Abstract
Background
To describe temporal and sociodemographic patterns of antimicrobial exposure during the first year of life in a large US cohort.
Methods
Singleton infants born 1998–2014 enrolled in Kaiser Permanente Northern California integrated health system (n = 345,550) were followed longitudinally via comprehensive electronic health records, capturing all systemic antimicrobial inpatient administrations and outpatient dispensings. Antimicrobial exposure was summarized by maternal and infant characteristics, birth year, inpatient/outpatient status, age in months, and drug class.
Results
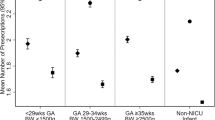
Overall, 44% of infants in this cohort received at least one dose of antimicrobials during infancy. Decreases over time were driven by reduced outpatient dispensings specifically in later infancy, primarily for penicillins. Among infants receiving any antimicrobials the median number of exposure-days was 16. Inpatient dispensings peaked in the first 30 days of life and outpatient dispensings peaked at 10–11 months. Birth characteristics (i.e., NICU admission, gestational age) were strong independent predictors of antimicrobial exposure between 0– < 3 months; sociodemographic factors were modest predictors of exposure for 3–12 months.
Conclusion
Predictors of antimicrobial exposure in early and late infancy are distinct with early infancy exposures highly correlated to birth characteristics. The cumulative proportion of infants exposed has decreased due to fewer late infancy outpatient dispensings.
Impact
-
Comprehensive antimicrobial exposure histories and the maternal and infant characteristics predicting exposure have not been well described in US populations.
-
This analysis provides estimates of cumulative antimicrobial exposures by sociodemographic factors, delivery characteristics, month of life, inpatient/outpatient status, and antibiotic class among one of the largest US HMOs.
-
Predictors of early infancy antimicrobial exposures differ from those in late infancy, with early exposures strongly correlated to birth characteristics and late infancy exposures modestly related to sociodemographic factors.
-
Antimicrobial exposure among infants decreased over the time period primarily due to reduced outpatient dispensings in later infancy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data that support the findings of this study are from the electronic medical record databases at Kaiser Permanente Northern California. Restrictions apply to the availability of these data, which were used with their permission for the current study, and so are not publicly available.
References
Al-Turkait, A., Szatkowski, L., Choonara, I. & Ojha, S. Drug utilisation in neonatal units in England and Wales: a national cohort study. Eur. J. Clin. Pharm. 78, 669–677 (2022).
De Jong, J., Van Den Berg, P. B., De Vries, T. W. & De Jong-van Den Berg, L. T. W. Antibiotic drug use of children in the Netherlands from 1999 till 2005. Eur. J. Clin. Pharm. 64, 913–919 (2008).
Hsieh, E. et al. Medication Use in the Neonatal Intensive Care Unit. Am. J. Perinatol. 31, 811–822 (2013).
Holstiege, J. & Garbe, E. Systemic antibiotic use among children and adolescents in Germany: a population-based study. Eur. J. Pediatr. 172, 787–795 (2013).
Stam, J. et al. Antibiotic use in infants in the first year of life in five European countries: Antibiotic use in infants. Acta Paediatrica 101, 929–934 (2012).
Youngster, I. et al. Antibiotic Use in Children – A Cross-National Analysis of 6 Countries. J. Pediatrics 182, 239–244.e1 (2017).
Cantey, J. B., Wozniak, P. S. & Sánchez, P. J. Prospective Surveillance of Antibiotic Use in the Neonatal Intensive Care Unit: Results From the SCOUT Study. Pediatr. Infect. Dis. J. 34, 267–272 (2015).
Hsia, Y. et al. Use of the WHO Access, Watch, and Reserve classification to define patterns of hospital antibiotic use (AWaRe): an analysis of paediatric survey data from 56 countries. Lancet Glob. Health 7, e861–e871 (2019).
Vaz, L. E. et al. Recent Trends in Outpatient Antibiotic Use in Children. Pediatrics 133, 375–385 (2014).
Versporten, A., Bielicki, J., Drapier, N. & Sharland, M. & Goossen,s H. The Worldwide Antibiotic Resistance and Prescribing in European Children (ARPEC) point prevalence survey: developing hospital-quality indicators of antibiotic prescribing for children. J. Antimicrob. Chemother. 71, 1106–1117 (2016).
Kim, H., Sitarik, A. R., Woodcroft, K., Johnson, C. C. & Zoratti, E. Birth mode, breastfeeding, pet exposure, and antibiotic use: associations with the gut microbiome and sensitization in children. Curr. Allergy Asthma Rep. 19, 22 (2019).
Fjalstad, J. W., Esaiassen, E., Juvet, L. K., Van Den Anker, J. N. & Klingenberg, C. Antibiotic therapy in neonates and impact on gut microbiota and antibiotic resistance development: a systematic review. J. Antimicrobial Chemother. 73, 569–580 (2018).
McDonnell, L. et al. Association between antibiotics and gut microbiome dysbiosis in children: systematic review and meta-analysis. Gut Microbes 13, 1870402 (2021).
Reyman, M. et al. Effects of early-life antibiotics on the developing infant gut microbiome and resistome: a randomized trial. Nat. Commun. 13, 893 (2022).
Baron, R. et al. The relationship of prenatal antibiotic exposure and infant antibiotic administration with childhood allergies: a systematic review. BMC Pediatr. 20, 312 (2020).
Anderson, H. et al. Prevalence and determinants of antibiotic exposure in infants: a population-derived Australian birth cohort study: antibiotic use in Australian infants. J. Paediatr. Child Health 53, 942–949 (2017).
Gagliotti, C., Morsillo, F., Resi, D., Milandri, M. & Moro, M. L. Antibiotic treatments for children ages 0–23 months in a Northern Italy Region: a cohort study. Infection 34, 155–157 (2006).
Kinlaw, A. C. et al. Trends in antibiotic use by birth season and birth year. Pediatrics 140, e20170441 (2017).
Pottegård, A. et al. Use of antibiotics in children: a Danish nationwide drug utilization study. Pediatr. Infect. Dis. J. 34, e16–e22 (2015).
Hales, C. M., Kit, B. K., Gu, Q. & Ogden, C. L. Trends in prescription medication use among children and adolescents—United States, 1999-2014. JAMA 319, 2009 (2018).
Snowden, J. M. & Klebanoff, M. A. Accurate identification of cohort study designs in perinatal research: a practical guide. Am. J. Obstet. Gynecol. 227, 231–235.e1 (2022).
Richards, M. et al. Intrapartum antibiotics and childhood asthma and allergic rhinitis: a retrospective cohort study. BJOG 129, 722–730 (2022).
Zou, G. A modified Poisson regression approach to prospective studies with binary data. Am. J. Epidemiol. 159, 702–706 (2004).
Spiegelman, D. & Hertzmark, E. Easy SAS calculations for risk or prevalence ratios and differences. Am. J. Epidemiol. 162, 199–200 (2005).
Curtis, H. J., Walker, A. J., Mahtani, K. R. & Goldacre, B. Time trends and geographical variation in prescribing of antibiotics in England 1998–2017. J. Antimicrobial Chemotherapy 74, 242–250 (2019).
Hobbs, M. R. et al. Antibiotic consumption by New Zealand children: exposure is near universal by the age of 5 years. J. Antimicrobial Chemother. 72, 1832–1840 (2017).
Lorch, S. A. et al. Antibiotic use in premature infants after discharge from the Neonatal Intensive Care Unit. Clin. Pediatr. 49, 249–257 (2010).
Hellman, J., Grape, M. & Ternhag, A. Antibiotic consumption among a Swedish cohort of children born in 2006. Acta Paediatr. 104, 1035–1038 (2015).
Lemas, D. J., et al. Postnatal pediatric systemic antibiotic episodes during the first three years of life are not associated with mode of delivery. PLoS One. 15, e0229861 (2020).
Marra, F., Patrick, D. M., Chong, M. & Bowie, W. R. Antibiotic use among children in British Columbia, Canada. J. Antimicrobial Chemother. 58, 830–839 (2006).
Touboul-Lundgren, P., Bruno, P., Bailly, L., Dunais, B. & Pradier, C. Paediatric antibiotic prescriptions in primary care in the Alpes-Maritimes area of southeastern France between 2008 and 2013. Eur. J. Clin. Microbiol. Infect. Dis. 36, 509–516 (2017).
Flannery, D. D. et al. Temporal trends and center variation in early antibiotic use among premature infants. JAMA Netw. Open 1, e180164 (2018).
Gordon, N. P. A comparison of sociodemographic and health characteristics of the Kaiser Permanente Northern California membership derived from two data sources: the 2008 Member Health Survey and the 2007 California Health Interview Survey (Kaiser Permanente Division of Research, 2012).
Gordon, N. P. Similarity of the adult Kaiser Permanente membership in Northern California to the insured and general population in Northern California: statistics from the 2011 California Health Interview Survey (Kaiser Permanente Division of Research, 2015).
Funding
NIH/NIAID Grant #R01AI122266. NIH did not provide input into study design.
Author information
Authors and Affiliations
Contributions
Hannah Barca conducted data management, carried out analyses, created data visualizations, drafted the manuscript, and critically reviewed and revised the manuscript. Jeannette Ferber produced the study datasets, conducted data management, and critically reviewed the manuscript. Megan Richards conducted data management, drafted code for data visualization, participated in conceptualizing the study, and critically reviewed and revised the manuscript. Matthew Strickland provided input on study design and critically reviewed and revised the manuscript. AJ Fernandez provided input on antimicrobial description and categorization, and critically reviewed and revised the manuscript. De-Kun Li participated in the process of obtaining funding, acquisition of data, and critically reviewed and revised the manuscript. Lyndsey Darrow conceptualized and designed the study, supervised data analyses, drafted the manuscript, and critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent Statement
All KPNC members provide consent to medical research using their EHR data upon enrollment, so no personal consent is required for accessing KPNC EHR data for IRB approved research projects.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Barca, H.C., Ferber, J., Richards, M. et al. Antimicrobial exposure during infancy in a longitudinal California cohort. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03171-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03171-x