Abstract
Background
Previous studies have shown that aberrant T lymphocyte apoptosis is involved in the pathogenesis of uveitis. Genetic variants of apoptotic pathway-related factors (including PDCD1, PDCD1LG2, FAS, and FASLG) may affect apoptosis and in turn predict susceptibility to autoimmune disease. This has not yet been studied in pediatric idiopathic uveitis (PIU) and juvenile idiopathic arthritis (JIA)-associated uveitis and was therefore the subject of the study presented here.
Methods
Fourteen single-nucleotide polymorphisms (SNPs) of several apoptosis-related pathway genes were analyzed in 1238 PIU patients, 128 JIA-associated uveitis patients and 1114 healthy controls using the iPLEX Gold Assay and MassARRAY platform.
Results
A lower frequency of the PDCD1/rs6710479 CC genotype in PIU patients was found when compared to controls (Pc = 3.42 × 10−3). A higher frequency of the PDCD1/rs7421861 A allele (Pc = 4.85 × 10−3) was observed in PIU patients as compared with controls. Stratification analysis showed a positive association of band keratopathy with the PDCD1/rs7565639 CT genotype (Pc = 1.05 × 10−2) and a negative association of this parameter with the PDCD1/rs7565639 C allele (Pc = 3.76 × 10−2).
Conclusions
This study revealed that rs6710479 and rs7421861 in the PDCD1 gene confer susceptibility to PIU in Han Chinese. A stratified analysis showed that PDCD1/rs7565639 is associated with band keratopathy in PIU patients.
Similar content being viewed by others
Introduction
Uveitis is an umbrella term for inflammatory diseases involving the uveal tract, retina, and vitreous, which can lead to significant visual impairment.1 Pediatric uveitis (PU) accounts for 2.2–13.8% of all uveitis cases and has a high risk of developing band keratopathy, cataract, secondary glaucoma, amblyopia, and other ocular complications.2 Almost all uveitis entities occurring in adults may also be seen in children. However, the most common subtype is pediatric idiopathic uveitis (PIU), and the second is juvenile idiopathic arthritis (JIA)-associated uveitis.3 Although the etiology of uveitis in children is not completely clarified, aberrant immune reactivity and genetic predisposition have been shown to be involved in its pathogenesis.4
Apoptosis is a mechanism that precisely eliminates unwanted cells and is essential for normal physiological transformation of cells as well as in various pathological processes.5 Previous studies have shown that the nuclear factor-kB signaling pathway is closely related to apoptosis and is involved in the transcriptional regulation of various apoptosis-related genes, which is an important pathway regulating immunity.6,7 There are four major genes in this pathway, including programmed cell death 1 (PDCD1), PDCD1LG2, FAS, and FASLG.8,9,10 Aberrant expression of these genes has been shown to be involved in certain autoimmune diseases.11,12,13,14 Polymorphisms of these genes have also been shown to be associated with a variety of autoimmune diseases, such as rheumatoid arthritis (RA),15 Graves’ disease,16 ankylosing spondylitis (AS),17 and systemic lupus erythematosus (SLE).18 Furthermore, their polymorphisms have also been shown to be associated with certain cancers,19,20 which might be related to its role in the process of cancer immunology. Whether these polymorphisms are also associated with PIU is not known and was therefore the subject of the present study.
Materials and methods
Study population
A total of 1238 patients with PIU, 128 JIA-associated uveitis patients, and 1114 healthy controls were included in this study. All the enrolled patients and healthy controls were Han Chinese. PIU was identified as uveitis in children whose age at onset was <16 years and not belonging to a well-defined uveitis entity. Patients with definite posterior involvement or with panuveitis were excluded from the study. These PIU patients all showed anterior uveitis evidenced by keratic precipitates, aqueous flare, and cells. Vitreous cells and opacities were observed in 148 cases. There was no obvious fundus abnormalities in our patients. Children with infectious uveitis entities and specific entities such as Vogt–Koyanagi–Harada syndrome diagnosed according to both sets of criteria presumed by the International Committee on Vogt–Koyanagi–Harada Disease Nomenclature21 and Yang et al.,22 Behcet’s disease (BD) diagnosed by the diagnostic criteria of the International Study Group for BD,23 Fuchs syndrome, or other defined uveitis types were also excluded from this study. According to the International Union of Rheumatology Association standards, JIA was defined as arthritis, without any other identifiable etiology in children under the age of 16 years, and existing for at least 6 weeks.24 All JIA patients were diagnosed by Rheumatologists and uveitis was diagnosed at the uveitis center of our hospital. All uveitis patients were seen by the same senior uveitis expert (P.Y.). Blood samples of all controls and patients were obtained from the uveitis center of the Department of Ophthalmology of the First Affiliated Hospital of Chongqing Medical University (Chongqing, China from May 2009 to May 2018) and the Department of Ophthalmology of the First Affiliated Hospital of Zhengzhou University (Zhengzhou, China from May 2017 to May 2018).
Ethical considerations
The study was approved by the Medical Ethics Committee of The First Affiliated Hospital of Zhengzhou University and the Clinical Research Ethics Committee of the First Affiliated Hospital of Chongqing Medical University, and each participant offered their informed consent before enrolment in the study. For minors, the informed consent was obtained from their parents or guardians. All procedures in this project followed the principles of the Helsinki Declaration.
Single-nucleotide polymorphism (SNP) choice and genotypes
Fourteen SNPs were selected from PDCD1, PDCD1LG2, FAS, and FASLG genes as candidates in this study, which were earlier shown to be significantly (P < 0.05) associated with a variety of autoimmune diseases or certain cancers.15,17,18,19,20,25,26,27,28 Candidate SNPs were screened on HaploView 4.2 with an r2 threshold of 0.8 and a minor allele frequency >0.05. The data of linkage disequilibrium from the Han Chinese Hap Map database were also taken into account. After using these criteria, the following SNPs were chosen for the study: four SNPs (rs7421861, rs2227982, rs6710479, rs7565639) of PDCD1, three SNPs (rs12001295, rs7852996, rs16923189) of PDCD1LG2, three SNPs (rs2234978, rs2234767, rs1468063) of FAS, and four SNPs (rs763110, rs5030772, rs859637, rs9286879) of FASLG.
The extraction of DNA and genotyping
Genomic DNA was obtained from peripheral blood using the QIAamp DNA Blood Mini Kit (QIAGEN, Valencia, CA). DNA was stored at −80 °C. The primers used to genotype were made according to the MassARRAY Assay software. Genotyping of these 14 selected SNPs were ascertained by iPLEX Gold Assay and the MassARRAY platform (Sequenom, San Diego, CA) using standard procedures. Data were analyzed by the MassARRAY Typer software (version 4.0).
Statistical analysis
The Hardy–Weinberg equilibrium of all candidate SNPs was calculated by χ2 test. Differences in allele and genotype frequencies were assessed by χ2 test or Fisher’s exact correction using the SPSS software (version 21.0, Chicago, IL), as well as calculation of odds ratios (ORs) and 95% confidence intervals. The P value was corrected by the Bonferroni method for multiple comparisons (Pc). Pc < 0.05 was defined as statistically significant.
Results
Clinical features
The clinical characteristics, family history of autoimmune diseases, laterality, gender, and age distribution of the PIU and JIA-associated uveitis patients as well as healthy controls are shown in Table 1. The PIU patients consisted of 1238 subjects (603 males and 635 females) with an average age of 10.5 ± 4.3 years at disease onset. JIA-associated uveitis patients included 47 males and 81 females with an average age of 9.6 ± 7.2 years at first disease onset. The mean age of healthy controls (including 516 males and 598 females) was 39.5 ± 10.4 years. In the PIU patients, family history of autoimmune diseases was noted in 40 cases, including RA (15), AS (12), SLE (2), vitiligo (3), psoriasis (4), scleroderma (1), polymyositis (1), eczema (1), and ichthyosis (1). In the JIA-associated uveitis patients, family history of autoimmune diseases was present in 9 cases, including RA (5), AS (3), and psoriasis (1).
Genotype and allele frequencies of SNPs in PIU
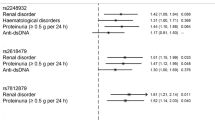
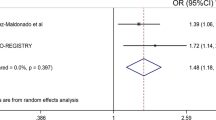
Fourteen SNPs in PDCD1, PDCD1LG2, FAS, and FASLG were genotyped and statistically analyzed in 1238 PIU patients and 1114 healthy controls. Significant differences were observed for SNP rs6710479 and rs7421861 in PDCD1 between patients and controls (Table 2). The frequency of the CC genotype of rs6710479 in PIU cases was significantly lower (P = 7.13 × 10−4; Pc = 3.42 × 10−3; OR = 0.466) than that in normal controls. Analysis of rs7421861 showed a lower frequency of the G allele (P = 1.01 × 10−4; Pc = 4.85 × 10−3; OR = 0.741) and higher frequencies of the AA genotype (P = 1.64 × 10−4; Pc = 7.87 × 10−3; OR = 1.407) and A allele (P = 1.01 × 10−4; Pc = 4.85 × 10−3; OR = 1.350) in PIU patients. No association could be detected between PIU and the other SNPs examined (Appendix 1).
Genotype and allele frequency of SNPs in the stratified analysis
Band keratopathy and cataract were the two most common complications in the PIU patients. To assess the association of selected SNPs with these two clinical features, we made a stratified analysis. A higher frequency of the PDCD1/rs7565639 T allele and CT genotype (P = 7.83 × 10−4, Pc = 3.76 × 10−2, OR = 1.732; P = 2.18 × 10−4, Pc = 1.05 × 10−2, OR = 1.879, respectively) and a lower frequency of the C allele (P = 7.83 × 10−4; Pc = 3.76 × 10−2; OR = 0.577) was found in patients with band keratopathy as compared to healthy controls (Table 3). There was no association of the 14 SNPs with the presence of complicated cataract (Appendix 2).
Genotype and allele frequencies of SNPs in JIA-associated uveitis
Fourteen SNPs in PDCD1, PDCD1LG2, FAS, and FASLG were also genotyped and statistically analyzed in 128 JIA-associated uveitis patients and 1114 healthy controls. The results showed a tendency of an association between three SNPs (rs2227982, rs6710479 and rs7421861) of the PDCD1 gene and JIA-associated uveitis (Table 4). Significance was, however, lost after Bonferroni correction (Appendix 3).
Discussion
The present study explored the genetic susceptibility of PIU in Han Chinese with apoptosis-related genes and showed a significant association with PDCD1 but not with PDCD1LG2, FAS, and FASLG. Polymorphisms of rs6710479 and rs7421861 in the PDCD1 gene were associated with PIU in Han Chinese, whereby individuals carrying the PDCD1/rs6710479 CC genotype were protected against PIU. Individuals with the PDCD1/ rs7421861 AA genotype or A allele were at a higher risk to develop this disease. Stratification analysis showed an association between band keratopathy and PDCD1/rs7565639, whereby the T allele or CT genotype was a risk factor and the CC genotype was protective.
Although the true pathogenesis of PIU remains unclear, immunological and genetic factors are likely to be involved.4 Previous studies on the genetic susceptibility of PIU have demonstrated that genetic polymorphisms of certain genes may play a role in the pathogenesis of PIU.29,30 However, its genetic background is not exactly clear yet, mainly due to the difficulty in collecting enough samples for such studies. For this purpose, we continuously collected the samples from PU patients over the past 9 years. In the patients with PU included in the present study, 98% (1213) were being referred to our uveitis center by doctors from local hospitals due to recurrent or refractory uveitis. The patients with one or two attacks were always treated at local hospitals. To ensure patient consistency and diagnostic accuracy, we made a large effort to only include those PIU patients and JIA patients who fulfilled strict diagnostic criteria. The 14 SNPs we selected from the apoptosis-related genes PDCD1, PDCD1LG2, FAS, and FASLG were based on previous studies and all the included SNPs had earlier been shown to be associated with at least one autoimmune disease or certain cancers.15,17,18,19,20,25,26,27,28
To the best of our knowledge, an association of PIU with a genetic variant of PDCD1 has not been previously reported. PDCD1 is a member of the cluster of differentiation 28 (CD28)/B7 family.9 PDCD1 is also expressed on ocular tissues and is involved in the induction of T lymphocyte apoptosis and inhibition of lymphocyte proliferation and cytokine secretion. It is thought to play an important role in the induction and/or maintenance of peripheral tolerance and autoimmune disease.31 PIU-associated SNPs of PDCD1 (rs7565639, rs6710479, and rs7421861) identified in the present study are located in intron 1, which may be related to transcriptional regulation and gene splicing.32 Owing to proximity to the promoter region, it may affect the expression of the PDCD1 gene and contribute to the development of PIU by controlling the balance of T lymphocyte apoptosis. More studies are, however, needed to clarify the biological mechanisms whereby these SNPs may affect the development of PIU.
The polymorphisms of rs7421861 and rs6710479 in the PDCD1 gene found to be important in our study have also been shown to be involved in the pathogenesis of colorectal cancer, in which PDCD1 plays a negative regulation of T cell activity,19 suggesting that genetic susceptibility to PIU may share biological mechanisms with cancer immunity. The OR value of the rs7421861 AA genotype and A allele in our study were 1.40 and 1.35, while in colorectal cancer, the AG genotype showed an OR value of 1.314. SNP 7565639, which was associated with band keratopathy in our patients, has earlier been shown to have a weak association with autoimmune myasthenia gravis.28 This suggests that rs7565639 may be a common susceptibility site for certain autoimmune diseases, although it did not show a correlation with Wegener’s granulomatosis. More autoimmune diseases need to be tested for this SNP to clarify this discrepancy.
JIA-associated uveitis shows clinical features similar to PIU, including location and nature of the intraocular inflammation. Complicated cataract and band keratopathy are commonly observed in both diseases.33 In this study, we also investigated the association of the tested SNPs with JIA-associated uveitis in Han Chinese but did not detect any significant associations following Bonferroni correction for multiple comparisons. These findings suggest that the two diseases do not share the same genetic background and may indeed be two separate uveitis entities.
This study has several limitations. First, our research only showed a significant association between rs7421861, rs6710479, rs7565639, and the risk of PIU but we did not provide the biological mechanisms explaining these observations. Second, owing to the relatively small number of samples from JIA-associated uveitis patients, we might have missed some associations and further studies using a larger sample size are needed. Third, our population was restricted to Han Chinese and studies in other ethnic groups are needed to confirm our findings. Another limitation is the fact that we only tested SNPs that were earlier shown to be associated with cancer or autoimmune disease and we may have missed associations with other unknown SNPs.
In conclusion, the results of this study showed associations of PDCD1/rs6710479 and rs7421861 with PIU. In addition, a stratified analysis according to the clinical features showed that PDCD1/rs7565639 is associated with band keratopathy in PIU. The results support a genetic association between PDCD1 polymorphisms and susceptibility to PIU in Han Chinese and provides new insights into the pathogenesis of this disease.
References
Guly, C. M. & Forrester, J. V. Investigation and management of uveitis. BMJ (Clin. Res. Ed.) 341, c4976 (2010).
Holland, G. N. & Stiehm, E. R. Special considerations in the evaluation and management of uveitis in children. Am. J. Ophthalmol. 135, 867–878 (2003).
Smith, J. A. et al. Epidemiology and course of disease in childhood uveitis. Ophthalmology 116, 1544–1551 (2009). 51.e1.
Angeles-Han, S. T. & Rabinovich, C. E. Uveitis in children. Curr. Opin. Rheumatol. 28, 544–549 (2016).
Elmore, S. Apoptosis: a review of programmed cell death. Toxicol. Pathol. 35, 495–516 (2007).
Zhang, Q., Lenardo, M. J. & Baltimore, D. 30 Years of NF-kappaB: a blossoming of relevance to human pathobiology. Cell 168, 37–57 (2017).
Oeckinghaus, A. & Ghosh, S. The NF-kappaB family of transcription factors and its regulation. Cold Spring Harb. Perspect. Biol. 1, a000034 (2009).
Bally, A. P. et al. NF-kappaB regulates PD-1 expression in macrophages. J. Immunol. 194, 4545–4554 (2015).
Liang, S. C. et al. Regulation of PD-1, PD-L1, and PD-L2 expression during normal and autoimmune responses. Eur. J. Immunol. 33, 2706–2716 (2003).
Contini, P. et al. Apoptosis of antigen-specific T lymphocytes upon the engagement of CD8 by soluble HLA class I molecules is Fas ligand/Fas mediated: evidence for the involvement of p56lck, calcium calmodulin kinase II, and calcium-independent protein kinase C signaling pathways and for NF-kappaB and NF-AT nuclear translocation. J. Immunol. 175, 7244–7254 (2005).
Nagafuchi, H. et al. Aberrant expression of Fas ligand on anti-DNA autoantibody secreting B lymphocytes in patients with systemic lupus erythematosus: “immune privilege”-like state of the autoreactive B cells. Clin. Exp. Rheumatol. 20, 625–631 (2002).
Wan, B. et al. Aberrant regulation of synovial T cell activation by soluble costimulatory molecules in rheumatoid arthritis. J. Immunol. 177, 8844–8850 (2006).
Pittet, C. L., Newcombe, J., Prat, A. & Arbour, N. Human brain endothelial cells endeavor to immunoregulate CD8 T cells via PD-1 ligand expression in multiple sclerosis. J. Neuroinflammation 8, 155 (2011).
Eftekharian, M. M. et al. Expression analysis of long non-coding RNAs in the blood of multiple sclerosis patients. J. Mol. Neurosci. 63, 333–341 (2017).
Yildir, S. et al. Relation of the Fas and FasL gene polymorphisms with susceptibility to and severity of rheumatoid arthritis. Rheumatol. Int. 33, 2637–2645 (2013).
Newby, P. R. et al. Tag SNP screening of the PDCD1 gene for association with Graves’ disease. Clin. Endocrinol. 67, 125–128 (2007).
Chen, S. et al. The associations between PD-1, CTLA-4 gene polymorphisms and susceptibility to ankylosing spondylitis: a meta-analysis and systemic review. Rheumatol. Int. 36, 33–44 (2016).
Lee, Y. H. & Song, G. G. Associations between the FAS -670 A/G, -1377 G/A, and FASL -844 T/C polymorphisms and susceptibility to systemic lupus erythematosus: a meta-analysis. Clin. Exp. Rheumatol. 34, 634–640 (2016).
Ge, J. et al. Association between co-inhibitory molecule gene tagging single nucleotide polymorphisms and the risk of colorectal cancer in Chinese. J. Cancer Res. Clin. Oncol. 141, 1533–1544 (2015).
Eun, Y. G. et al. Single nucleotide polymorphisms of the Fas gene are associated with papillary thyroid cancer. Auris Nasus Larynx 42, 326–331 (2015).
Read, R. W. et al. Revised diagnostic criteria for Vogt-Koyanagi-Harada disease: report of an international committee on nomenclature. Am. J. Ophthalmol. 131, 647–652 (2001).
Yang, P. et al. Development and evaluation of diagnostic criteria for Vogt-Koyanagi-Harada disease. JAMA Ophthalmol. 136, 1025–1031 (2018).
Criteria for diagnosis of Behcet’s disease. International Study Group for Behcet’s Disease. Lancet 335, 1078–1080 (1990).
Petty, R. E. et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J. Rheumatol. 31, 390–392 (2004).
Abelson, A. K. et al. No evidence of association between genetic variants of the PDCD1 ligands and SLE. Genes Immun. 8, 69–74 (2007).
Pizarro, C. et al. PD-L1 gene polymorphisms and low serum level of PD-L1 protein are associated to type 1 diabetes in Chile. Diabetes Metab. Res. Rev. 30, 761–766 (2014).
Forni, D. et al. A 175 million year history of T cell regulatory molecules reveals widespread selection, with adaptive evolution of disease alleles. Immunity 38, 1129–1141 (2013).
Sakthivel, P., Ramanujam, R., Wang, X. B., Pirskanen, R. & Lefvert, A. K. Programmed Death-1: from gene to protein in autoimmune human myasthenia gravis. J. Neuroimmunol. 193, 149–155 (2008).
Xiang, Q. et al. TNF receptor-associated factor 5 gene confers genetic predisposition to acute anterior uveitis and pediatric uveitis. Arthritis Res. Ther. 15, R113 (2013).
Wei, L. et al. MicroRNA-146a and Ets-1 gene polymorphisms are associated with pediatric uveitis. PLoS ONE 9, e91199 (2014).
Chen, L. et al. Constitutive neuronal expression of the immune regulator, programmed death 1 (PD-1), identified during experimental autoimmune uveitis. Ocul. Immunol. Inflamm. 17, 47–55 (2009).
Majewski, J. & Ott, J. Distribution and characterization of regulatory elements in the human genome. Genome Res. 12, 1827–1836 (2002).
Thorne, J. E., Woreta, F., Kedhar, S. R., Dunn, J. P. & Jabs, D. A. Juvenile idiopathic arthritis-associated uveitis: incidence of ocular complications and visual acuity loss. Am. J. Ophthalmol. 143, 840–846 (2007).
Acknowledgements
We thank all participants involved in the present study. This work was supported by “51282” Project for Henan Medical Science and Technology Innovative Talents, Joint Funds of the National Natural Science Foundation of China U1304812 , Medical Scientific and Technological Project of Henan province 201602092 , Scientific and Technological Project of Henan province 172102310374 , Natural Science Foundation Major International (Regional) Joint Research Project 81720108009, and National Natural Science Foundation Project 81770914.
Author information
Authors and Affiliations
Contributions
T.P. and L.D. made substantial contributions to conception and design. F.L., Q.C., and N.L. made substantial contributions to acquisition of data or analysis and interpretation of data. T.P., Y.L., X.M., and L.S. drafted the article and revised it critically for important intellectual content. P.Y. designed this study. P.Y., A.K., and L.D. gave the final approval of the version to be published. All named authors have agreed to its submission. It is not currently being considered for publication by another journal, and if the paper is accepted it will not subsequently be published in the same or similar form in any language without the consent of publishers.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Pang, T., Du, L., Li, F. et al. Association of apoptosis genes in PDCD1 but not PDCD1LG2, FAS, and FASLG with pediatric idiopathic uveitis in Han Chinese. Pediatr Res 87, 634–638 (2020). https://doi.org/10.1038/s41390-019-0612-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0612-4