Abstract
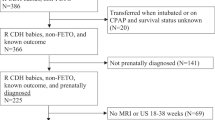
Objective
To evaluate the association between prenatal imaging predictors of patients with left-sided congenital diaphragmatic hernia (LCDH) and postnatal outcomes.
Study design
CDH study group data were reviewed for LCDH infants born 2015–2019. Prenatal ultrasound (US) and magnetic resonance imaging (MRI) data were collected and correlated with postnatal information including CDHSG defect size (A through D or non-repair (NR)).
Results
In total, 929 LCDH patients were included. Both US and MRI imaging predictors correlated with postnatal survival (72.2%) and ECLS use (29.6%). Logistic regression models confirmed increased survival and decreased ECLS use with larger values for all predictors. Importantly, all prenatal values evaluated showed no significant difference between defect size D and NR patients.
Conclusions
This is the largest cohort of LCDH patients and demonstrates that prenatal imaging factors correlate with postnatal outcomes and confirms that patients in the non-repair group are prenatally similar to type D defects.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that supports the findings of this study are available from the corresponding author upon reasonable request.
References
Bianchi DWCT, D’Alton ME, Malone FD, eds. Fetology. 2nd ed. New York, NY: McGraw-Hill; 2010.
Burgos CM, Frenckner B, Luco M, Harting MT, Lally PA, Lally KP. Prenatally versus postnatally diagnosed congenital diaphragmatic hernia—side, stage, and outcome. J Pediatr Surg. 2019;54:651–5.
Jancelewicz T, Brindle ME. Prediction tools in congenital diaphragmatic hernia. Semin Perinatol. 2020;44:151165.
Metkus AP, Filly RA, Stringer MD, Harrison MR, Adzick NS. Sonographic predictors of survival in fetal diaphragmatic hernia. J Pediatr Surg. 1996;31:148–51.
Jani J, Nicolaides KH, Keller RL, Benachi A, Peralta CF, Favre R, et al. Observed to expected lung area to head circumference ratio in the prediction of survival in fetuses with isolated diaphragmatic hernia. Ultrasound Obstet Gynecol. 2007;30:67–71.
Yang SH, Nobuhara KK, Keller RL, Ball RH, Goldstein RB, Feldstein VA, et al. Reliability of the lung-to-head ratio as a predictor of outcome in fetuses with isolated left congenital diaphragmatic hernia at gestation outside 24-26 weeks. Am J Obstet Gynecol. 2007;197:30.e1–7.
Jani JC, Benachi A, Nicolaides KH, Allegaert K, Gratacos E, Mazkereth R, et al. Prenatal prediction of neonatal morbidity in survivors with congenital diaphragmatic hernia: a multicenter study. Ultrasound Obstet Gynecol. 2009;33:64–9.
Deprest JA, Flemmer AW, Gratacos E, Nicolaides K. Antenatal prediction of lung volume and in-utero treatment by fetal endoscopic tracheal occlusion in severe isolated congenital diaphragmatic hernia. Semin Fetal Neonatal Med. 2009;14:8–13.
Harrison MR, Langer JC, Adzick NS, Golbus MS, Filly RA, Anderson RL, et al. Correction of congenital diaphragmatic hernia in utero, V. Initial clinical experience. J Pediatr Surg. 1990;25:47–55.
Deprest JA, Hyett JA, Flake AW, Nicolaides K, Gratacos E. Current controversies in prenatal diagnosis 4: Should fetal surgery be done in all cases of severe diaphragmatic hernia? Prenat Diagn. 2009;29:15–9.
Oluyomi-Obi T, Kuret V, Puligandla P, Lodha A, Lee-Robertson H, Lee K, et al. Antenatal predictors of outcome in prenatally diagnosed congenital diaphragmatic hernia (CDH). J Pediatr Surg. 2017;52:881–8.
Barnewolt CE, Kunisaki SM, Fauza DO, Nemes LP, Estroff JA, Jennings RW. Percent predicted lung volumes as measured on fetal magnetic resonance imaging: a useful biometric parameter for risk stratification in congenital diaphragmatic hernia. J Pediatr Surg. 2007;42:193–7.
Mayer S, Klaritsch P, Petersen S, Done E, Sandaite I, Till H, et al. The correlation between lung volume and liver herniation measurements by fetal MRI in isolated congenital diaphragmatic hernia: a systematic review and meta-analysis of observational studies. Prenat Diagn. 2011;31:1086–96.
Tsao K, Lally KP. The Congenital Diaphragmatic Hernia Study Group: a voluntary international registry. Semin Pediatr Surg. 2008;17:90–7.
Lally KP, Lasky RE, Lally PA, Bagolan P, Davis CF, Frenckner BP, et al. Standardized reporting for congenital diaphragmatic hernia-an international consensus. J Pediatr Surg. 2013;48:2408–15.
Putnam LR, Harting MT, Tsao K, Morini F, Yoder BA, Luco M, et al. Congenital diaphragmatic hernia defect size and infant morbidity at discharge. Pediatrics. 2016;138:e20162043.
Youden WJ. Index for rating diagnostic tests. Cancer 1950;3:32–5.
Morini F, Valfrè L, Capolupo I, Lally KP, Lally PA, Bagolan P. Congenital diaphragmatic hernia: defect size correlates with developmental defect. J Pediatr Surg. 2013;48:1177–82.
Congenital Diaphragmatic Hernia Study Group. Estimating disease severity of congenital diaphragmatic hernia in the first 5 min of life. J Pediatr Surg. 2001;36:141–5.
Lally KP, Lally PA, Lasky RE, Tibboel D, Jaksic T, Wilson JM, et al. Defect size determines survival in infants with congenital diaphragmatic hernia. Pediatrics. 2007;120:e651–7.
Mullassery D, Ba’ath ME, Jesudason EC, Losty PD. Value of liver herniation in prediction of outcome in fetal congenital diaphragmatic hernia: a systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2010;35:609–14.
Basta AM, Lusk LA, Keller RL, Filly RA. Fetal stomach position predicts neonatal outcomes in isolated left-sided congenital diaphragmatic hernia. Fetal Diagn Ther. 2016;39:248–55.
Cordier AG, Cannie MM, Guilbaud L, De Laveaucoupet J, Martinovic J, Nowakowska D, et al. Stomach position versus liver-to-thoracic volume ratio in left-sided congenital diaphragmatic hernia. J Matern Fetal Neonatal Med. 2015;28:190–5.
Romiti A, Viggiano M, Savelli S, Salvi S, Vicario R, Vassallo C, et al. Comparison of mediastinal shift angles obtained with ultrasound and magnetic resonance imaging in fetuses with isolated left sided congenital diaphragmatic hernia. J Matern Fetal Neonatal Med. 2022;35:269–74.
Abbasi N, Cortes MS, Ruano R, Johnson A, Morgan T, Coleman B, et al. Variability in antenatal prognostication of fetal diaphragmatic hernia across the North American Fetal Therapy Network (NAFTNet). Prenat Diagn. 2020;40:342–50.
Snoek KG, Peters NCJ, van Rosmalen J, van Heijst AFJ, Eggink AJ, Sikkel E, et al. The validity of the observed-to-expected lung-to-head ratio in congenital diaphragmatic hernia in an era of standardized neonatal treatment; a multicenter study. Prenat Diagnosis. 2017;37:658–65.
Mesas Burgos C, Hammarqvist-Vejde J, Frenckner B, Conner P. Differences in outcomes in prenatally diagnosed congenital diaphragmatic hernia compared to postnatal detection: a single-center experience. Fetal Diagnosis Ther. 2016;39:241–7.
Deprest J, Brady P, Nicolaides K, Benachi A, Berg C, Vermeesch J, et al. Prenatal management of the fetus with isolated congenital diaphragmatic hernia in the era of the TOTAL trial. Semin Fetal Neonatal Med. 2014;19:338–48.
Ruano R, Lazar DA, Cass DL, Zamora IJ, Lee TC, Cassady CI, et al. Fetal lung volume and quantification of liver herniation by magnetic resonance imaging in isolated congenital diaphragmatic hernia. Ultrasound Obstet Gynecol. 2014;43:662–9.
Shieh HF, Barnewolt CE, Wilson JM, Zurakowski D, Connolly SA, Estroff JA, et al. Percent predicted lung volume changes on fetal magnetic resonance imaging throughout gestation in congenital diaphragmatic hernia. J Pediatr Surg. 2017;52:933–7.
Akinkuotu AC, Cruz SM, Abbas PI, Lee TC, Welty SE, Olutoye OO, et al. Risk-stratification of severity for infants with CDH: Prenatal versus postnatal predictors of outcome. J Pediatr Surg. 2016;51:44–8.
Werner NL, Coughlin M, Kunisaki SM, Hirschl R, Ladino-Torres M, Berman D, et al. Prenatal and postnatal markers of severity in congenital diaphragmatic hernia have similar prognostic ability. Prenat Diagnosis. 2016;36:107–11.
Harting MT, Hollinger L, Tsao K, Putnam LR, Wilson JM, Hirschl RB, et al. Aggressive surgical management of congenital diaphragmatic hernia: worth the effort?: a multicenter, prospective, cohort study. Ann Surg. 2018;267:977–82.
Sperling JD, Sparks TN, Berger VK, Farrell JA, Gosnell K, Keller RL, et al. Prenatal diagnosis of congenital diaphragmatic hernia: does laterality predict perinatal outcomes? Am J Perinatol. 2018;35:919–24.
DeKoninck P, Gomez O, Sandaite I, Richter J, Nawapun K, Eerdekens A, et al. Right-sided congenital diaphragmatic hernia in a decade of fetal surgery. BJOG. 2015;122:940–6.
Author information
Authors and Affiliations
Consortia
Contributions
Study conception and design: EEP, PAL, MTH, GBM, and KPL; Data acquisition: PAL; Analysis and data interpretation: EEP, MK, and SC; Drafting of the manuscript: EEP, MK, and MTH; Critical revision: PAL, FK, FM, RP, KPVM, MTH, GBM, and KPL.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A list of members and their affiliations appears in the Supplementary Information.
Supplementary information
Rights and permissions
About this article
Cite this article
Perrone, E.E., Karmakar, M., Lally, P.A. et al. Image-based prenatal predictors correlate with postnatal survival, extracorporeal life support use, and defect size in left congenital diaphragmatic hernia. J Perinatol 42, 1195–1201 (2022). https://doi.org/10.1038/s41372-022-01357-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01357-x