Abstract
Background/objective
Many studies have shown that child BMI or weight status tracks over time, but the demographic predictors of high tracking have not been investigated. Our objective was to identify demographic predictors of persistence (duration) of healthy weight and overweight/obesity throughout childhood, and to examine whether tracking was age dependent.
Methods
We conducted secondary data analysis of 4606 children from the Birth cohort and 4983 children from the Kindergarten cohort of the Longitudinal Study of Australian Children with follow-up to age 12/13 and 16/17 years, respectively. Retrospective and prospective tracking were examined descriptively. Time-to-event analysis determined demographic predictors of persistence of healthy weight and overweight/obesity beyond age 4–5 years, after controlling for child BMI z-score. Weight status was determined using WHO methods.
Results
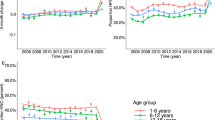
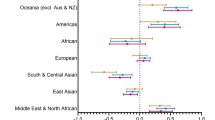
Tracking of healthy weight was consistently higher than that of overweight/obesity, and incident overweight was equally likely throughout childhood and adolescence. Tracking of overweight was lower for children under 7 years than in middle childhood and adolescence (2-year probability 65%, compared with 80%; 2-year resolution of overweight 35 and 20%). Children of lower socioeconomic position, those from culturally and linguistically diverse backgrounds, and girls were more likely to move into overweight (hazard ratios [95%CI] for incident overweight: 1.39 [1.26–1.52], 1.16 [1.02–1.31] and 1.12 [1.02–1.23], respectively) and less likely to resolve their overweight (hazard ratios for resolution of overweight/obesity: 0.77 [0.69–0.85], 0.8 [0.69–0.92] and 0.79 [0.71–0.81], respectively) during childhood. However, persistence of weight status was not significantly affected by rurality or Indigenous status (P > 0.05).
Conclusions
Lowest tracking and highest natural resolution of overweight in children under 7 years suggests this may be an opportune time for interventions to reduce overweight. Primary and secondary prevention programmes during the school years should be designed with special consideration for lower socioeconomic communities, for culturally and linguistically diverse populations and for girls.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–42.
Australian Institute of Health and Welfare. Overweight and obesity: an interactive insight. What is overweight and obesity? Australian Institute of Health and Welfare. (2020). https://www.aihw.gov.au/reports/overweight-obesity/overweight-and-obesity-an-interactive-insight/contents/prevalence.
Hardy LL, Mihrshahi S, Gale J, Drayton BA, Bauman A, Mitchell J. 30-year trends in overweight, obesity and waist-to-height ratio by socioeconomic status in Australian children, 1985 to 2015. Int J Obes. 2005;41:76–82.
Singh AS, Mulder C, JWR Twisk, van Mechelen W, MJM Chinapaw. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9:474–88.
Wheaton N, Millar L, Allender S, Nichols M. The stability of weight status through the early to middle childhood years in Australia: a longitudinal study. BMJ Open. 2015;5. https://bmjopen.bmj.com/content/5/4/e006963.
Magarey AM, Daniels LA, Boulton TJ, Cockington RA. Predicting obesity in early adulthood from childhood and parental obesity. Int J Obes Relat Metab Disord. 2003;27:505–13.
Fuentes RM, Notkola I-L, Shemeikka S, Tuomilehto J, Nissinen A. Tracking of body mass index during childhood: a 15-year prospective population-based family study in eastern Finland. Int J Obes Relat Metab Disord. 2003;27:716–21.
Johannsson E, Arngrimsson SA, Thorsdottir I, Sveinsson T. Tracking of overweight from early childhood to adolescence in cohorts born 1988 and1994: overweight in a high birth weight population. Int J Obes. 2006;30:1265–71.
Department of Social Services, Australian Institute of Family Studies, Australian Bureau of Statisitics. Growing up in Australia: longitudinal study of Australian children (LSAC) release 7.2 (waves 1-7). ADA Dataverse; 2018. https://dataverse.ada.edu.au/dataset.xhtml?persistentId=doi:10.26193/F2YRL5.
Australian Institute of Family Studies. The longitudinal study of Australian children: an Australian government initiative data user guide. Australian Institute of Family Studies; 2018. https://www.aihw.gov.au/getmedia/ac61b7d7-7991-4e15-8fa6-a7973479fa8b/aihw-phe-274.pdf.aspx?inline=true.
WHO. BMI-for-age. WHO. (2021). https://www.who.int/childgrowth/standards/bmi_for_age/en/.
WHO. Growth reference data for 5-19 years. WHO. (2021). https://www.who.int/growthref/en/.
WHO. Application tools. WHO. (2021). http://www.who.int/growthref/tools/en/.
Juonala M, Lau T, Wake M, Grobler A, Kerr JA, Magnussen CG, et al. Early clinical markers of overweight/obesity onset and resolution by adolescence. Int J Obes. 2020;44:82–93.
Ziauddeen N, Roderick PJ, Macklon NS, Alwan NA. Predicting childhood overweight and obesity using maternal and early life risk factors: a systematic review: Predicting childhood overweight. Obes Rev. 2018;19:302–12.
Kerr JA, Long C, Clifford SA, Muller J, Gillespie AN, Donath S, et al. Early-life exposures predicting onset and resolution of childhood overweight or obesity. Arch Dis Child. 2017;102:915–22.
Askie L, Espinoza D, Martin A, Daniels LA, Mihrshahi S, Taylor R, et al. Early prevention of obesity in children (EPOCH)—an individual participant data prospective meta-analysis of four randomised controlled trials: outcomes at 2 years of age. Rochester, NY: Social Science Research Network; 2018. Report no.: ID 3234852. https://papers.ssrn.com/abstract=3234852.
de Wilde JA, Middelkoop B, Verkerk PH. Tracking of thinness and overweight in children of Dutch, Turkish, Moroccan and South Asian descent from 3 through 15 years of age: a historical cohort study. Int J Obes. 2005;42:1230–8.
Cunningham SA, Kramer MR, Narayan KMV. Incidence of childhood obesity in the United States. N Engl J Med. 2014;370:403–11.
Geserick M, Vogel M, Gausche R, Lipek T, Spielau U, Keller E, et al. Acceleration of BMI in early childhood and risk of sustained obesity. N Engl J Med. 2018;379:1303–12.
Baur LA, Garnett SP. Early childhood—a critical period for obesity prevention. Nat Rev Endocrinol. 2019;15:5–6.
McLaren L. Socioeconomic status and obesity. Epidemiol Rev. 2007;29:29–48.
Lobstein T, Baur L, Uauy R. IASO International Obesity TaskForce. Obesity in children and young people: a crisis in public health. Obes Rev. 2004;5:4–104.
Shrewsbury V, Wardle J. Socioeconomic status and adiposity in childhood: a systematic review of cross-sectional studies 1990-2005. Obesity. 2008;16:275–84.
Hardy LL, Jin K, Mihrshahi S, Ding D. Trends in overweight, obesity, and waist-to-height ratio among Australian children from linguistically diverse backgrounds, 1997 to 2015. Int J Obes. 2005;43:116–24.
Cyril S, Nicholson JM, Agho K, Polonsky M, Renzaho AM. Barriers and facilitators to childhood obesity prevention among culturally and linguistically diverse (CALD) communities in Victoria, Australia. Aust N Z J Public Health. 2017;41:287–93.
Scott B, Bolton KA, Strugnell C, Allender S, Marks J. Weight status and obesity-related dietary behaviours among culturally and linguistically diverse (CALD) children in Victoria, Australia. BMC Pediatr. 2019;19:511.
Australian Bureau of Statistics. Main features—key findings. Australian Bureau of Statistics; 2014. https://www.abs.gov.au/ausstats/abs@.nsf/mf/4727.0.55.006.
Anderson DJ, Yoshizawa T. Cross-cultural comparisons of health-related quality of life in Australian and Japanese midlife women: the Australian and Japanese Midlife Women’s Health Study. Menopause. 2007;14:697–707.
Mead E, Batterham AM, Atkinson G, Ells LJ. Predicting future weight status from measurements made in early childhood: a novel longitudinal approach applied to Millennium Cohort Study data. Nutr Diabetes. 2016;6:e200.
Pei Z, Flexeder C, Fuertes E, Thiering E, Koletzko B, Cramer C, et al. Early life risk factors of being overweight at 10 years of age: results of the German birth cohorts GINIplus and LISAplus. Eur J Clin Nutr. 2013;67:855–62.
Veltsista A, Kanaka C, Gika A, Lekea V, Roma E, Bakoula C. Tracking of overweight and obesity in Greek youth. Obes Facts. 2010;3:166–72.
Gardner CD. Preventing weight gain more important than weight loss and more realistic to study in cohorts than in randomized controlled trials. Am J Clin Nutr. 2019;110:544–5.
Partridge SR, Redfern J. Strategies to engage adolescents in digital health interventions for obesity prevention and management. Healthcare. 2018;6:70.
Evensen E, Wilsgaard T, Furberg A-S, Skeie G. Tracking of overweight and obesity from early childhood to adolescence in a population-based cohort—the Tromsø Study: Fit Futures. BMC Pediatr. 2016;16:64.
Buscot M-J, Thomson RJ, Juonala M, Sabin MA, Burgner DP, Lehtimäki T, et al. BMI trajectories associated with resolution of elevated youth bmi and incident adult obesity. Pediatrics. 2018;141:e20172003. https://doi.org/10.1542/peds.2017-200.
Liu Z, Xu H-M, Wen L-M, Peng Y-Z, Lin L-Z, Zhou S, et al. A systematic review and meta-analysis of the overall effects of school-based obesity prevention interventions and effect differences by intervention components. Int J Behav Nutr Phys Act. 2019;16:95.
Yuksel HS, Şahin FN, Maksimovic N, Drid P, Bianco A. School-based intervention programs for preventing obesity and promoting physical activity and fitness: a systematic review. Int J Environ Res Public Health. 2020;17:347. https://doi.org/10.3390/ijerph17010347.
Wang Y, Cai L, Wu Y, Wilson RF, Weston C, Fawole O, et al. What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes Rev. 2015;16:547–65.
Egger G, Swinburn B. An ‘ecological’ approach to the obesity pandemic. BMJ. 1997;315:477–80.
Li L, Hardy R, Kuh D, Lo Conte R, Power C. Child-to-adult body mass index and height trajectories: a comparison of 2 British birth cohorts. Am J Epidemiol. 2008;168:1008–15.
Johnson W, Li L, Kuh D, Hardy R. How has the age-related process of overweight or obesity development changed over time? Co-ordinated analyses of individual participant data from five United Kingdom birth cohorts. PLoS Med. 2015;12:e1001828.
Usback S. The longitudinal study of Australian children. LSAC Technical paper no. 20: wave 7 weighting and non-response: 32. Australian Government Department of Social services: Australian Institute of Family Studies, Canberra.
Acknowledgements
This research is a part of a program of work of the National Health and Medical Research Council Centre of Research Excellence in the Early Prevention of Obesity in Childhood (#1101675). The authors would like to thank the parents and children who took part in the Longitudinal Study of Australian Children, and the Australian Institute of Family Studies for providing the data. JC was supported by a Postgraduate Research Scholarship from The Australian Prevention Partnership Centre. AK was supported by NHMRC PhD scholarship (#1169039).
Author information
Authors and Affiliations
Contributions
AH, LAB and PK conceived the study design. AH, JC and AK carried out data analysis. All authors contributed to data interpretation and the writing and critical review of the final manuscript. All authors have agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hayes, A.J., Carrello, J.P., Kelly, P.J. et al. Looking backwards and forwards: tracking and persistence of weight status between early childhood and adolescence. Int J Obes 45, 870–878 (2021). https://doi.org/10.1038/s41366-021-00751-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00751-3
This article is cited by
-
Differences in weight status among Australian children and adolescents from priority populations: a longitudinal study
International Journal of Obesity (2024)
-
Tracking between cardiovascular-related measures at 4 and 8 years of age in the INMA-Asturias cohort
European Journal of Pediatrics (2023)
-
Tracking of anthropometric characteristics from childhood to adolescence: an 8-year follow-up findings from the Czech ELSPAC study
BMC Public Health (2022)