Abstract
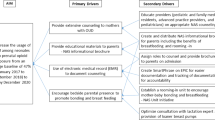
Objective
To describe factors impacting receipt of mother’s own milk (MOM) at discharge among California infants diagnosed with neonatal abstinence syndrome (NAS).
Study Design
Cohort study of the California Perinatal Quality Care Collaborative’s Maternal Substance Exposure Database for infants with NAS and gestational age ≥ 34 weeks from 2019 to 2020.
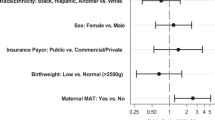
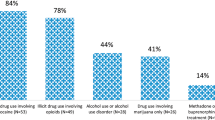
Result
245 infants with NAS were identified. Variables with an increased likelihood of being discharged on MOM included maternal medication assisted treatment (p = 0.001), use of maternal addiction services (p < 0.001), receiving donor human milk (p = 0.001), being treated in the well baby unit (p < 0.001), rooming-in (p < 0.001), and kangaroo care (p < 0.001). Among infants with NAS for whom MOM was recommended (n = 84), rooming-in was the only factor associated with being discharged on MOM (p = 0.002); receiving formula was the only inversely associated factor (p < 0.001).
Conclusion
Results suggest supporting the mother-infant dyad and using non-pharmacologic treatment methods, such as rooming-in, increase receipt of MOM at discharge.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data for this study are not publicly available due to data use agreements with participating hospitals. Elements of the data can be made accessible based on purpose with appropriate permissions based on request to the authors.
References
Stover MW, Davis JM. Opioids in pregnancy and neonatal abstinence syndrome. Semin Perinatol. 2015;39:561–5.
Haight SC, Ko JY, Tong VT, Bohm MK, Callaghan WM. Opioid Use disorder documented at delivery hospitalization—United States, 1999–2014. MMWR Morb Mortal Wkly Rep. 2018;67:845–9.
Patrick SW, Barfield WD, Poindexter BB, COMMITTEE ON, FETUS AND. NEWBORN, COMMITTEE ON SUBSTANCE USE AND PREVENTION. Neonatal opioid withdrawal syndrome. Pediatrics 2020;146:e2020029074.
Reece-Stremtan S, Marinelli KA. The academy of breastfeeding medicine. ABM Clinical Protocol #21: Guidelines for breastfeeding and substance use or substance use disorder, revised 2015. Breastfeed Med. 2015;10:135–41.
Walsh MC, Crowley M, Wexelblatt S, Ford S, Kuhnell P, Kaplan HC, et al. Ohio perinatal quality collaborative improves care of neonatal narcotic abstinence syndrome. Pediatrics 2018;141:e20170900.
Committee Opinion No. 711 Summary. Opioid use and opioid use disorder in pregnancy. Obstet Gynecol. 2017;130:488–9.
Clark RRS. Breastfeeding in women on opioid maintenance therapy: A review of policy and practice. J Midwifery Women’s Health. 2019;64:545–58.
Graves LE, Turner S, Nader M, Sinha S. Breastfeeding and opiate substitution therapy: Starting to understand infant feeding choices. Subst Abuse Res Treat. 2016 ;10s1:SART.S34553.
Tsai LC, Doan TJ. Breastfeeding among mothers on opioid maintenance treatment: A literature review. J Hum Lact. 2016;32:521–9.
Wachman EM, Byun J, Philipp BL. Breastfeeding Rates Among Mothers of Infants with Neonatal Abstinence Syndrome. Breastfeed Med. 2010;5:159–64.
Office of the Surgeon General (US), Centers for Disease Control and Prevention (US), Office on Women’s Health (US). The Surgeon General’s Call to Action to Support Breastfeeding. Rockville (MD): Office of the Surgeon General (US); 2011 [cited 2021 Aug 25]. (Publications and Reports of the Surgeon General). Available from: http://www.ncbi.nlm.nih.gov/books/NBK52682/
Pritham UA. Breastfeeding promotion for management of neonatal abstinence syndrome. J Obstet Gynecol Neonatal Nurs. 2013;42:517–26.
Shukla S, Hanna I, Cortez J, Mansour M, Eiges A, Sharma P, et al. Increasing usage of mother’s own milk in neonates at risk of neonatal abstinence syndrome: MOM-NAS quality improvement initiative. J Perinatol. 2021;41:2684–9.
Grossman MR, Lipshaw MJ, Osborn RR, Berkwitt AK. A novel approach to assessing infants with neonatal abstinence syndrome. Hosp Pediatr. 2018;8:1–6.
Wei T, Simko V R package “corrplot”: Visualization of a Correlation Matrix (Version 0.88). 2021. Available from: https://github.com/taiyun/corrplot
MacMillan KDL, Rendon CP, Verma K, Riblet N, Washer DB, Volpe Holmes A. Association of rooming-in with outcomes for neonatal abstinence syndrome: A systematic review and meta-analysis. JAMA Pediatr. 2018;172:345.
Holmes AV, Atwood EC, Whalen B, Beliveau J, Jarvis JD, Matulis JC, et al. Rooming-in to treat neonatal abstinence syndrome: improved family-centered care at lower cost. PEDIATRICS 2016;137:e20152929.
Pandey R, Kanike N, Ibrahim M, Swarup N, Super DM, Groh-Wargo S, et al. Lactose-free infant formula does not change outcomes of neonatal abstinence syndrome (NAS): A randomized clinical trial. J Perinatol. 2021;41:598–605.
Kaplan HC, Kuhnell P, Walsh MC, Crowley M, McClead R, Wexelblatt S, et al. Orchestrated testing of formula type to reduce length of stay in neonatal abstinence syndrome. Pediatrics 2020;146:e20190914.
Lembeck AL, Tuttle D, Locke R, Lawler L, Jimenez P, Mackley A, et al. Breastfeeding and formula selection in neonatal abstinence syndrome. Am J Perinatol. 2020;s-0040-1713754.
O’Connor AB, Collett A, Alto WA, O’Brien LM. Breastfeeding rates and the relationship between breastfeeding and neonatal abstinence syndrome in women maintained on buprenorphine during pregnancy. J Midwifery Women’s Health. 2013;58:383–8.
Welle-Strand GK, Skurtveit S, Jansson LM, Bakstad B, Bjarkø L, Ravndal E. Breastfeeding reduces the need for withdrawal treatment in opioid-exposed infants. Acta Paediatr. 2013;n/a-n/a.
Holmes AP, Schmidlin HN, Kurzum EN. Breastfeeding considerations for mothers of infants with neonatal abstinence syndrome. Pharmacother J Hum Pharmacol Drug Ther. 2017;37:861–9.
Demirci JR, Bogen DL, Klionsky Y. Breastfeeding and methadone therapy: The maternal experience. Subst Abus. 2015;36:203–8.
Sachs HC. The transfer of drugs and therapeutics into human breast milk: An update on selected topics. Pediatrics 2013;132:e796.
Kantorowska A, Wei JC, Cohen RS, Lawrence RA, Gould JB, Lee HC. Impact of donor milk availability on breast milk use and necrotizing enterocolitis rates. Pediatrics 2016;137:e20153123.
Parker MG, Burnham LA, Kerr SM, Belfort MB, Perrin MT, Corwin MJ, et al. National prevalence of donor milk use among level 1 nurseries. Hosp Pediatr. 2020;10:1078–86.
Recto P, McGlothen-Bell K, McGrath J, Brownell E, Cleveland LM. The role of stigma in the nursing care of families impacted by neonatal abstinence syndrome. Adv Neonatal Care. 2020;20:354–63.
Atkins DN, Durrance CP. State policies that treat prenatal substance use as child abuse or neglect fail to achieve their intended goals: Study examines the effect of state policies that treat prenatal substance use as child abuse or neglect on the incidence of neonatal abstinence syndrome and other factors. Health Aff (Millwood). 2020;39:756–63.
Clemans-Cope L, Holla N, Lee HC, Cong AS, Castro R, Chyi L, et al. Neonatal abstinence syndrome management in California birth hospitals: results of a statewide survey. J Perinatol. 2020;40:463–72.
Acknowledgements
The authors thank the MatEx participating California NICUs for their enthusiastic dedication in improving the care of substance exposed infants and submitting their data to support a community of learning. The authors also thank Fulani Davis and Janella Parucha at the CPQCC Data Center for their efforts in ensuring the accuracy and clarity of the data.
Author contributions
TTN conceptualized and designed the study, and drafted the initial manuscript; CTN coordinated the study, drafted the initial manuscript, and critically reviewed the manuscript; MKQ developed statistical models for the study, conducted data analyses, and critically reviewed the manuscript; JW, LC, and RC contributed to the study design and critically reviewed the manuscript; AH and PA-J contributed to the study design and critically reviewed the manuscript; HCL contributed to study design, supervised the study team, and critically reviewed the manuscript; and all authors approved the final manuscript as submitted.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nguyen, T.T., Toney-Noland, C., Wong, J. et al. Neonatal abstinence syndrome and mother’s own milk at discharge. J Perinatol 42, 1044–1050 (2022). https://doi.org/10.1038/s41372-022-01430-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01430-5