Abstract
Background
When compared with infant formula, human milk enhances gastric emptying in preterm infants. Hydrogen peroxide (H2O2) is present in large quantities in human milk that has an antimicrobial role for the mother and infant. In vitro adult rat studies suggest that H2O2 facilitates gastric motor contraction. Hypothesizing that H2O2 enhances gastric motility, we investigated its effects on the newborn rat stomach tissue.
Methods
Rat newborn and adult gastric fundic segments, or their smooth muscle cells, were used to evaluate the muscle response to H2O2 exposure. Tissue expression of Rho kinase 2 (ROCK-2; Western blot), its catalase activity, and H2O2 content (Amplex Red) were measured. H2O2 gastric mucosal diffusion was evaluated with Ussing chambers.
Results
In both newborn and adult rats, H2O2 induced gastric muscle contraction and this response was attenuated by pre-incubation with the antioxidant melatonin. H2O2 passively diffused across the gastric mucosa. Its effect on the muscle was modulated via ROCK-2 activation and inhibited by melatonin.
Conclusion
H2O2, at a concentration similar to that of human milk, promotes gastric motility in the rat. To the extent that the present findings can be clinically extrapolated, the human milk H2O2 content may enhance gastric emptying in neonates.
Similar content being viewed by others
Introduction
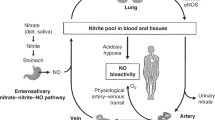
In preterm infants, delayed gastric emptying resulting in feeding intolerance is common and associated with prolonged need for parenteral nutrition.1 The factors contributing to the reduced gastric content clearance in this population are unclear, but are related to the type of milk diet. Infants fed with human milk showed a faster gastric emptying rate, when compared with formula feed.2 Yet, the human milk factor(s) contributing to the enhanced gastric motility remain elusive. One possible such factor is the milk-containing hydrogen peroxide (H2O2).
Human milk has on average H2O2 (10−5 M), a concentration that peaks within days after delivery before declining by the fourth postnatal week.3 In contrast, commercially available infant formule do not contain this metabolite, since they lack xanthine oxidase activity,4 an enzyme responsible for H2O2 generation in human milk.5
In adult rats, H2O2 (10−3 M) potentiates acetylcholine-induced gastric primary smooth muscle cell contraction via a Rho kinase-2 (ROCK-2)-mediated pathway.6 Melatonin, a powerful antioxidant factor, has the opposite effect in the rodent’s bowel by reducing its motor tone.7 These observations suggest that oxidative stress has a direct effect on gastrointestinal motility. To the best of our knowledge, the direct effect of H2O2 on the gastric motor tone has not been investigated. Hypothesizing that H2O2 directly promotes gastric muscle contraction, the main goal of this study was to evaluate the gastric motor effect of this metabolite in the newborn rat and the transduction pathway involved in the potential response.s
Methodology
Design
Studies were conducted in a laboratory setting utilizing newborn and adult rat gastric tissue.
Animals
All procedures were conducted in accordance with the Canadian Animals for Research Act and Canadian Council on Animal Care regulations, and the Hospital for Sick Children Research Institute Animal Care Committee approved the study (Protocol # 41975).
Sprague–Dawley (Charles River, Montreal, QC, Canada) adult (>6 weeks old) and newborn (1–7 days of age) rats were studied. Adult rats were fed a regular rodent diet composed of animal and vegetable protein (Certified Rodent Diet 5002, LabDiet, St. Louis, MO, United States) and housed under standard lighting and temperature conditions.
The animals were sacrificed with pentobarbital sodium injection (60 mg/kg ip). The gastric tissue was removed fresh to be either used for functional studies or snap-frozen in liquid nitrogen immediately after death and stored at −80 °C for <1 month for later processing.
Measurements
All chemicals and reagents were obtained from Sigma-Aldrich (Oakville, ON, Canada), unless otherwise indicated.
Myograph measurements
A single gastric fundic strip was obtained per animal. After retrieval, the fundic strips were maintained in ice-cold Krebs–Henseleit solution (in mM: 115 NaCl, 25 NaHCO3, 138 NaHPO4, 2.51 KCl, 2.46 MgSO4-7H2O, 191 CaCl2, and 5.56 dextrose) bubbled with 95% O2, 5% CO2. The muscle strips were dissected free, end-clamped with flat-surface tissue clips, and submerged into a 10-ml tissue bath (Radnoti, Monrovia, CA) filled with Krebs–Henseleit solution at 37 °C, pH 7.4. One end of the muscle strip was fixed to the bottom of the tissue bath and the top clamp was tied to an isometric force transducer myograph (Harvard Apparatus, Saint Laurent, QC, Canada) using 7-0 braided silk. Isometric changes were digitized and recorded (LabChart Pro, AD Instruments, Colorado
Tissues were bathed in Krebs–Henseleit buffer bubbled with 95% O2, 5% CO2 and maintained at 37 °C. After 1 h of equilibration, the optimal tissue resting tension was determined by repeated stimulation with 128 mM KCl until maximum active tension was reached. All subsequent force measurements were obtained at optimal resting tension.
Muscle contraction potential was evaluated in response to H2O2 and normalized to the maximum force induced by 128 mM KCl. Electrical field stimulation (EFS) was employed to evaluate the neuromuscular-induced force generation, as previously reported.8 In summary, using a commercially available stimulator (Cibertec, Madrid, Spain), the following settings were used: 80 V (voltage) stimulation and 0.5 ms pulses with 20-s trains of at a frequency of 5 Hz. Three stimulations, obtained 10 min apart, were employed and the data wereaveraged to determine the EFS-induced force response.
To evaluate the antioxidant effect on the H2O2-induced contraction, the tissue was pre-incubated with melatonin (10−3 M) for 30 min. Force was normalized to the tissue cross-sectional area (length × diameter), as previously reported for vascular tissue.9,10
Freshly dispersed smooth muscle cells (SMC)
To evaluate the H2O2 effect on the gastric muscle independently of its innervation, and other tissue factors, as well as under more physiologic isotonic conditions, we measured the individual SMC shortening response to this metabolite. The technique was previously described.8 In summary, the gastric tissue was digested in 1 ml/mg collagenase and 0.01% Soybean Trypsin Inhibitor (ThermoFisher, Burlington, Ontario, Canada), and the SMCs were dispersed in DMEM cell culture media (Wisent, St. Bruno, Quebec, Canada). One hour after dispersion, the SMCs were exposed to H2O2 at a final media concentration of 10−4 for either 15 min (shortening measurements) or 6 and 24 h (Western blotting), while maintained at 37 °C and 5% CO2 in a conventional incubator. Following this, the cells were immediately fixed with 1% acrolein. Cells maintained for a similar duration in calcium-free PBS media served as control. Light microscopy images at ×20 magnification were obtained using Leica DM IRE2 microscope (Wetzlar, Germany), and the cells’ lengths were measured using ImageJ (NIH, Bethesda, MA). H2O2-induced cell length changes (shortening) were expressed as percentage of average-control SMC length. The cells were obtained from seven newborns and five adult animals. A minimum of 50 H2O2-exposed and control cells from age group were evaluated.
Western blotting for ROCK-2 content and activity
The cell lysate protein was extracted in 10 mM Tris–HCl, pH 7.4 lysis buffer containing 1% Triton X-100 and protease/phosphatase inhibitor cocktails (Thermo Fisher Scientific Inc., Rockford, IL), and centrifuged at 14,000 × g for 30 min. Protein concentrations were determined via the Bradford assay (Bio-Rad, Mississauga, ON, CA), utilizing bovine serum albumin. Equivalent amounts of lysate proteins in Laemmli buffer were fractionated on SDS–PAGE, transferred to polyvinylidene difluoride membranes, and blotted. Membranes were treated with 5% BSA (Sigma, Oakville, ON, Canada), and exposed at 4 °C overnight for the phosphorylated myosin phosphatase target subunit 1 (pMYPT1;Thr 852, the equivalent of the human Thr 853; 1:500; Santa Cruz, Santa Cruz, CA), and total MYPT1 (1:1000; BD Biosciences, Mississauga, ON) antibodies. Appropriate IgG conjugated with HRP were used as secondary antibodies.
Protein bands were identified using enhanced chemiluminescence (ECL, Perkin Elmer, Shelton, Connecticut), and images were digitally captured using a MicroChemi chemiluminescent system (DNR Bio-imaging systems, Jerusalem, Israel). Bands were quantified by digital densitometry of non-saturated images, with background density removed. After pMYPT1 was detected, membranes were stripped and then reblotted for the normalizer protein total MYPT to account for differences in protein loading.
Band intensities were quantified by Image-J software (National Institutes of Health, Bethesda, MA). ROCK-2 activity was determined as the ratio of phospho-MYPT1/MYPT1 chemiluminescence band intensity. The antioxidant effect of melatonin upon ROCK-2 enzyme activity was evaluated following 24 h co-incubation of H2O2 (10−4 M) with melatonin (10−3 M).
H2O2 content and catalase activity
The tissue and SMC H2O2 content was obtained using Amplex Red reagent in the presence of horseradish peroxidase, and absorption was measured at 571 nm. The catalase inhibitor 3-Amino-1,2,4-triazole (3-AT) was utilized at a concentration of 10−3 M.11
Catalase activity in tissues and cells was measured using Amplex Red Catalase Assay kit (Thermo Fisher Scientific), according to the manufacturer’s instructions. Briefly, tissues were homogenized in 25 mM HEPES buffer, pH 7.4, plus 1 mM EDTA and protease inhibitors. Alternatively, SMCs were lysed in 25 mM HEPES buffer, pH 7.4, plus 1 mM EDTA and protease inhibitors by repeated freeze–thaw cycles. After centrifugation at 6000 × g for 5 min at 4 °C, tissue and cell lysates were incubated with 40 μmol/L H2O2 for 30 min. The non-degraded H2O2 was measured to determine the catalase activity using Amplex Red reagent in the presence of horseradish peroxidase, and absorption was measured at 571 nm. The relative activity was determined according to a standard curve using purified catalase, performed in parallel to the tested samples, and presented as mUnits/ml/mg protein. Data were normalized for tissue protein content.
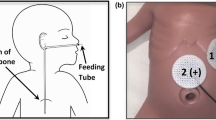
Ussing chambers
Fresh newborn rat gastric tissue was mounted in Ussing chambers (Physiologic Instruments, San Diego) to separate the mucosal and the serosal side. Tissues were incubated in modified Meyler solution at 37 °C in the presence of the catalase inhibitor 3-AT (10−3 M). Mucosal integrity was documented by assessing the transepithelial resistance that was 78 ± 28 Ohm cm2 (N = 5). After equilibration, H2O2 (10−5 M) was added to the mucosal chamber. The H2O2 content of the mucosal and serosal side was measured immediately and 30 min later to determine the mucosal–serosal diffusion of this molecule.
Data analysis
Data were first evaluated to determine Gaussian distribution by Skewness, Kurtosis, and Omnibus testing. Normally distributed data were analyzed by parametric data. Group differences were statistically evaluated by unpaired Student’s t test or two-way analysis of variance (ANOVA) with multiple comparisons obtained by the Tukey–Kramer test. Statistical significance was determined at P < 0.05. All statistical analyses were performed with the Number Cruncher Statistical System software (NCSS, Kaysville, Utah). Data are presented as mean ± SEM.
The sample size utilized for each experiment is listed in the figure legends and refers to tissue or SMC number. As previously stated, only one tissue sample per animal was used for each experiment. Given their high yield for freshly dispersed SMCs, we utilized larger sample sizes, when compared with tissue, in order to minimize the possibility of a type I error. We strived to maximize the sample size and minimize animal utilization according to the Canadian Council on Animal Care guidelines (www.ccac.ca; accessed July 20, 2018). Given that an average rat litter size has 12–15 pups and that they had to be used before 7 days of age, the newborn tissue sample size was larger when compared with the adult counterpart. At least 1000 freshly dispersed SMCs per condition were utilized for the experiments involving ROCK-2 protein expression and activity measurements.
Results
We first evaluated whether H2O2 promotes gastric muscle contraction by measuring its force generation dose response in newborn and adult tissues. At both ages, H2O2 induced a concentration-dependent muscle contraction that was of greater magnitude in the adult, when compared with the newborn gastric strips (Fig. 1a). We previously reported that the rat gastric muscle contraction potential is developmentally regulated and significantly reduced early in life.8 As such, we indexed the gastric motor response data to the tissue-specific KCl-induced response (Fig. 1b). The newborn and adult dose responses overlapped suggesting that the H2O2-induced gastric muscle contraction early in life is limited by its maturational potential, as opposed to a lesser agonist effect in the newborn tissue.
H2O2-induced force dose response of newborn ( < 7 d; N = 27) and adult (N = 7) gastric fundic strips studied in an isometric myograph and normalized to either cross-sectional tissue area (a) or 128 mM KCl-induced stimulation (b). **P < 0.01 when compared with the newborn data by two-way ANOVA and Tukey–Kramer multiple comparison testing. Panel C: H2O2-induced (10−4 M) shortening of newborn ( < 7 d; N = 253) and adult (N = 313) gastric fundus freshly dispersed smooth muscle cells. **P < 0.01 when compared with the newborn values by unpaired Student's t test. Data are Mean ± SE
To further ascertain the H2O2-induced gastric muscle contraction, we comparatively evaluated its response in freshly dispersed newborn and adult SMC (Fig. 1c). H2O2 (10−4 M) induced cell shortening at both ages, the magnitude of which was greater in the adult as compared with the newborn muscle.
We proceeded to assess whether the mechanism responsible for the H2O2-induced gastric muscle contraction relates to its oxidative potential. For this, the newborn gastric tissue H2O2 dose response was measured in the absence and presence of the antioxidant melatonin. Pre-incubation with melatonin (10−3 M) significantly reduced the fundic muscle contraction response to H2O2 (Fig. 2a). To confirm that oxidative stress suppression negatively affects the contraction independently of H2O2, the EFS-induced newborn gastric muscle force was measured in the absence and presence of melatonin (10−3 M). The antioxidant significantly reduced the EFS-induced newborn gastric muscle contraction (Fig. 2b).
a Melatonin (10−3 M) pre-incubation effect on the H2O2-induced force dose response of newborn ( < 7 d) gastric fundic strips studied in an isometric myograph and normalized to 128 mM KCl-induced stimulation. **P < 0.01 when compared with the melatonin data by two-way ANOVA and Tukey–Kramer multiple comparison testing. N = 27 and eight, respectively, for control and melatonin-exposed. b Electrical field stimulation (EFS)-induced gastric fundic motor contraction in the absence and presence of melatonin (10−3 M) in newborn rats' gastric fundic tissue (N = 18). *P < 0.05 when compared with the newborn values by unpaired Student's t test. Data are Mean ± SE
Since others reported that H2O2 promotes ROCK-2 activation in the adult rat stomach,6 we proceeded to evaluate this signaling pathway in the newborn fundic tissue. H2O2 exposure (10−4 M) for 6 h promoted a significant increase in newborn fundic SMC ROCK-2 expression and activity (Fig. 3a, b, respectively). This response was mostly abrogated in the presence of melatonin (10−3 M; c)
Rho kinase 2 (ROCK-2) protein expression (a) and activity (b, c—expressed as the ratio of phosphorylated MYPT/Total MYPT [myosin phosphatase target subunit 1]) in newborn gastric fundus tissue freshly dispersed smooth muscle cells. Panel C shows data relative to ROCK-2 activity of freshly dispersed smooth muscle cells cultured in DMEM media for 24 h in the absence (Control) and presence of either H2O2 (10−4 M) alone or in combination with melatonin (10−3 M). Measurements were obtained from three (a, b) or four (c) distinct cell culture dishes for each condition. **P < 0.01 when compared with time = 0 (a, b) or control (c) by one-way ANOVA and Tukey–Kramer multiple comparison testing. Data are Mean ± SE
As part of cell metabolism, H2O2 is intrinsically generated and thus plays an important physiological role. As such, we further investigated the possible age-dependent differences in its gastric tissue content. Newborn and adult gastric tissue H2O2 content was significantly higher when assayed in the presence of the catalase inhibitor 3-AT, as compared with untreated samples (Fig. 4). Catalase inhibition resulted in an age-dependent difference in H2O2 content measurement, suggesting that the gastric content/activity of this enzyme is maturationally regulated (Fig. 4). Indeed, when compared with the adult values, the newborn gastric tissue and its SMC catalase activities were significantly higher (Fig. 5a, b).
Gastric fundus H2O2 content from newborn and adult rat tissue (N = 3 each). Each tissue was evaluated in the absence and presence of the catalase inhibitor 3-AT (10−3 M). **P < 0.01, when compared with the newborn values by unpaired Student's t test. §P < 0.05 and § §P < 0.01, when compared with the control values by paired Student's t test. Data are Mean ± SE
Lastly, we evaluated passive H2O2 diffusion across the newborn rat gastric mucosa to ascertain if the stomach luminal content of this molecule can reach its muscle layer. Following exposure of the mucosal side to H2O2 in an Ussing chamber, we documented, 30 min later, a statistically significant increase in H2O2 concentration at the serosal/muscular tissue side (Fig. 6).
Discussion
In the present study, we demonstrated that H2O2 passively diffuses across the newborn rat gastric mucosa and promotes muscle contraction via its oxidative properties and ROCK-2 activation. In addition, we showed that when compared with adult rat samples, the newborn gastric tissue H2O2 content was significantly higher suggesting that early in life, the stomach milk content contributes to the tissue level of this metabolite.
Human milk has a relatively high concentration of mammary gland-derived H2O2. Breastfeeding results in a further increase in the milk H2O2 concentration following exposure to the newborn saliva exposure. Al-Shehri et al, reported that the H2O2 concentration of human milk mixed with neonatal saliva is 10−5 M.3
We recently reported that H2O2 in milk is rapidly degraded by the milk-containing catalase and lactoperoxidase enzymes.5 Human milk H2O2 is mostly stable in the acidic range found in the stomach and rapidly degraded at room temperature.5 Thus, the expressed, processed, and stored human milk gavage fed to preterm neonates likely contains lower H2O2 concentrations, when compared to the gastric milk content of breastfed infants.
Human milk feeding enhances gastric emptying2,12 and reduces the duration of parenteral nutrition13 in very low birth weight neonates, when compared with formula-based nutrition. The mechanism supporting the breastmilk advantage is incompletely understood. Although several factors including protein type, degree of hydrolysis14,15, and fortification16,17,18,19 affect the rate of gastric emptying in human milk-fed neonates, the gastrokinetic effect of milk-derived H2O2 has not been previously addressed.
Newborn rodents are suitable animal models to evaluate gastrointestinal motility, since they are developmentally comparable to that of 32-week gestation infants.20 In addition, we recently reported that H2O2 can be retrieved from the newborn rat gastric milk curd, further supporting the use of this animal model to address the study goals.
In the present study, we demonstrated that H2O2 induced gastric fundus muscle contraction in a dose-dependent manner. A significant H2O2-induced force and cell shortening was documented for both newborn and adult-derived gastric wall muscle. That H2O2-promoted SMC shortening not only confirms the tissue strip findings, but also indicates that H2O2 acts directly on the gastric smooth muscle and is not dependent on its innervation and/or other wall-containing factors.
Our findings indicate that gastric muscle contraction was observed at H2O2 concentrations of 10−6 M or higher. These concentrations are in the range that we reported5 for the rat milk H2O2 content (31 ± 3 × 10−6 M). H2O2 is diffusible across cell compartments, and the signaling properties has long been recognized in other organs such as the brain.21 In the present study, we demonstrated that H2O2 could passively diffuse across the newborn rat gastric mucosa, thus enabling it to have a direct effect on the muscle layer. Together, the above evidence strongly suggest that milk-derived H2O2 may facilitate and/or promote newborn gastric motility.
We documented that in the newborn, the H2O2-induced gastric muscle contraction is mediated via the ROCK-2 pathway. Such conclusion is derived from the fact that an in vitro H2O2 exposure for as little as 6 hours significantly increased the ROCK-2 activity, and response was abolished in the presence of the antioxidant melatonin. Such findings confirm similar observations obtained in adult gastric tissue.6
van der Vliet et al.22 showed that in adult rats the gastric mucosal catalase activity is significantly higher, when compared with the intestinal counterpart. In the present study, we showed that a higher gastric catalase activity is present in the newborn, when compared with the adult tissue. The factors accounting for such maturational-dependent pattern is unclear.
It is appealing to speculate that from an evolution point-of-view, the age-dependent difference in gastric tissue catalase activity may reflect the newborn versus adult changes in gastric lumen H2O2 exposure. H2O2 is present in plants23 and other ingestible sources24 that constitute the adult diet. Yet, the higher content of this metabolite in milk may result in greater H2O2 ingestion early in life.
H2O2 has been referred to as a Jekyll and Hyde signaling molecule given its important physiological role at lower concentration, but potentially harmful in certain tissues at higher levels.25 Given the potential H2O2 harmful effects on the gastric epithelium,26 an age-dependent regulation of catalase activity in the gastric wall may allow for its beneficial antimicrobial and gastrokinetic effects while providing a certain degree of tissue protection. That H2O2 is not completely degraded by the tissue catalase activity is evident from the inhibitor-treated samples’ data in Fig. 4. There, we showed not only its presence, but a higher gastric H2O2 content in the newborn, when compared with the adult.
Interestingly, there may be an anatomic region-dependent distinct response to H2O2 in the rat’s gastrointestinal tract. Adult rat intestinal muscle strips pretreated for 30 min with H2O2 (10−3 M) showed impaired methacholine-induced motor contraction.22 At a similar concentration, however, H2O2 enhanced the acetylcholine-induced adult rat gastric muscle contraction.6 The extent to which this anatomic region differences in H2O2 response relate to the tissue catalase content/activity requires further evaluation.
The present study has limitations. All measurements were obtained in vitro from freshly collected gastric tissue samples. We have not proven that milk-derived H2O2 promotes and/or facilitates gastric motility in vivo. Further confirmatory experiments are required to establish H2O2 potential gastric emptying enhancing role in human milk-fed infants. In addition, although statistical significance was demonstrated for all comparative data, the derived conclusions are limited to the present study population. In order to ensure that the observed results can be generalized, future studies addressing a similar experimental design with a priori sample size and power estimations are warranted.
The current findings are of significant clinical translational importance. Feeding intolerance, manifesting as delayed gastric emptying, is commonly observed in preterm neonates resulting in the need for prolonged parenteral nutritional support and its associated risks.1,27 No suitable pharmacological prokinetic agents are available to enhance gastric emptying in these infants. These novel data strongly suggest that human milk-derived H2O2 has a prokinetic gastric motor effect that might account for the enhanced gastric emptying rate documented in nursing infants, when compared with formula-fed neonates.
In conclusion, H2O2 promotes a dose-dependent gastric muscle contraction in newborn rats via its oxidative properties and ROCK-2 activation. Further clinical studies addressing the importance of this molecule in the regulation of gastric emptying early in life is warranted to circumvent enteral feeding intolerance in preterm infants.
References
Fanaro, S. Feeding intolerance in the preterm infant. Early Hum. Dev. 89(Suppl 2), S13–S20 (2013).
Ewer, A. K., Durbin, G. M., Morgan, M. E. & Booth, I. W. Gastric emptying in preterm infants. Arch. Dis. Child Fetal Neonatal Ed. 71, F24–F27 (1994).
Al-Shehri, S. S. et al. Breastmilk-saliva interactions boost innate immunity by regulating the oral microbiome in early infancy. PLoS ONE 10, e0135047 (2015).
Stevens, C. R. et al. Antibacterial properties of xanthine oxidase in human milk. Lancet 356, 829–830 (2000).
Cieslak, M., Ferreira, C. H. F., Shifrin, Y., Pan, J. & Belik, J. Human milk H2O2 content: does it benefit preterm infants? Pediatr. Res. 83, 687–692 (2018).
Al-Shboul, O. & Mustafa, A. Effect of oxidative stress on Rho kinase II and smooth muscle contraction in rat stomach. Can. J. Physiol. Pharmacol. 93, 405–411 (2015).
Bubenik, G. The effect of serotonin, N‐acetylserotonin, and melatonin on spontaneous contractions of isolated rat intestine. J. Pineal Res 3, 41–54 (1986).
Sobchak, C., Fajardo, A. F., Shifrin, Y., Pan, J. & Belik, J. Gastric and pyloric sphincter muscle function and the developmental-dependent regulation of gastric content emptying in the rat. Am. J. Physiol. Gastrointest. Liver Physiol. 310, G1169–G1175 (2016).
Enomoto, M. et al. Newborn rat response to single vs. combined cGMP-dependent pulmonary vasodilators. Am. J. Physiol. Lung Cell Mol. Physiol. 306, L207–L215 (2014).
Enomoto, M., Pan, J., Shifrin, Y. & Belik, J. Age dependency of vasopressin pulmonary vasodilatory effect in rats. Pediatr. Res 75, 315–321 (2014).
De Man, J. G., Moreels, T. G., De Winter, B. Y., Herman, A. G. & Pelckmans, P. A. Pre- and postjunctional protective effect of neocuproine on the nitrergic neurotransmitter in the mouse gastric fundus. Br. J. Pharmacol. 132, 277–285 (2001).
Tomomasa, T. et al. Gastroduodenal motility in neonates: response to human milk compared with cow’s milk formula. Pediatrics 80, 434–438 (1987).
Cristofalo, E. A. et al. Randomized trial of exclusive human milk versus preterm formula diets in extremely premature infants. J. Pediatr. 163, 1592–1595 (2013).
Perrella, S. L., Hepworth, A. R., Simmer, K. N. & Geddes, D. T. Influences of breast milk composition on gastric emptying in preterm infants. J. Pediatr. Gastroenterol. Nutr. 60, 264–271 (2015).
Meyer, R., Foong, R. X., Thapar, N., Kritas, S. & Shah, N. Systematic review of the impact of feed protein type and degree of hydrolysis on gastric emptying in children. BMC Gastroenterol. 15, 137 (2015).
McClure, R. J. & Newell, S. J. Effect of fortifying breast milk on gastric emptying. Arch. Dis. Child Fetal Neonatal Ed. 74, F60–F62 (1996).
Ewer, A. K. & Yu, V. Y. Gastric emptying in pre-term infants: the effect of breast milk fortifier. Acta Paediatr. 85, 1112–1115 (1996).
Yigit, S., Akgoz, A., Memisoglu, A., Akata, D. & Ziegler, E. E. Breast milk fortification: effect on gastric emptying. J. Matern. Fetal Neonatal Med. 21, 843–846 (2008).
Gathwala, G., Shaw, C., Shaw, P., Yadav, S. & Sen, J. Human milk fortification and gastric emptying in the preterm neonate. Int J. Clin. Pract. 62, 1039–1043 (2008).
de, V. P., Soret, R., Suply, E., Heloury, Y. & Neunlist, M. Postnatal development of myenteric neurochemical phenotype and impact on neuromuscular transmission in the rat colon. Am. J. Physiol. Gastrointest. Liver Physiol. 299, G539–G547 (2010).
Kamsler, A. & Segal, M. Hydrogen peroxide as a diffusible signal molecule in synaptic plasticity. Mol. Neurobiol. 29, 167–178 (2004).
van der Vliet, A., Tuinstra, T. J. & Bast, A. Modulation of oxidative stress in the gastrointestinal tract and effect on rat intestinal motility. Biochem. Pharmacol. 38, 2807–2818 (1989).
Cheeseman, J. M. Hydrogen peroxide concentrations in leaves under natural conditions. J. Exp. Bot. 57, 2435–2444 (2006).
Lambert, J. D., Kwon, S. J., Hong, J. & Yang, C. S. Salivary hydrogen peroxide produced by holding or chewing green tea in the oral cavity. Free Radic. Res. 41, 850–853 (2007).
Gough, D. R. & Cotter, T. G. Hydrogen peroxide: a Jekyll and Hyde signalling molecule. Cell Death Dis. 2, e213 (2011).
Paula, A. B. et al. Effects on gastric mucosa induced by dental bleaching–an experimental study with 6% hydrogen peroxide in rats. J. Appl. Oral. Sci. 23, 497–507 (2015).
Bozzetti, V., Tagliabue, P. E., Visser, G. H., van Bel, F. & Gazzolo, D. Feeding issues in IUGR preterm infants. Early Hum. Dev. 89(Suppl 2), S21–S23 (2013).
Acknowledgements
This study was supported by a grant from the Canadian Institutes of Health Research (MOP 133664).
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: A.F.F., C.S., Y.S., J.P., T.G. and J.B. For drafting the article or revising it critically for important intellectual content: A.F.F., T.G. and J.B. For final approval of the version to be published: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fajardo, A.F., Sobchak, C., Shifrin, Y. et al. Hydrogen peroxide promotes gastric motility in the newborn rat. Pediatr Res 84, 751–756 (2018). https://doi.org/10.1038/s41390-018-0154-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0154-1