current. Activation of this pathway decreased bursting activity and the occurrence of epileptiform discharges in slices from the hippocampus of pilocarpine treated chronic epileptic rats [72]. In the EC, application of fenfluramine (FFA), a 5-HT-releasing drug, reversibly blocked epileptiform activity in an in vitro model of epilepsy in Wistar rats [73]. Coapplication of the 5-HT1a receptor antagonist WAY-100635 prevented the FFA-induced anticonvulsive effect. Further studies found that focal application of 5-HT increased the frequency and amplitude of spontaneous inhibitory postsynaptic current (sIPSC) of principal neurons in the EC via activation of 5-HT2a receptor [74]. It can also generate membrane depolarization and increase the action potential frequency of GABAergic interneurons in the EC, which can be reversed by inhibiting TASK-3 K+ channel or 5-HT2a receptor antagonist. While, in frontal cortex, 5-HT produces multiple effects on epileptiform activity in rat cortical slices via activation of different 5-HT receptor subtypes. The excitatory action of 5-HT is predominately mediated by 5-HT2 receptors and the inhibitory effects can be attributed to the activation of 5-HT1a and 5-HT1b receptors [75]. In conclusion, application of 5-HT in the limbic system regulates the balance of excitation and inhibition that has a mainly anticonvulsive but also proconvulsive function, which may be mediated by different 5-HT receptors in different downstream circuits.
Optogenetic modulation
Optogenetics enables optical control of membrane potential through transducing microbial opsin genes to get modulation of specific neural populations or circuits in freely moving animals. It takes the advantages of high temporal versatility and cellular specificity. As we mentioned above, the raphe nuclei contain various types of neurons, and studies with method of lesion or electrostimulation interventions are unable to selectively modulate the 5-HTergic systems in specific subregions of the raphe nuclei, which can be solved by optogenetics but relevant optogenetic studies are very limited. In a DBA/1 mouse model and PTZ model, photostimulation of DR 5-HTergic neurons in DBA/1 TPH2-ChR2 mice suppressed tonic seizures in most mice, but had no effect on clonic seizures [76]. However, in another mouse hippocampal kindling model of our research which was considered as a type of clonic seizures of TLE, we found that activities of DR 5-HTergic neurons were markedly increased during hippocampal seizures, and time-aligned inhibition of hyperactivity of DR 5-HTergic neurons with method of either optogenetic inhibition of DR 5-HTergic neurons or 1-Hz DR DBS significantly retarded the acquisition of kindling seizures [24]. These researches indicated that DR 5-HTergic neurons may play different roles in different types of epilepsy and functions of other subregions of the raphe nuclei remain to be investigated.
The raphe nuclei in comorbidities of epilepsy
The raphe nuclei in epilepsy associated depression
Mood disorder and major depression are frequently comorbid with epilepsy (Table 4). In patients with idiopathic generalized epilepsy with tonic-clonic seizures (IGE-TCS) and depression, patients with hypoechogenic brainstem raphe had significantly higher score of Chinese version Neurological Disorders Depression Inventory for Epilepsy (C-NDDI-E) and Beck Depression Inventory-II (BDI-II), and most patients with IGE-TCS and depression exhibited hypoechogenic brainstem raphe, but few patients with IGE-TCS without depression exhibited hypoechogenic brainstem raphe [77]. Furthermore, epileptic patients with hypoechogenicity in the brainstem raphe had higher epileptic discharge index during sleep period but not during awake period, indicating the modulation of the brainstem raphe in epileptic discharge during the sleep cycle [78]. In TLE patients, the BDI score positively correlated with the binding potential of [18F]MPPF, a 5-HT1a antagonist, in the raphe nuclei and in the insula contralateral to seizure onset, whereas somatic symptoms positively correlated with the [18F]MPPF binding potential in the ipsilateral hippocampus and bilateral left mid-cingulate gyrus and the inferior dorsolateral frontal cortex [79]. In most animal models of epilepsy, especially in chronic models like pilocarpine model and KA model, epileptic animals exhibited increase in immobility time under conditions of forced swim test which was indicative of despair-like state, and loss of taste preference in saccharin solution consumption test which pointed to the symptomatic equivalence of anhedonia [26, 30]. Fast scan cyclic voltammetry (FSCV) of serotonergic raphe nucleus (RN)-prefrontal cortex (PFC) pathways and dopaminergic ventral tegmental area (VTA)-nucleus accumbens (NAcc) pathways showed that animals with preexisting deviations in RN-PFC invariably developed despair two months after pilocarpine SE and rats with deviations in VTA-NAcc developed anhedonia [80]. It is suggested that epilepsy triggers decompensations in the already vulnerable depression-relevant neuronal circuits, which culminate in depression.
Pharmacological studies partly reveal the mechanism of depression associated with epilepsy. Intra-raphe injection of M40, a galanin receptor type 1 (GalR1)/type 2 (GalR2) antagonist, improved depressive-like behavior in epileptic “depressed” rats, while intra-raphe administration of M871, a preferential GalR2 antagonist, exacerbated depressive-like behavior [81]. In post-SE rats, depression-like impairments also included the hyperactivity of the hypothalamo-pituitary-adrenocortical axis; the diminished raphe-hippocampus 5-HTergic system; and the upregulation of presynaptic 5-HT1a receptors [82]. Pharmacological activation of postsynaptic 5-HT1a receptors in the hippocampus improved depressive deficits in epileptic rats. However, administration of fluoxetine (20 mg· kg−1 ·d−1 for 10 days) significantly shortened immobility time under condition of forced swim test in naïve animals, but did not improve performance in post-SE rats [30]. The drug-resistant depression-like behavior suggested that depression in epilepsy may have distinct underlying mechanisms. Two-week long bilateral intrahippocampal infusion of human recombinant Interleukin-1 receptor antagonist (IL-1ra) improved all of the depressive impairments, without modifying spontaneous seizure frequency and without affecting normal parameters in naïve rats [83]. Combined administration of fluoxetine and IL-1ra completely abolished all hallmarks of epilepsy-associated depressive abnormalities, which implicated that the resistance to SSRI was partly driven by the interleukin-1β signaling [84]. Besides, coadministration of fluoxetine and reboxetine, a norepinephrine reuptake inhibitor (NERI), fully reversed depressive-like behavior in epilepsy [85]. In conclusion, the mechanism underlying the depression in epilepsy may be associated not only with dysregulation of the raphe 5-HTergic systems, but also with alteration of hippocampal 5-HTergic signaling and interleukin-1β signaling and central norepinephrinergic systems.
The raphe nuclei in SUDEP
Sudden unexpected death in epilepsy often happened immediately after a tonic-clonic seizure with potential mechanisms of seizure-induced respiratory depression, cardiac arrhythmia, cerebral depression, and autonomic dysfunction [86] (Table 4). In SUDEP cases, volume loss of the brain was very serious [19]. In particular, volume loss in the raphe nuclei was highly correlated with the time between last MRI and SUDEP which means that brainstem atrophy which expands into the raphe can increase the risk for SUDEP [87]. In the medullary raphe of SUDEP patients, there was significantly less c-fos expression than in non-epilepsy controls [88]. Besides, TPH and SERT expression in the raphe were reduced in cases of SUDEP [89]. Moreover, Cx43 glia, which is considered essential for normal respiratory regulation, was reduced in the MR in SUDEP cases [90]. These clinical researches all indicates the participation of the raphe nuclei and their 5-HTergic system in SUDEP. What about the animal model of SUDEP? For example, amygdala kindling seizure can result in respiratory physiology impairment in rats [22]. Optogenetic activation of DR 5-HTergic neurons reduced the duration of post-ictal generalized EEG suppression following seizures in kindled Pet1-Cre mice, thus reducing the risk of SUDEP [91]. But the classic animal model of SUDEP is the DBA mouse model, a model that acoustically evoked generalized seizures leads to seizure-induced respiratory arrest (S-IRA) and results in SUDEP unless resuscitation is rapidly instituted. Manganese-enhanced magnetic resonance imaging (MEMRI) data in male DBA/1 mouse brain showed significantly increased activity in the RMg, RPa and CLi but not in the DR, the MR and the ROb immediately after acoustically-induced S-IRA [92]. The increased activities at certain raphe nuclei were supposed to be compensatory mechanisms for apnea but were not sufficient to prevent death. In the brainstem tissue of DBA/2 mice, 5-HT2c, 5-HT3, and 5-HT4 receptors expressions were significantly diminished, while the 5-HT2b receptors expression was significantly elevated [93]. Photostimulation of DR 5-HTergic neurons in DBA/1 TPH2-ChR2 mice significantly reduced the incidence of S-IRA, and the S-IRA-suppressing effect of photostimulation was increased by 5-HTP and was reversed by specific 5-HT3 receptor antagonist [76]. In general, it seems that the medullary raphe has a close relationship with SUDEP, but the midbrain raphe may also play a role in it. However, their cellular and circuit mechanisms underlying SUDEP are worth for further research.
The raphe nuclei in other comorbidities of epilepsy
The raphe nuclei are reported to be associated with many other brain dysfunctions in epilepsy such as pain, attention deficit/hyperactivity (ADHD), impulsive-like behavior, autism like behavior, cognition and memory deficit and sleep deficit [85, 94, 95]. Among them, studies about the raphe nuclei in pain and epilepsy are the most (Table 4). Noxious stimulation suppressed epileptic seizures in humans and epileptiform activities in experimental animal models. Intravenous injection of 8-hydroxydipropylaminotetralin (DPAT), imipramine, and fluoxetine, drugs known to depress dorsal raphe unit activity, prevented suppression of focal epileptiform activity induced by noxious stimulation in penicillin model of epilepsy in SD rats [96]. Quipazine, an agonist at 5-HT receptors, in part restored the suppression that had been blocked by DPAT or imipramine. Several serotonin antagonists effective at 5-HT1 and 5-HT2 receptors blocked this suppression. Furthermore, pressure ejection in the vicinity of the DR with 5-HT, DPAT, fluoxetine and baclofen prevented cortical desynchronization as well as the suppression of focal epileptiform activity in the same model of epilepsy [97]. Moreover, the DR is also implicated in the postictal antinociception. Neurochemical lesion of the DR induced a significant decrease of the postictal analgesia and pre-treatment of the DR with atropine or mecamylamine decreased the postictal antinociceptive phenomenon in PTZ model in male Wistar rats [98, 99]. Additional evidence demonstrated the recruitment of 5-HT1a/1b, 5-HT2a/2c, 5-HT6, and 5-HT7 receptors of the DR [100, 101], in addition to 5-HT2 receptor of the RMg [102], in the postictal antinociception. In conclusion, the DR may underlie the clinical effectiveness of noxious stimuli in suppressing epileptic seizures and the postictal antinociceptive process.
Further perspectives on the raphe nuclei in epilepsy
In summary, the raphe nuclei and 5-HTergic system indeed are closely implicated in epilepsy and associated comorbidities. But there are still many questions remain to be answered.
How does the seizure propagate to the raphe nuclei?
Neuronal firing, immediate-early genes expression and MRI activities indicate that the raphe nuclei participate in the epilepsy network directly. But the seizure pathway propagating from the seizure focus to the raphe nuclei is still unknown. Retrograde viral tracing found that the DR and the MR 5-HT neurons receive dense projections from the somatomotor cortex, amygdala and relatively sparse projections from the thalamus, hypothalamus, midbrain reticular nucleus [6]. Early studies also found that large numbers of neurons in the frontal cortex, dorsomedial nucleus of the hypothalamus, zona incerta, periaqueductal gray and deep layers of the superior colliculus project to the RMg [103]. It is very likely that seizure propagate from these nuclei to the raphe nuclei but the direct evidence is lacking. Further studies could use circuit-specific-labeled virus combined with calcium imaging and optogenetic regulation to investigate the precise circuit basis from seizure focus to the raphe nuclei.
What are the roles of different subregions of the raphe nuclei in different types of epilepsy?
The raphe nuclei are comprised of the rostral group and the caudal group. The rostral group including the DR and the MR and their forebrain projections are implicated in various models of epilepsy. Intervention studies revealed that these two subregions are particularly implicated in the frequency and duration of the epileptiform activities. Meanwhile, the caudal group also named the medullary raphe are generally regarded to have a function in the SUDEP. Most studies found alterations of the medullary raphe in SUDEP but direct interventional evidence is still lacking. Instead, optogenetic activation of the DR 5-HT neurons significantly alleviated the S-IRA in DBA/1 mouse model of SUDEP. How do the DR participate in respiratory control? Anterograde tracing found that the 5-HT neurons in the DR and the MR have dense projections to the medulla, which may in part explain the role of DR in SUDEP. Since the MR also has dense projections to the medulla, does the MR also have a role in the SUDEP? These questions suggest that more investigations of the exact role of different subregions of the raphe nuclei in different types of epilepsy should be undertaken in the future.
What are the downstream circuits underlying the divergent roles of the raphe nuclei in epilepsy and neural excitability?
Intervention studies found that lesion or pharmacological inhibition of the raphe 5-HTergic systems significantly elevate the severity of seizure, while pharmacological or optogenetic activation of the raphe 5-HTergic systems remarkably inhibit epileptiform activity. But what downstream that the raphe 5-HTergic system modulation influences seizure activity is still largely unknown. System applications of SSRIs have inconsistent effects on different models of epilepsy. However, electrophysiological studies in vitro partly demonstrated that serotonin application in the frontal cortex and limbic systems including the hippocampus and the EC predominately inhibits the epileptiform activity associated with 5-HT1a, 5-HT1b, 5-HT2a, 5-HT2c and 5-HT3 receptors. In addition, systemic application of fluoxetine also had no effect on depression in epilepsy, but activation of postsynaptic 5-HT1a receptors in the hippocampus partly alleviated the depression-like behavior in epilepsy. These results indicated that the 5-HTergic system is complicated and different downstream organizations of the raphe 5-HTergic systems may play different roles through various receptors. Besides, even being the same receptor, it may have opposite function in local neural excitability. For example, activation of 5-HT1a receptor induced hyperpolarization of pyramidal neurons in the dorsal CA1, but increased pyramidal neurons firing in the prefrontal cortex by preferentially inhibiting GABAergic interneurons. Let alone there are 14 kinds of 5-HT receptors with diverse functions in the downstream neural excitability. Therefore, circuit level modulation of the raphe 5-HTergic system should be undertaken in epilepsy and comorbidities by the means of circuit-specific optogenetic and chemogenetic strategies combined with transgenic mice. Furthermore, single cell RNA sequence could help to find circuit-specific molecules which are beneficial for the development for targeting drugs in the future. And clarification of diversities of the raphe 5-HTergic systems, like functions of these circuit-specific molecules and functions of specific 5-HT receptors in specific brain regions, would accelerate the development of 5-HTergic drugs that provide therapeutic help for not only the epilepsy but also many other brain disorders associated with abnormal neural excitability.
References
Wang Y, Chen Z. An update for epilepsy research and antiepileptic drug development: Toward precise circuit therapy. Pharmacol Ther. 2019;201:77–93.
Arana A, Wentworth CE, Ayuso-Mateos JL, Arellano FM. Suicide-related events in patients treated with antiepileptic drugs. N Engl J Med. 2010;363:542–51.
Hornung JP. The human raphe nuclei and the serotonergic system. J Chem Neuroanat. 2003;26:331–43.
Kawashima T, Zwart MF, Yang CT, Mensh BD, Ahrens MB. The serotonergic system tracks the outcomes of actions to mediate short-term motor learning. Cell. 2016;167:933–46 e20.
Andalman AS, Burns VM, Lovett-Barron M, Broxton M, Poole B, Yang SJ, et al. Neuronal dynamics regulating brain and behavioral state transitions. Cell. 2019;177:970–85 e20.
Pollak Dorocic I, Furth D, Xuan Y, Johansson Y, Pozzi L, Silberberg G, et al. A whole-brain atlas of inputs to serotonergic neurons of the dorsal and median raphe nuclei. Neuron. 2014;83:663–78.
Commons KG. Ascending serotonin neuron diversity under two umbrellas. Brain Struct Funct. 2016;221:3347–60.
Brust RD, Corcoran AE, Richerson GB, Nattie E, Dymecki SM. Functional and developmental identification of a molecular subtype of brain serotonergic neuron specialized to regulate breathing dynamics. Cell Rep. 2014;9:2152–65.
Mason P. Contributions of the medullary raphe and ventromedial reticular region to pain modulation and other homeostatic functions. Annu Rev Neurosci. 2001;24:737–77.
Sos KE, Mayer MI, Cserep C, Takacs FS, Szonyi A, Freund TF, et al. Cellular architecture and transmitter phenotypes of neurons of the mouse median raphe region. Brain Struct Funct. 2017;222:287–99.
Millan MJ, Marin P, Bockaert J, Mannoury la Cour C. Signaling at G-protein-coupled serotonin receptors: recent advances and future research directions. Trends Pharmacol Sci. 2008;29:454–64.
Varga V, Losonczy A, Zemelman BV, Borhegyi Z, Nyiri G, Domonkos A, et al. Fast synaptic subcortical control of hippocampal circuits. Science. 2009;326:449–53.
Teixeira CM, Rosen ZB, Suri D, Sun Q, Hersh M, Sargin D, et al. Hippocampal 5-HT input regulates memory formation and schaffer collateral excitation. Neuron. 2018;98:992–1004 e4.
Llado-Pelfort L, Santana N, Ghisi V, Artigas F, Celada P. 5-HT1A receptor agonists enhance pyramidal cell firing in prefrontal cortex through a preferential action on GABA interneurons. Cereb Cortex. 2012;22:1487–97.
Stanford IM, Kantaria MA, Chahal HS, Loucif KC, Wilson CL. 5-Hydroxytryptamine induced excitation and inhibition in the subthalamic nucleus: action at 5-HT(2C), 5-HT(4) and 5-HT(1A) receptors. Neuropharmacology. 2005;49:1228–34.
Bortolozzi A, Diaz-Mataix L, Scorza MC, Celada P, Artigas F. The activation of 5-HT receptors in prefrontal cortex enhances dopaminergic activity. J Neurochem. 2005;95:1597–607.
Okaty BW, Commons KG, Dymecki SM. Embracing diversity in the 5-HT neuronal system. Nat Rev Neurosci. 2019;20:397–424.
Padou V, Boyet S, Nehlig A. Changes in transport of [14C] alpha-aminoisobutyric acid across the blood-brain barrier during pentylenetetrazol-induced status epilepticus in the immature rat. Epilepsy Res. 1995;22:175–83.
Mueller SG, Bateman LM, Laxer KD. Evidence for brainstem network disruption in temporal lobe epilepsy and sudden unexplained death in epilepsy. Neuroimage Clin. 2014;5:208–16.
Englot DJ, D’Haese P-F, Konrad PE, Jacobs ML, Gore JC, Abou-Khalil BW, et al. Functional connectivity disturbances of the ascending reticular activating system in temporal lobe epilepsy. J Neurol Neurosurg Psychiatry. 2017;88:925–32.
Zhan Q, Buchanan GF, Motelow JE, Andrews J, Vitkovskiy P, Chen WC, et al. Impaired serotonergic brainstem function during and after seizures. J Neurosci. 2016;36:2711–22.
Totola LT, Malheiros-Lima MR, Delfino-Pereira P, Del Vecchio F, Souza FC, Takakura AC, et al. Amygdala rapid kindling impairs breathing in response to chemoreflex activation. Brain Res. 2019;1718:159–68.
Lörincz M, Oláh M, Baracskay P, Szilágyi N, Juhász G. Propagation of spike and wave activity to the medial prefrontal cortex and dorsal raphe nucleus of WAG/Rij rats. Physiol Behav. 2007;90:318–24.
Cheng H, Qi Y, Lai N, Yang L, Xu C, Wang S, et al. Inhibition of hyperactivity of the dorsal raphe 5-HTergic neurons ameliorates hippocampal seizure. CNS Neurosci Ther. 2021;27:963–72.
Lin WH, Huang HP, Lin MX, Chen SG, Lv XC, Che CH, et al. Seizure-induced 5-HT release and chronic impairment of serotonergic function in rats. Neurosci Lett. 2013;534:1–6.
Maia GH, Soares JI, Andrade PA, Leite JF, Luz LL, Andrade JP, et al. Altered taste preference and loss of limbic-projecting serotonergic neurons in the dorsal raphe nucleus of chronically epileptic rats. Behav Brain Res. 2016;297:28–36.
Maia GH, Soares JI, Almeida SG, Leite JM, Baptista HX, Lukoyanova AN, et al. Altered serotonin innervation in the rat epileptic brain. Brain Res Bull. 2019;152:95–106.
Ma DL, Tang YC, Chen PM, Chia SC, Jiang FL, Burgunder JM, et al. Reorganization of CA3 area of the mouse hippocampus after pilocarpine induced temporal lobe epilepsy with special reference to the CA3-septum pathway. J Neurosci Res. 2006;83:318–31.
Hayashi M, Itoh M, Araki S, Kumada S, Tanuma N, Kohji T, et al. Immunohistochemical analysis of brainstem lesions in infantile spasms. Neuropathology. 2000;20:297–303.
Mazarati A, Siddarth P, Baldwin RA, Shin D, Caplan R, Sankar R. Depression after status epilepticus: behavioural and biochemical deficits and effects of fluoxetine. Brain. 2008;131:2071–83.
Hatini PG, Commons KG. Serotonin abnormalities in Dravet syndrome mice before and after the age of seizure onset. Brain Res. 2019;1724:146399.
Szot P, Reigel CE, White SS, Veith RC. Alterations in mRNA expression of systems that regulate neurotransmitter synaptic content in seizure-naive genetically epilepsy-prone rat (GEPR): transporter proteins and rate-limiting synthesizing enzymes for norepinephrine, dopamine and serotonin. Brain Res Mol Brain Res. 1996;43:233–45.
Lin WH, Li XF, Lin MX, Zhou Y, Huang HP. Novel insights into the effect of paroxetine administration in pilocarpine‑induced chronic epileptic rats. Mol Med Rep. 2017;16:8245–52.
Toczek MT, Carson RE, Lang L, Ma Y, Spanaki MV, Der MG, et al. PET imaging of 5-HT1A receptor binding in patients with temporal lobe epilepsy. Neurology. 2003;60:749–56.
Savic I, Lindström P, Gulyás B, Halldin C, Andrée B, Farde L. Limbic reductions of 5-HT1A receptor binding in human temporal lobe epilepsy. Neurology. 2004;62:1343–51.
Giovacchini G, Toczek MT, Bonwetsch R, Bagic A, Lang L, Fraser C, et al. 5-HT 1A receptors are reduced in temporal lobe epilepsy after partial-volume correction. J Nucl Med. 2005;46:1128–35.
Meschaks A, Lindstrom P, Halldin C, Farde L, Savic I. Regional reductions in serotonin 1A receptor binding in juvenile myoclonic epilepsy. Arch Neurol. 2005;62:946–50.
Palomero-Gallagher N, Schleicher A, Bidmon HJ, Pannek HW, Hans V, Gorji A, et al. Multireceptor analysis in human neocortex reveals complex alterations of receptor ligand binding in focal epilepsies. Epilepsia. 2012;53:1987–97.
Kalynchuk LE, Pinel JP, Meaney MJ. Serotonin receptor binding and mRNA expression in the hippocampus of fearful amygdala-kindled rats. Neurosci Lett. 2006;396:38–43.
Gilling KE, Oltmanns F, Behr J. Impaired maturation of serotonergic function in the dentate gyrus associated with epilepsy. Neurobiol Dis. 2013;50:86–95.
Krishnakumar A, Anju TR, Abraham PM, Paulose CS. Alteration in 5-HT(2)C, NMDA receptor and IP3 in cerebral cortex of epileptic rats: restorative role of Bacopa monnieri. Neurochem Res. 2015;40:216–25.
Arbabi Jahan A, Rad A, Ghanbarabadi M, Amin B, Mohammad-Zadeh M. The role of serotonin and its receptors on the anticonvulsant effect of curcumin in pentylenetetrazol-induced seizures. Life Sci. 2018;211:252–60.
Yang Z, Liu X, Yin Y, Sun S, Deng X. Involvement of 5-HT(7) receptors in the pathogenesis of temporal lobe epilepsy. Eur J Pharmacol. 2012;685:52–8.
Tecott LH, Sun LM, Akana SF, Strack AM, Lowenstein DH, Dallman MF, et al. Eating disorder and epilepsy in mice lacking 5-HT2c serotonin receptors. Nature. 1995;374:542–6.
Brennan TJ, Seeley WW, Kilgard M, Schreiner CE, Tecott LH. Sound-induced seizures in serotonin 5-HT2c receptor mutant mice. Nat Genet. 1997;16:387–90.
Applegate CD, Tecott LH. Global increases in seizure susceptibility in mice lacking 5-HT2C receptors: a behavioral analysis. Exp Neurol. 1998;154:522–30.
Sarnyai Z, Sibille EL, Pavlides C, Fenster RJ, McEwen BS, Toth M. Impaired hippocampal-dependent learning and functional abnormalities in the hippocampus in mice lacking serotonin(1A) receptors. Proc Natl Acad Sci USA. 2000;97:14731–6.
Witkin JM, Baez M, Yu J, Barton ME, Shannon HE. Constitutive deletion of the serotonin-7 (5-HT(7)) receptor decreases electrical and chemical seizure thresholds. Epilepsy Res. 2007;75:39–45.
Schenkel LC, Bragatti JA, Becker JA, Torres CM, Martin KC, de Souza AC, et al. Serotonin gene polymorphisms and psychiatry comorbidities in temporal lobe epilepsy. Epilepsy Res. 2012;99:260–6.
Buchanan GF, Murray NM, Hajek MA, Richerson GB. Serotonin neurones have anti-convulsant effects and reduce seizure-induced mortality. J Physiol. 2014;592:4395–410.
Fox MA, Andrews AM, Wendland JR, Lesch KP, Holmes A, Murphy DL. A pharmacological analysis of mice with a targeted disruption of the serotonin transporter. Psychopharmacology. 2007;195:147–66.
Li J, Lin H, Zhu X, Li L, Wang X, Sun W, et al. Association study of functional polymorphisms in serotonin transporter gene with temporal lobe epilepsy in Han Chinese population. Eur J Neurol. 2012;19:351–3.
Hatini PG, Commons KG. A 5-HT1D -receptor agonist protects Dravet syndrome mice from seizure and early death. Eur J Neurosci. 2020;52:4370–4.
Cavalheiro EA, Elisabetsky E, Campos CJ. Effect of brain serotonin level on induced hippocampal paroxysmal activity in rats. Pharmacol Biochem Behav. 1981;15:363–6.
Trindade-Filho EM, de Castro-Neto EF, de A, Carvalho R, Lima E, Scorza FA, et al. Serotonin depletion effects on the pilocarpine model of epilepsy. Epilepsy Res. 2008;82:194–9.
Lerner-Natoli M. Serotonin and kindling development. Int J Neurosci. 1987;36:139–51.
Clough R, Statnick M, Maring-Smith M, Wang C, Eells J, Browning R, et al. Fetal raphe transplants reduce seizure severity in serotonin-depleted GEPRs. Neuroreport. 1996;8:341–6.
Statnick MA, Maring-Smith ML, Clough RW, Wang C, Dailey JW, Jobe PC, et al. Effect of 5,7-dihydroxytryptamine on audiogenic seizures in genetically epilepsy-prone rats. Life Sci. 1996;59:1763–71.
Cunningham JT, Mifflin SW, Gould GG, Frazer A. Induction of c-Fos and DeltaFosB immunoreactivity in rat brain by Vagal nerve stimulation. Neuropsychopharmacology. 2008;33:1884–95.
Manta S, Dong J, Debonnel G, Blier P. Optimization of vagus nerve stimulation parameters using the firing activity of serotonin neurons in the rat dorsal raphe. Eur Neuropsychopharmacol. 2009;19:250–5.
Manta S, El Mansari M, Blier P. Novel attempts to optimize vagus nerve stimulation parameters on serotonin neuronal firing activity in the rat brain. Brain Stimul. 2012;5:422–9.
Manta S, Dong J, Debonnel G, Blier P. Enhancement of the function of rat serotonin and norepinephrine neurons by sustained vagus nerve stimulation. J Psychiatry Neurosci. 2009;34:272–80.
Manta S, El Mansari M, Debonnel G, Blier P. Electrophysiological and neurochemical effects of long-term vagus nerve stimulation on the rat monoaminergic systems. Int J Neuropsychopharmacol. 2013;16:459–70.
Guedes RCA, Araújo MDGRD, Verçosa TC, Bion FM, de Sá AL, Pereira A, et al. Evidence of an inverse correlation between serotonergic activity and spreading depression propagation in the rat cortex. Brain Res. 2017;1672:29–34.
Kovacs DA, Zoll JG. Seizure inhibition by median raphe nucleus stimulation in rat. Brain Res. 1974;70:165–9.
Sabatino M, Ferraro G, La Grutta V. Relay stations and neurotransmitters between the pallidal region and the hippocampus. Electroencephalogr Clin Neurophysiol. 1991;78:302–10.
Michele S, Vella N, Ferraro G, Gravante G, La Grutta V. Neurotransmitters involved in the habenular control of raphe-hippocampal circuit. Pharmacol Res. 1989;21:39–40. Suppl 1
Alhaj MW, Zaitone SA, Moustafa YM. Fluvoxamine alleviates seizure activity and downregulates hippocampal GAP-43 expression in pentylenetetrazole-kindled mice: role of 5-HT3 receptors. Behav Pharmacol. 2015;26:369–82.
Kanner AM. Most antidepressant drugs are safe for patients with epilepsy at therapeutic doses: A review of the evidence. Epilepsy Behav. 2016;61:282–6.
Frye CA, Muscatiello NA. 3alpha,5alpha-THP in the raphe magnus attenuates PTZ-induced myoclonic seizures. Brain Res. 2001;911:146–51.
Behr J, Heinemann U. Effects of serotonin on different patterns of low Mg2+-induced epileptiform activity in the subiculum of rats studied in vitro. Brain Res. 1996;737:331–4.
Petersen AV, Jensen CS, Crépel V, Falkerslev M, Perrier J-F. Serotonin regulates the firing of principal cells of the subiculum by inhibiting a T-type Ca current. Front Cell Neurosci. 2017;11:60.
Gentsch K, Heinemann U, Schmitz B, Behr J. Fenfluramine blocks low-Mg2+-induced epileptiform activity in rat entorhinal cortex. Epilepsia. 2000;41:925–8.
Deng PY, Lei S. Serotonin increases GABA release in rat entorhinal cortex by inhibiting interneuron TASK-3 K+ channels. Mol Cell Neurosci. 2008;39:273–84.
Bobula B, Zahorodna A, Bijak M. Different receptor subtypes are involved in the serotonin-induced modulation of epileptiform activity in rat frontal cortex in vitro. J Physiol Pharmacol. 2001;52:265–74.
Zhang H, Zhao H, Zeng C, Van Dort C, Faingold CL, Taylor NE, et al. Optogenetic activation of 5-HT neurons in the dorsal raphe suppresses seizure-induced respiratory arrest and produces anticonvulsant effect in the DBA/1 mouse SUDEP model. Neurobiol Dis. 2018;110:47–58.
Tao W-W, Cai X-T, Shen J, Shi X-G, Wang Y. Hypoechogenicity of brainstem raphe correlates with depression in migraine patients. J Headache Pain. 2019;20:53.
Li HL, Deng ZR, Zhang J, Ding CH, Shi XG, Wang L, et al. Sonographic hypoechogenicity of brainstem raphe nucleus is correlated with electroencephalographic spike frequency in patients with epilepsy. Epilepsy Behav. 2021;117:107884.
Lothe A, Didelot A, Hammers A, Costes N, Saoud M, Gilliam F, et al. Comorbidity between temporal lobe epilepsy and depression: a [18F]MPPF PET study. Brain. 2008;131:2765–82.
Medel-Matus JS, Shin D, Sankar R, Mazarati A. Inherent vulnerabilities in monoaminergic pathways predict the emergence of depressive impairments in an animal model of chronic epilepsy. Epilepsia. 2017;58:e116–e21.
Medel-Matus JS, Shin D, Sankar R, Mazarati A. Galanin contributes to monoaminergic dysfunction and to dependent neurobehavioral comorbidities of epilepsy. Exp Neurol. 2017;289:64–72.
Pineda EA, Hensler JG, Sankar R, Shin D, Burke TF, Mazarati AM. Plasticity of presynaptic and postsynaptic serotonin 1A receptors in an animal model of epilepsy-associated depression. Neuropsychopharmacology. 2011;36:1305–16.
Mazarati AM, Pineda E, Shin D, Tio D, Taylor AN, Sankar R. Comorbidity between epilepsy and depression: role of hippocampal interleukin-1beta. Neurobiol Dis. 2010;37:461–7.
Pineda EA, Hensler JG, Sankar R, Shin D, Burke TF, Mazarati AM. Interleukin-1β causes fluoxetine resistance in an animal model of epilepsy-associated depression. Neurotherapeutics. 2012;9:477–85.
Kumar U, Medel-Matus JS, Redwine HM, Shin D, Hensler JG, Sankar R, et al. Effects of selective serotonin and norepinephrine reuptake inhibitors on depressive- and impulsive-like behaviors and on monoamine transmission in experimental temporal lobe epilepsy. Epilepsia. 2016;57:506–15.
Shorvon S, Tomson T. Sudden unexpected death in epilepsy. Lancet. 2011;378:2028–38.
Mueller SG, Nei M, Bateman LM, Knowlton R, Laxer KD, Friedman D, et al. Brainstem network disruption: A pathway to sudden unexplained death in epilepsy? Hum Brain Mapp. 2018;39:4820–30.
Patodia S, Tan I, Ellis M, Somani A, Scheffer IE, Sisodiya SM, et al. Medullary tyrosine hydroxylase catecholaminergic neuronal populations in sudden unexpected death in epilepsy. Brain Pathol. 2021;31:133–43.
Patodia S, Somani A, O’Hare M, Venkateswaran R, Liu J, Michalak Z, et al. The ventrolateral medulla and medullary raphe in sudden unexpected death in epilepsy. Brain. 2018;141:1719–33.
Patodia S, Paradiso B, Ellis M, Somani A, Sisodiya SM, Devinsky O, et al. Characterisation of medullary astrocytic populations in respiratory nuclei and alterations in sudden unexpected death in epilepsy. Epilepsy Res. 2019;157:106213.
Petrucci AN, Joyal KG, Chou JW, Li R, Vencer KM, Buchanan GF. Post-ictal generalized EEG suppression is reduced by enhancing dorsal raphe serotonergic neurotransmission. Neuroscience. 2021;453:206–21.
Kommajosyula SP, Randall ME, Brozoski TJ, Odintsov BM, Faingold CL. Specific subcortical structures are activated during seizure-induced death in a model of sudden unexpected death in epilepsy (SUDEP): A manganese-enhanced magnetic resonance imaging study. Epilepsy Res. 2017;135:87–94.
Uteshev VV, Tupal S, Mhaskar Y, Faingold CL. Abnormal serotonin receptor expression in DBA/2 mice associated with susceptibility to sudden death due to respiratory arrest. Epilepsy Res. 2010;88:183–8.
Pineda E, Jentsch JD, Shin D, Griesbach G, Sankar R, Mazarati A. Behavioral impairments in rats with chronic epilepsy suggest comorbidity between epilepsy and attention-deficit/hyperactivity disorder. Epilepsy Behav. 2014;31:267–75.
McMahon JJ, Yu W, Yang J, Feng H, Helm M, McMahon E, et al. Seizure-dependent mTOR activation in 5-HT neurons promotes autism-like behaviors in mice. Neurobiol Dis. 2015;73:296–306.
Neuman RS, Thompson PM. Serotonin mediates suppression of focal epileptiform activity induced by noxious stimulation. Epilepsia. 1989;30:307–13.
Thompson PM, Zebrowski G, Neuman RS. Alteration of neocortical activity in response to noxious stimulation: participation of the dorsal raphe. Neuropharmacology. 1991;30:135–41.
de Oliveira RC, de Oliveira R, Biagioni AF, Falconi-Sobrinho LL, Coimbra NC. Dorsal raphe nucleus acetylcholine-mediated neurotransmission modulates post-ictal antinociception: The role of muscarinic and nicotinic cholinergic receptors. Brain Res. 2016;1631:80–91.
Freitas RL, Ferreira CM, Ribeiro SJ, Carvalho AD, Elias-Filho DH, Garcia-Cairasco N, et al. Intrinsic neural circuits between dorsal midbrain neurons that control fear-induced responses and seizure activity and nuclei of the pain inhibitory system elaborating postictal antinociceptive processes: a functional neuroanatomical and neuropharmacological study. Exp Neurol. 2005;191:225–42.
Freitas RL, Bassi GS, de Oliveira AM, Coimbra NC. Serotonergic neurotransmission in the dorsal raphe nucleus recruits in situ 5-HT(2A/2C) receptors to modulate the post-ictal antinociception. Exp Neurol. 2008;213:410–8.
Freitas RL, Ferreira CM, Urbina MA, Marino AU, Carvalho AD, Butera G, et al. 5-HT1A/1B, 5-HT6, and 5-HT7 serotonergic receptors recruitment in tonic-clonic seizure-induced antinociception: role of dorsal raphe nucleus. Exp Neurol. 2009;217:16–24.
de Oliveira RC, de Oliveira R, Ferreira CM, Coimbra NC. Involvement of 5-HT(2) serotonergic receptors of the nucleus raphe magnus and nucleus reticularis gigantocellularis/paragigantocellularis complex neural networks in the antinociceptive phenomenon that follows the post-ictal immobility syndrome. Exp Neurol. 2006;201:144–53.
Carlton SM, Leichnetz GR, Young EG, Mayer DJ. Supramedullary afferents of the nucleus raphe magnus in the rat: a study using the transcannula HRP gel and autoradiographic techniques. J Comp Neurol. 1983;214:43–58.
Acknowledgements
The work was supported by grants from the National Natural Science Foundation of China (81630098, 82022071) and the Starry Night Science Fund of the Zhejiang University Shanghai Institute for Advanced Study (SN-ZJU-SIAS-0011).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Cheng, Hm., Gao, Cs., Lou, Qw. et al. The diverse role of the raphe 5-HTergic systems in epilepsy. Acta Pharmacol Sin 43, 2777–2788 (2022). https://doi.org/10.1038/s41401-022-00918-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-022-00918-2