Abstract
Background
Prospective evidence supports active surveillance/watchful waiting (AS/WW) as an efficacious management option for low-risk prostate cancer that avoids potential treatment toxicity. AS/WW schedules require regular follow-up and adherence, and it is unknown to what extent patient socioeconomic status (SES) may impact management decisions for AS/WW. We sought to determine whether AS/WW use in the United States differs according to patient SES.
Design
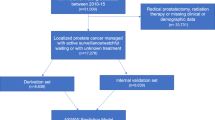
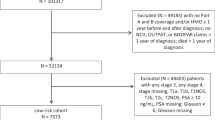
Using the Surveillance, Epidemiology, and End Results Prostate with AS/WW Database, all adult men diagnosed with localized low-risk prostate cancer (clinical T1–T2a, Gleason 6, and prostate-specific antigen <10 ng/mL) and managed with either AS/WW, radical prostatectomy, or radiotherapy were identified between 2010 and 2015. SES tertile was measured by the validated Yost Index (low: 0–10,901; middle: 10,904–11,469; high: 11,470–11,827). AS/WW trends were defined across SES tertiles from 2010 to 2015. Logistic multivariable regression defined adjusted odds ratios (aOR) for receipt of AS/WW by SES tertile.
Results
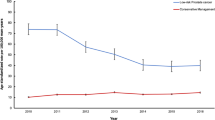
In 50,302 men, AS/WW use was higher with increasing SES tertile (24.6, 25.3, and 30.5% for low, middle, and high SES tertiles, respectively; PTrend (SES) <0.001). From 2010 to 2015, AS/WW use in the low, middle, and high SES tertiles increased from 11.2 to 37.3%, 14.1 to 45.8%, and 17.6 to 46.4%, respectively (PTrends <0.001). By 2015, likelihood of AS/WW became comparable among the middle vs. high SES tertiles (aOR 0.96, 95% confidence interval (CI): 0.83–1.11, P = 0.55), but remained lower among the low vs. high SES tertile (aOR 0.73, 95% CI: 0.64–0.83, P < 0.001).
Conclusions
AS/WW use for low-risk prostate cancer in the US differs by SES. Despite increases in AS/WW across SES from 2010 to 2015, patients from low SES received significantly lower rates of AS/WW compared with higher SES groups. SES may therefore influence management decisions, where factors associated with low SES might act as a barrier to AS/WW, and may need to be addressed to reduce any disproportionate risk of unnecessary treatment to lower SES patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Hamdy FC, Donovan JL, Lane JA, Mason M, Metcalfe C, Holding P, et al. 10-Year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med. 2016;375:1415–24.
Klotz L, Vesprini D, Sethukavalan P, Jethava V, Zhang L, Jain S, et al. Long-term follow-up of a large active surveillance cohort of patients with prostate cancer. J Clin Oncol. 2015;33:272–7.
Donovan JL, Hamdy FC, Lane JA, Mason M, Metcalfe C, Walsh E, et al. Patient-reported outcomes after monitoring, surgery, or radiotherapy for prostate cancer. N Engl J Med. 2016;375:1425–37.
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Prostate Cancer. Version 2. 2018, 8 Mar 2018. National Comprehensive Cancer Network, Inc. https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf. Accessed 1 Jul 2018.
Mahal BA, Butler S, Franco I, Spratt DE, Rebbeck TR, D’Amico AV, et al. Use of active surveillance or watchful waiting for low-risk prostate cancer and management trends across risk groups in the United States, 2010–2015. JAMA. 2019;321:704–6.
Loeb S, Byrne N, Makarov DV, Lepor H, Walter D. Use of conservative management for low-risk prostate cancer in the veterans affairs integrated health care system from 2005–2015. JAMA. 2018;319:2231–3.
D’Amico AV. Active surveillance versus treatment of prostate cancer: should metastasis be the primary end point? J Clin Oncol. 2017;35:1638–40.
Loeb S, Walter D, Curnyn C, Gold HT, Lepor H, Makarov DV. How active is active surveillance? Intensity of followup during active surveillance for prostate cancer in the United States. J Urol. 2016;196:721–6.
Zapka J, Taplin SH, Price RA, Cranos C, Yabroff R. Factors in quality care—the case of follow-up to abnormal cancer screening tests-problems in the steps and interfaces of care. J Natl Cancer Inst Monogr. 2010;2010:58–71.
Surveillance, Epidemiology, and End Results Program Prostate with Active Surveillance/Watchful Waiting Database. 2018. https://seer.cancer.gov/seerstat/databases/prostate-ww/index.html. Accessed 28 May 2018.
Yost K, Perkins C, Cohen R, Morris C, Wright W. Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control. 2001;12:703–11.
Mohler JL, Kantoff PW, Armstrong AJ, Bahnson RR, Cohen M, D’Amico AV, et al. Prostate cancer, version 2. 2014. J Natl Compr Canc Netw. 2014;12:686–718.
Loeb S, Bjurlin MA, Nicholson J, Tammela TL, Penson DF, Carter HB, et al. Overdiagnosis and overtreatment of prostate cancer. Eur Urol. 2014;65:1046–55.
Boyajian R, Simeoli A, Orio PF, Martin NE, King MT, Mouw KW, et al. Virtual PSA Monitoring Program Pilot: the integration of technology in post treatment prostate cancer patient care to optimize workflow and increase access to care. Int J Radiat Oncol Biol Phys. 2018;102:e101–e102.
Loeb S, Curnyn C, Fagerlin A, Braithwaite RS, Schwartz MD, Lepor H, et al. Informational needs during active surveillance for prostate cancer: a qualitative study. Patient Educ Couns. 2018;101:241–7.
Acknowledgements
Dr. Mahal is funded by the Prostate Cancer Foundation-American Society for Radiation Oncology Award to End Prostate Cancer. Dr. Nguyen is funded by the Prostate Cancer Foundation. None of the funders listed above had any input on the design and conduct of the study; None of the funders listed above had any input on the collection, management, analysis, and interpretation of the data; None of the funders listed above had any input on the preparation, review, or approval of the manuscript; None of the funders listed above had any input on the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Butler, S.S., Loeb, S., Cole, A.P. et al. United States trends in active surveillance or watchful waiting across patient socioeconomic status from 2010 to 2015. Prostate Cancer Prostatic Dis 23, 179–183 (2020). https://doi.org/10.1038/s41391-019-0175-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-019-0175-9
This article is cited by
-
Intensity of observation with active surveillance or watchful waiting in men with prostate cancer in the United States
Prostate Cancer and Prostatic Diseases (2023)