Abstract
Objective
F13A1/FXIII-A transglutaminase has been linked to adipogenesis in cells and to obesity in humans and mice, however, its role and associated molecular pathways in human acquired excess weight have not been explored.
Methods
We examined F13A1 expression and association to human weight gain in weight-discordant monozygotic twins (Heavy-Lean difference (ΔWeight, 16.8 kg ± 7.16 for n = 12). The twin pairs were examined for body composition (by dual-energy X-ray absorptiometry), abdominal body fat distribution (by magnetic resonance imaging), liver fat content (by magnetic resonance spectroscopy), circulating adipocytokines, leptin and adiponectin, as well as serum lipids. Affymetrix full transcriptome mRNA analysis was performed from adipose tissue and adipocyte-enriched fractions from subcutaneous abdominal adipose tissue biopsies. F13A1 differential expression between the heavy and lean co-twins was examined and its correlation transcriptome changes between co-twins were performed.
Results
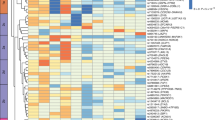
F13A1 mRNA showed significant increase in adipose tissue (p < 0.0001) and an adipocyte-enriched fraction (p = 0.0012) of the heavier co-twin. F13A1 differential expression in adipose tissue (Heavy-Lean ΔF13A1) showed significant negative correlation with circulating adiponectin (p = 0.0195) and a positive correlation with ΔWeight (p = 0.034), ΔBodyFat (0.044) and ΔAdipocyte size (volume, p = 0.012;) in adipocyte-enriched fraction. A whole transcriptome-wide association study (TWAS) on ΔF13A1 vs weight-correlated ΔTranscriptome identified 182 F13A1-associated genes (r > 0.7, p = 0.05) with functions in several biological pathways including cell stress, inflammatory response, activation of cells/leukocytes, angiogenesis and extracellular matrix remodeling. F13A1 did not associate with liver fat accumulation.
Conclusions
F13A1 levels in adipose tissue increase with acquired excess weight and associate with pro-inflammatory, cell stress and tissue remodeling pathways. This supports its role in expansion and inflammation of adipose tissue in obesity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Cristancho AG, Lazar MA. Forming functional fat: a growing understanding of adipocyte differentiation. Nat Rev Mol Cell Biol. 2011;12:722–34.
Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444:840–6.
Datta R, Podolsky MJ, Atabai K. Fat fibrosis: friend or foe? JCI insight. 2018;3:e122289.
Sun K, Kusminski CM, Scherer PE. Adipose tissue remodeling and obesity. J Clin Invest. 2011;121:2094–101.
Rosen ED, Spiegelman BM. What we talk about when we talk about fat. Cell. 2014;156:20–44.
Heinonen S, Jokinen R, Rissanen A, Pietilainen KH. White adipose tissue mitochondrial metabolism in health and in obesity. Obesity Rev. 2020;21:e12958.
Heinonen S, Buzkova J, Muniandy M, Kaksonen R, Ollikainen M, Ismail K, et al. Impaired mitochondrial biogenesis in adipose tissue in acquired obesity. Diabetes. 2015;64:3135–45.
Heinonen S, Muniandy M, Buzkova J, Mardinoglu A, Rodriguez A, Fruhbeck G, et al. Mitochondria-related transcriptional signature is downregulated in adipocytes in obesity: a study of young healthy MZ twins. Diabetologia. 2017;60:169–81.
Naukkarinen J, Surakka I, Pietilainen KH, Rissanen A, Salomaa V, Ripatti S, et al. Use of genome-wide expression data to mine the “Gray Zone” of GWA studies leads to novel candidate obesity genes. PLoS Genet. 2010;6:e1000976.
Heinonen S, Saarinen L, Naukkarinen J, Rodriguez A, Fruhbeck G, Hakkarainen A, et al. Adipocyte morphology and implications for metabolic derangements in acquired obesity. Int J Obes. 2014;38:1423–31.
Muszbek L, Bereczky Z, Bagoly Z, Komaromi I, Katona E. Factor XIII: a coagulation factor with multiple plasmatic and cellular functions. Physiol Rev. 2011;91:931–72.
Mitchell JL, Mutch NJ. Let’s cross-link: diverse functions of the promiscuous cellular transglutaminase factor XIII-A. J. Thromb Haemost. 2019;17:19–30.
Eckert RL, Kaartinen MT, Nurminskaya M, Belkin AM, Colak G, Johnson GV, et al. Transglutaminase regulation of cell function. Physiol Rev. 2014;94:383–417.
Hsieh L, Nugent D. Factor XIII deficiency. Haemophilia. 2008;14:1190–200.
Mousa A, Cui C, Song A, Myneni VD, Sun H, Li JJ, et al. Transglutaminases factor XIII-A and TG2 regulate resorption, adipogenesis and plasma fibronectin homeostasis in bone and bone marrow. Cell Death Differ. 2017;24:844–54.
Mosher DF. Factor XIII and adipocyte biology. Blood. 2014;124:1213–4.
Myneni VD, Hitomi K, Kaartinen MT. Factor XIII-A transglutaminase acts as a switch between preadipocyte proliferation and differentiation. Blood. 2014;124:1344–53.
Myneni VD, Mousa A, Kaartinen MT. Factor XIII-A transglutaminase deficient mice show signs of metabolically healthy obesity on high fat diet. Sci Rep. 2016;6:35574.
Pietilainen KH, Naukkarinen J, Rissanen A, Saharinen J, Ellonen P, Keranen H, et al. Global transcript profiles of fat in monozygotic twins discordant for BMI: pathways behind acquired obesity. PLoS Med. 2008;5:e51.
Kaprio J. Twin studies in Finland 2006. Twin Res Hum Genet. 2006;9:772–7.
Graner M, Seppala-Lindroos A, Rissanen A, Hakkarainen A, Lundbom N, Kaprio J, et al. Epicardial fat, cardiac dimensions, and low-grade inflammation in young adult monozygotic twins discordant for obesity. Am J Cardiol. 2012;109:1295–302.
Naukkarinen J, Heinonen S, Hakkarainen A, Lundbom J, Vuolteenaho K, Saarinen L, et al. Characterising metabolically healthy obesity in weight-discordant monozygotic twins. Diabetologia. 2014;57:167–76.
Pietrobelli A, Formica C, Wang Z, Heymsfield SB. Dual-energy X-ray absorptiometry body composition model: review of physical concepts. Am J Physiol. 1996;271:E941–51.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Ritchie ME, Phipson B, Wu D, Hu Y, Law CW, Shi W, et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43:e47.
Phipson B, Lee S, Majewski IJ, Alexander WS, Smyth GK. Robust hyperparameter estimation protects against hypervariable genes and improves power to detect differential expression. Ann Appl Stat. 2016;10:946–63.
Gentleman RC, Carey VJ, Bates DM, Bolstad B, Dettling M, Dudoit S, et al. Bioconductor: open software development for computational biology and bioinformatics. Genome Biol. 2004;5:R80.
R Core Team (2020) R: A language and environment for statistical computing. Austria, Vienna: R Foundation for Statistical Computing; 2011.
Durinck S, Spellman PT, Birney E, Huber W. Mapping identifiers for the integration of genomic datasets with the R/Bioconductor package biomaRt. Nat Protoc. 2009;4:1184–91.
Jukarainen S, Heinonen S, Ramo JT, Rinnankoski-Tuikka R, Rappou E, Tummers M, et al. Obesity Is Associated With Low NAD(+)/SIRT Pathway Expression in Adipose Tissue of BMI-Discordant Monozygotic Twins. The. J Clin Endocrinol Metab. 2016;101:275–83.
Kaye SM, Pietilainen KH, Kotronen A, Joutsi-Korhonen L, Kaprio J, Yki-Jarvinen H. et al. Obesity-related derangements of coagulation and fibrinolysis: a study of obesity-discordant monozygotic twin pairs. Obesity. 2012;20:88–94.
Pietilainen KH, Ismail K, Jarvinen E, Heinonen S, Tummers M, Bollepalli S, et al. DNA methylation and gene expression patterns in adipose tissue differ significantly within young adult monozygotic BMI-discordant twin pairs. Int J Obes. 2016;40:654–61.
Sahebekhtiari N, Saraswat M, Joenväärä S, Jokinen R, Lovric A, Kaye S, et al. Plasma proteomics analysis reveals dysregulation of complement proteins and inflammation in acquired obesity-A study on rare bmi-discordant monozygotic twin pairs. Proteomics Clin Appl. 2019;13:e1800173.
Reilly SM, Saltiel AR. Adapting to obesity with adipose tissue inflammation. Nat Rev Endocrinol. 2017;13:633–43.
Stolarczyk E. Adipose tissue inflammation in obesity: a metabolic or immune response? Curr Opin Pharmacol. 2017;37:35–40.
Lee BC, Lee J. Cellular and molecular players in adipose tissue inflammation in the development of obesity-induced insulin resistance. Biochim Biophys Acta. 2014;1842:446–62.
Han CY. Roles of reactive oxygen species on insulin resistance in adipose tissue. Diabetes Metab J. 2016;40:272–9.
Chan PC, Hsiao FC, Chang HM, Wabitsch M, Hsieh PS. Importance of adipocyte cyclooxygenase-2 and prostaglandin E2-prostaglandin E receptor 3 signaling in the development of obesity-induced adipose tissue inflammation and insulin resistance. FASEB J. 2016;30:2282–97.
Banhos Danneskiold-Samsøe N, Sonne SB, Larsen JM, Hansen AN, Fjære E, Isidor MS, et al. Overexpression of cyclooxygenase-2 in adipocytes reduces fat accumulation in inguinal white adipose tissue and hepatic steatosis in high-fat fed mice. Sci Rep. 2019;9:8979.
Burhans MS, Hagman DK, Kuzma JN, Schmidt KA, Kratz M. Contribution of adipose tissue inflammation to the development of type 2 diabetes mellitus. Compr Physiol. 2018;9:1–58.
Ruan H, Dong LQ. Adiponectin signaling and function in insulin target tissues. J Mol Cell Biol. 2016;8:101–9.
Stern JH, Rutkowski JM, Scherer PE. Adiponectin, leptin, and fatty acids in the maintenance of metabolic homeostasis through adipose tissue crosstalk. Cell Metab. 2016;23:770–84.
Bagoly Z, Katona E, Muszbek L. Factor XIII and inflammatory cells. Thromb Res. 2012;129:S77–81.
Sun H, Kaartinen MT. Transglutaminases in monocytes and macrophages. Med Sci. 2018;6:115.
Church CD, Berry R, Rodeheffer MS. Isolation and study of adipocyte precursors. Methods Enzymol. 2014;537:31–46.
Orr JS, Kennedy AJ, Hasty AH. Isolation of adipose tissue immune cells. J Visualized Exp. 2013;75:e50707.
Tandon P, Wafer R, Minchin JEN. Adipose morphology and metabolic disease. J Exp Biol. 2018;221(Pt Suppl 1):jeb164970.
Arner E, Westermark PO, Spalding KL, Britton T, Rydén M, Frisén J, et al. Adipocyte turnover: relevance to human adipose tissue morphology. Diabetes. 2010;59:105–9.
Spalding KL, Arner E, Westermark PO, Bernard S, Buchholz BA, Bergmann O, et al. Dynamics of fat cell turnover in humans. Nature. 2008;453:783–7.
Veilleux A, Caron-Jobin M, Noël S, Laberge PY, Tchernof A. Visceral adipocyte hypertrophy is associated with dyslipidemia independent of body composition and fat distribution in women. Diabetes. 2011;60:1504–11.
Aeschlimann D, Mosher D, Paulsson M. Tissue transglutaminase and factor XIII in cartilage and bone remodeling. Semin Thromb Hemost. 1996;22:437–43.
Kopec AK, Abrahams SR, Thornton S, Palumbo JS, Mullins ES, Divanovic S, et al. Thrombin promotes diet-induced obesity through fibrin-driven inflammation. J Clin Invest. 2017;127:3152–66.
Kim I, Kim HG, Moon SO, Chae SW, So JN, Koh KN, et al. Angiopoietin-1 induces endothelial cell sprouting through the activation of focal adhesion kinase and plasmin secretion. Circ Res. 2000;86:952–9.
Christiaens V, Scroyen I, Lijnen HR. Role of proteolysis in development of murine adipose tissue. Thromb Haemost. 2008;99:290–4.
Van Hul M, Frederix L, Lijnen HR. Role of thrombospondin-2 in murine adipose tissue angiogenesis and development. Obesity. 2012;20:1757–62.
Dorgalaleh A, Rashidpanah J. Blood coagulation factor XIII and factor XIII deficiency. Blood Rev. 2016;30:461–75.
Cohen G, Hadas R, Stefania R, Pagoto A, Ben-Dor S, Kohen F, et al. Magnetic resonance imaging reveals distinct roles for tissue transglutaminase and factor XIII in maternal angiogenesis during early mouse pregnancy. Arterioscler Thromb Vasc Biol. 2019;39:1602–13.
Dardik R, Loscalzo J, Inbal A. Factor XIII (FXIII) and angiogenesis. J Thromb Haemost. 2006;4:19–25.
Inbal A, Dardik R. Role of coagulation factor XIII (FXIII) in angiogenesis and tissue repair. Pathophysiol Haemost Thromb. 2006;35:162–5.
Nikolajsen CL, Dyrlund TF, Poulsen ET, Enghild JJ, Scavenius C. Coagulation factor XIIIa substrates in human plasma: identification and incorporation into the clot. J Biol Chem. 2014;289:6526–34.
Wolff G, Taranko AE, Meln I, Weinmann J, Sijmonsma T, Lerch S, et al. Diet-dependent function of the extracellular matrix proteoglycan Lumican in obesity and glucose homeostasis. Mol Metab. 2019;19:97–106.
Taleb S, Lacasa D, Bastard JP, Poitou C, Cancello R, Pelloux V, et al. Cathepsin S, a novel biomarker of adiposity: relevance to atherogenesis. FASEB J. 2005;19:1540–2.
Lafarge JC, Pini M, Pelloux V, Orasanu G, Hartmann G, Venteclef N, et al. Cathepsin S inhibition lowers blood glucose levels in mice. Diabetologia. 2014;57:1674–83.
Acknowledgements
This study was supported by grants to MTK from the Canadian Institutes of Health Research (CIHR) (MOP-119403). MA is supported by an internal stipend, Nyman Award, from the Faculty of Medicine of McGill University. AH is a summer scholar of McGill Initiative in Computational Medicine. AB is supported by Healthy Brains for Healthy Lives initiative at McGill University. SH was supported by Finnish Diabetes Research Foundation, Emil Aaltonen Foundation, Finnish Medical Foundation and Helsinki University Hospital funds. KHP is funded by the Academy of Finland, grant numbers 314383, 266286 and the Academy of Finland, Centre of Excellence in Research on Mitochondria, Metabolism and Disease (FinMIT), grant number 272376; Finnish Medical Foundation; Gyllenberg Foundation; Novo Nordisk Foundation, grant numbers NNF17OC0027232, NNF10OC1013354; Finnish Diabetes Research Foundation; Finnish Foundation for Cardiovascular Research; University of Helsinki, Government Research Funds and Helsinki University Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kaartinen, M.T., Arora, M., Heinonen, S. et al. F13A1 transglutaminase expression in human adipose tissue increases in acquired excess weight and associates with inflammatory status of adipocytes. Int J Obes 45, 577–587 (2021). https://doi.org/10.1038/s41366-020-00722-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-020-00722-0