Abstract
Objective
To determine if maternal cardiac disease affects delivery mode and to investigate maternal morbidity.
Study design
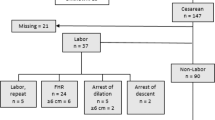
Retrospective cohort study performed using electronic medical record data. Primary outcome was mode of delivery; secondary outcomes included indication for cesarean delivery, and rates of severe maternal morbidity.
Results
Among 14,160 deliveries meeting inclusion criteria, 218 (1.5%) had maternal cardiac disease. Cesarean delivery was more common in women with maternal cardiac disease (adjusted odds ratio 1.63 [95% confidence interval 1.18–2.25]). Patients delivered by cesarean delivery in the setting of maternal cardiac disease had significantly higher rates of severe maternal morbidity, with a 24.38-fold higher adjusted odds of severe maternal morbidity (95% confidence interval: 10.56–54.3).
Conclusion
While maternal cardiac disease was associated with increased risk of cesarean delivery, most were for obstetric indications. Additionally, cesarean delivery in the setting of maternal cardiac disease is associated with high rates of severe maternal morbidity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, Blomstrom-Lundqvist C, Cifkova R, De Bonis M, et al. ESC guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J. 2018;39:3165–241.
Ashrafi R, Curtis SL. Heart disease and pregnancy. Cardiol Ther. 2017;6:157–73.
Elkayam U, Goland S, Pieper PG, Silverside CK. High-risk cardiac disease in pregnancy: part I. J Am Coll Cardiol. 2016;68:396–410.
Elkayam U, Goland S, Pieper PG, Silverside CK. High-risk cardiac disease in pregnancy: part II. J Am Coll Cardiol. 2016;68:502–16.
Fretts RC, Schmittdiel J, McLean FH, Usher RH, Goldman MB. Increased maternal age and the risk of fetal death. N Engl J Med. 1995;333 15:953–7.
Chan A, Wolfe D, Zaidi AN. Pregnancy and congenital heart disease: a brief review of risk assessment and management. Clin Obstet Gynecol. 2020;63:836–51.
Canobbio MM, Warnes CA, Aboulhosn J, Connolly HM, Khanna A, Koos BJ, et al. Management of pregnancy in patients with complex congenital heart disease. Circulation. 2017;135:e50–e87.
Smok DA. Aortopathy in pregnancy. Semin Perinatol. 2014;38:295–303.
Ouzounian JG, Elkayam U. Physiologic changes during normal pregnancy and delivery. Cardiol Clin. 2012;30:317–29.
Nanna M, Stergiopoulos K. Pregnancy complicated by valvular heart disease: an update. J Am Heart Assoc. 2014;3:e000712.
Silversides CK, Grewal J, Mason J, Sermer M, Kiess M, Rychel V, et al. Pregnancy outcomes in women with heart disease: The CARPREG II study. J Am Coll Cardiol. 2018;71:2419–30.
Anon. ACOG practice bulletin No. 212: pregnancy and heart disease. Obstet Gynecol. 2019;133:e320–e356.
Anon. ACOG practice bulletin No 222. Gestational hypertension and preeclampsia. Obstet Gynecol. 2020;135:e237–e260.
Wu P, Haththotuwa R, Kwok CH, Babu A, Kotronias RA, Rushton C, et al. Preeclampsia and future cardiovascular health: a systematic review and meta-analysis. Circulation. 2017;10:e003497.
Roos-Hesselink JW, Ruys TP, Stein JI, Thilen U, Webb GD, Niwa K, et al. Outcome of pregnancy in patients with structural or ischaemic heart disease: results of a registry of the European Society of Cardiology. ROPAC Investigators. Eur Heart J. 2013;34:657–65.
Say L, Chou D, Gemmill A, Tuncalp O, Moller AB, Daniels A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet. Glob Health. 2014;2:e323–e333.
Severe Maternal Morbidity. Centers for Disease Control. Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion. 2020.
Arendt KW, Lindley KJ. Obstetric anesthesia management of the patient with cardiac disease. Int J Obstet Anesth. 2019;37:73–85.
Easter SR, Rouse CE, Duarte V, Hynes JS, Singh MN, Landzberg MJ, et al. Planned vaginal delivery and cardiovascular morbidity in pregnant women with heart disease. Am J Obstet Gynecol. 2020;222:77.e1–77.e11.
Sibai BM. Evaluation and management of severe preeclampsia before 34 weeks’ gestation. SMFM Clin Opin. 2013;203:p191–198.
Malhamé I, Danilack VA, Raker CA, et al. Cardiovascular severe maternal morbidity in pregnant and postpartum women: development and internal validation of risk prediction models. BJOG. 2021;128:922–32.
Ackerman CM, Platner MH, Spatz ES, et al. Severe cardiovascular morbidity in women with hypertensive diseases during delivery hospitalization. Am J Obstet Gynecol. 2019;220:582.e1–582.e11.
Dahlgren LS, Dadelszen PV, Christilaw J, Janssen PA, Lisonkova S, Marquette GP, et al. Caesarean section on maternal request: risks and benefits in healthy nulliparous women and their infants. J Obstet Gynaecol Can. 2009;31:808–17.
Signore C, Klebanoff M. Neonatal morbidity and mortality after elective cesarean delivery. Clin Perinatol. 2008;35:361–71.
Hardee I, Wright L, McCracken C, Lawson E, Oster ME. Maternal and neonatal outcomes of pregnancies in women with congenital heart disease: a meta-analysis. J Am Heart Assoc. 2021;10:e017834.
Ruys TPE, Roos-Hesselink JW, Pijuan-Domenech A, Vasario E, Gaisin IR, Iung B, et al. Is a planned caesarean section in women with cardiac disease beneficial? Heart. 2015;101:530–6.
Safi LM, Tsiaras SV. Update on valvular heart disease in pregnancy. Curr Treat Options Cardio Med. 2017;19:70.
Minhas AS, Rahman F, Gavin N, Cedars A, Vaught AJ, Zakaria S, et al. Cardiovascular and obstetric delivery complications in pregnant women with valvular heart disease. Am J Cardiol. 2021;158:90–97.
Funding
AJV received funding through the Eunice Kennedy Shriver National Institute of Child Health & Human Development Building Interdisciplinary Research in Women’s Health (BIRCWH) Award (K12-HD085845) and the Johns Hopkins University School of Medicine Robert E. Meyerhoff Professorship Award. GS is supported by Blumenthal Scholarship In Preventive Cardiology. AM was supported by the National Heart, Lung, and Blood Institute training grant T32HL007024, the Lou and Nancy Grasmick Endowed Research Fellowship and the Marie-Josée and Henry R. Kravis Endowed Fellowship. JJF was supported by the National Center for Advancing Translational Sciences via award TL1TR002555.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study. JF performed the statistical analyses. NG and KD drafted the manuscript and NG, JV and JF revised it. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gavin, N.R., Federspiel, J.J., Boyer, T. et al. Mode of delivery among women with maternal cardiac disease. J Perinatol 43, 849–855 (2023). https://doi.org/10.1038/s41372-023-01625-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01625-4
This article is cited by
-
Cardio-Obstetrics: A Focused Review
Current Cardiology Reports (2023)
-
Neuraxial Anesthesia in High-Risk Cardiac Patients
Current Anesthesiology Reports (2023)