Abstract
Background
Advanced perinatal medicine has decreased the mortality rate of preterm infants. Long-term neurodevelopmental outcomes of very-low-birth-weight infants (VLBWIs) remain to be investigated.
Methods
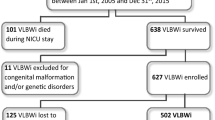
Participants were 124 VLBWIs who had in-hospital birth from 2007 to 2015. Perinatal information, developmental or intelligence quotient (DQ/IQ), and neurological comorbidities at ages 3 and 6 years were analyzed.
Results
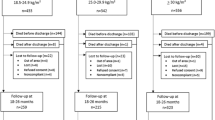
Fifty-eight (47%) VLBWIs received neurodevelopmental assessments at ages 3 and 6 years. Among them, 15 (26%) showed DQ/IQ <75 at age 6 years. From age 3 to 6 years, 21 (36%) patients showed a decrease (≤–10), while 5 (9%) showed an increase (≥+10) in DQ/IQ scores. Eight (17%) with autism spectrum disorder or attention-deficit hyperactivity disorder (ASD/ADHD) showed split courses of DQ/IQ, including two with ≤–10 and one with +31 to their scores. On the other hand, all 7 VLBWIs with cerebral palsy showed DQ ≤35 at these ages. Magnetic resonance imaging detected severe brain lesions in 7 (47%) of those with DQ <75 and 1 (18%) with ASD/ADHD.
Conclusions
VLBWIs show a broad spectrum of neurodevelopmental outcomes after 6 years. These divergent profiles also indicate that different risks contribute to the development of ASD/ADHD from those of cerebral palsy and epilepsy in VLBWIs.
Impact
-
Very-low-birth-weight infants (VLBWIs) show divergent neurodevelopmental outcomes from age 3 to 6 years.
-
A deep longitudinal study depicts the dynamic change in neurodevelopmental profiles of VLBWIs from age 3 to 6 years.
-
Perinatal brain injury is associated with developmental delay, cerebral palsy and epilepsy, but not with ASD or ADHD at age 6 years.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All data are available in the main manuscript and Supplementary information.
References
Younge, N. et al. Survival and neurodevelopmental outcomes among periviable infants. N. Engl J. Med. 376, 617–628 (2017).
Inoue, H. et al. Neurodevelopmental outcomes in infants with birth weight </=500 g at 3 years of age. Pediatrics 142, e20174286 (2018).
Inoue, H. et al. Early mortality and morbidity in infants with birth weight of 500 grams or less in Japan. J. Pediatr. 190, 112–117.e113 (2017).
Kono, Y., Mishina, J., Yonemoto, N., Kusuda, S. & Fujimura, M. Outcomes of very-low-birthweight infants at 3 years of age born in 2003-2004 in Japan. Pediatr. Int. 53, 1051–1058 (2011).
Matsushita, Y. et al. Association of perinatal factors of epilepsy in very low birth weight infants, using a nationwide database in Japan. J. Perinatol. 39, 1472–1479 (2019).
Tamaru, S. et al. Neurodevelopmental outcomes of very low birth weight and extremely low birth weight infants at 18 months of corrected age associated with prenatal risk factors. Early Hum. Dev. 87, 55–59 (2011).
Kidokoro, H. et al. Brain injury and altered brain growth in preterm infants: predictors and prognosis. Pediatrics 134, e444–e453 (2014).
Ochiai, M. et al. Longitudinal study of very low birth weight infants until 9years of age; attention deficit hyperactivity and autistic features are correlated with their cognitive functions. Early Hum. Dev. 91, 783–786 (2015).
Khazanchi, R., Lyden, E. R. & Peeples, E. S. Reevaluating 30-day head ultrasound screening for preterm infants in the era of decreasing periventricular leukomalacia. J. Matern. Fetal Neonatal Med. 35, 907–913 (2022).
Ochiai, M. et al. Survival and neurodevelopmental outcome of preterm infants born at 22-24 weeks of gestational age. Neonatology 105, 79–84 (2014).
Counsell, S. J., Rutherford, M. A., Cowan, F. M. & Edwards, A. D. Magnetic resonance imaging of preterm brain injury. Arch. Dis. Child Fetal Neonatal Ed. 88, F269–F274 (2003).
Martinez-Biarge, M. et al. MRI based preterm white matter injury classification: the importance of sequential imaging in determining severity of injury. PLoS One 11, e0156245 (2016).
Rogers, C. E., Lean, R. E., Wheelock, M. D. & Smyser, C. D. Aberrant structural and functional connectivity and neurodevelopmental impairment in preterm children. J. Neurodev. Disord. 10, 38 (2018).
Smyser, C. D., Wheelock, M. D., Limbrick, D. D. Jr & Neil, J. J. Neonatal brain injury and aberrant connectivity. Neuroimage 185, 609–623 (2019).
Vaher, K. et al. General factors of white matter microstructure from DTI and NODDI in the developing brain. Neuroimage 254, 119169 (2022).
Meldrum, S. J. et al. Autism spectrum disorder in children born preterm-role of exposure to perinatal inflammation. Front. Neurosci. 7, 123 (2013).
Torio, M. et al. Neurodevelopmental outcomes of high-risk preterm infants: a prospective study in Japan. Neurol. Clin. Pract. 11, 398–405 (2021).
Serenius, F. et al. Neurodevelopmental outcomes among extremely preterm infants 6.5 years after active perinatal care in Sweden. JAMA Pediatr. 170, 954–963 (2016).
Koeda, T. & Takeshita, K. Visuo-perceptual impairment and cerebral lesions in spastic diplegia with preterm birth. Brain Dev. 14, 239–244 (1992).
Novak, I. et al. Early, accurate diagnosis and early intervention in cerebral palsy: advances in diagnosis and treatment. JAMA Pediatr. 171, 897–907 (2017).
Palumbi, R. et al. Neurodevelopmental and emotional-behavioral outcomes in late-preterm infants: an observational descriptive case study. BMC Pediatr. 18, 318 (2018).
Sakuta, S. et al. Clinical features of behavioral symptoms in patients with semantic dementia: does semantic dementia cause autistic traits? PLoS One 16, e0247184 (2021).
Patel, R. M. Short- and long-term outcomes for extremely preterm infants. Am. J. Perinatol. 33, 318–328 (2016).
Rommel, A. S. et al. Association of preterm birth with attention-deficit/hyperactivity disorder-like and wider-ranging neurophysiological impairments of attention and inhibition. J. Am. Acad. Child Adolesc. Psychiatry 56, 40–50 (2017).
Nakashima, T. et al. Trends in bronchopulmonary dysplasia among extremely preterm infants in Japan, 2003-2016. J. Pediatr. 230, 119–125.e117 (2021).
Yasuoka, K. et al. Late-onset circulatory collapse and risk of cerebral palsy in extremely preterm infants. J. Pediatr. 212, 117–123.e114 (2019).
Chen, L. W. et al. Early neurodevelopmental trajectories for autism spectrum disorder in children born very preterm. Pediatrics 146, e20200297 (2020).
Lejeune, F. et al. Effects of an early postnatal music intervention on cognitive and emotional development in preterm children at 12 and 24 months: preliminary findings. Front. Psychol. 10, 494 (2019).
Isayama, T. The clinical management and outcomes of extremely preterm infants in Japan: past, present, and future. Transl. Pediatr. 8, 199–211 (2019).
Nakanishi, H. et al. Trends in the neurodevelopmental outcomes among preterm infants from 2003-2012: a retrospective cohort study in Japan. J. Perinatol. 38, 917–928 (2018).
Cayam-Rand, D. et al. Predicting developmental outcomes in preterm infants: a simple white matter injury imaging rule. Neurology 93, e1231–e1240 (2019).
DeMaster, D. et al. Nurturing the preterm infant brain: leveraging neuroplasticity to improve neurobehavioral outcomes. Pediatr. Res. 85, 166–175 (2019).
Schlapbach, L. J. et al. Impact of sepsis on neurodevelopmental outcome in a Swiss national cohort of extremely premature infants. Pediatrics 128, e348–e357 (2011).
Brouwer, A. et al. Neurodevelopmental outcome of preterm infants with severe intraventricular hemorrhage and therapy for post-hemorrhagic ventricular dilatation. J. Pediatr. 152, 648–654 (2008).
Fazzi, E. et al. Neurodevelopmental outcome at 5-7 years in preterm infants with periventricular leukomalacia. Neuropediatrics 25, 134–139 (1994).
Pavlek, L. R., Mueller, C., Jebbia, M. R., Kielt, M. J. & Fathi, O. Near-infrared spectroscopy in extremely preterm infants. Front. Pediatr. 8, 624113 (2020).
Gano, D. & Barkovich, A. J. Cerebellar hypoplasia of prematurity: causes and consequences. Handb. Clin. Neurol. 162, 201–216 (2019).
Bax, M. C. Terminology and classification of cerebral palsy. Dev. Med. Child Neurol. 6, 295–297 (1964).
Knickmeyer, R. C. et al. A structural MRI study of human brain development from birth to 2 years. J. Neurosci. 28, 12176–12182 (2008).
Spoto, G. et al. Cerebellum and prematurity: a complex interplay between disruptive and dysmaturational events. Front. Syst. Neurosci. 15, 655164 (2021).
Hayakawa, K. et al. Pontine and cerebellar injury in neonatal hypoxic-ischemic encephalopathy: MRI features and clinical outcomes. Acta Radio. 61, 1398–1405 (2020).
Agrawal, S., Rao, S. C., Bulsara, M. K. & Patole, S. K. Prevalence of autism spectrum disorder in preterm infants: a meta-analysis. Pediatrics 142, e20180134 (2018).
Kita, Y., Ashizawa, F. & Inagaki, M. Prevalence estimates of neurodevelopmental disorders in Japan: a community sample questionnaire study. Psychiatry Clin. Neurosci. 74, 118–123 (2020).
Zablotsky, B. et al. Prevalence and trends of developmental disabilities among children in the United States: 2009-2017. Pediatrics 144, e20190811 (2019).
O’Reilly, H., Johnson, S., Ni, Y., Wolke, D. & Marlow, N. Neuropsychological outcomes at 19 years of age following extremely preterm birth. Pediatrics 145, e20192087 (2020).
O’Reilly, H., Ni, Y., Johnson, S., Wolke, D. & Marlow, N. Extremely preterm birth and autistic traits in young adulthood: The Epicure Study. Mol. Autism 12, 30 (2021).
Acknowledgements
We thank Drs Toshiro Hara (President Fukuoka Children’s Hospital, Professor Emeritus at Kyushu University), and Ryutaro Kira (Fukuoka Children’s Hospital) for their cordial support of this research; Drs Takeshi Shono and Kumiko Shono (Department of Pediatric Surgery, KMC) for the management of patients; and all physicians and co-medical staff in our department for helpful discussions.
Funding
This study was supported by JSPS KAKENHI grant numbers JP19K10613 (P.F.C.), JP18K15677 (Y.S.), JP17K16271 (Y.I.), JP19K08281 (Y.S.); AMED grant numbers JP20ek0109411, JP20wm0325002h; Research grant for prion diseases from the Ministry of Health, Labour and Welfare of Japan (JP20FC1054); The Japan Epilepsy Research Foundation, and Kawano Masanori Memorial Public Interest Incorporated Foundation for Promotion of Pediatrics (Y.S.).
Author information
Authors and Affiliations
Contributions
R.O., K.W., P.F.C., and Y.S. analyzed data and drafted the manuscript. R.O., K.W., and J.O. performed the neurodevelopmental tests. T.N., Y. Sakemi, T.O., Y. Sonoda, Y.I., H.I., and M.O. managed the patients and analyzed data. H.Y. and S.O. conceptualized and organized the grand-design of this study. All of the authors critically reviewed and approved the final form of this manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was approved by the Institutional Review Boards at KMC (REC2021–024) and Kyushu University (#29-628 and #29-635).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ogata, R., Watanabe, K., Chong, P.F. et al. Divergent neurodevelopmental profiles of very-low-birth-weight infants. Pediatr Res 95, 233–240 (2024). https://doi.org/10.1038/s41390-023-02778-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02778-w
This article is cited by
-
Association of birthweight and risk of incident dementia: a prospective cohort study
GeroScience (2024)
-
Synergistic effects of achieving perinatal interventions on bronchopulmonary dysplasia in preterm infants
European Journal of Pediatrics (2024)