Abstract
Background/Objectives
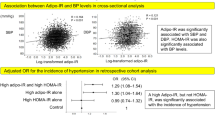
Obesity-associated insulin resistance (IR) may develop in multiple organs, representing different aetiologies towards cardiometabolic diseases. This study aimed to identify distinct plasma lipid profiles in overweight/obese individuals who show muscle-IR and/or liver-IR.
Subjects/Methods
Baseline data of the European multicenter DiOGenes project were used (n = 640; 401 women, nondiabetic BMI: 27-45 kg/m2). Muscle insulin sensitivity index (MISI) and hepatic insulin resistance index (HIRI) were derived from a 5-point oral glucose tolerance test. The 140 plasma lipids were quantified by liquid chromatography–mass spectrometry. Linear mixed models were used to evaluate associations between MISI, HIRI and plasma lipids.
Results
MISI was comparable between sexes while HIRI and triacylglycerol (TAG) levels were lower in women than in men. MISI was associated with higher lysophosphatidylcholine (LPC) levels (standardized (std)β = 0.126; FDR-p = 0.032). Sex interactions were observed for associations between HIRI, TAG and diacylglycerol (DAG) lipid classes. In women, but not in men, HIRI was associated with higher levels of TAG (44 out of 55 species) and both DAG species (stdβ: 0.139–0.313; FDR-p < 0.05), a lower odd-chain/even-chain TAG ratio (stdβ = −0.182; FDR-p = 0.005) and a lower very-long-chain/long-chain TAG ratio (stdβ = −0.156; FDR-p = 0.037).
Conclusions
In overweight/obese individuals, muscle insulin sensitivity is associated with higher plasma LPC concentrations. Women have less hepatic IR and lower TAG than men. Nevertheless, hepatic IR is associated with higher plasma TAG and DAG concentrations and a lower abundance of odd-chain and very-long-chain TAG in women, but not in men. This suggests a more pronounced worsening of plasma lipid profile in women with the progression of hepatic IR.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444:840–6.
Samuel VT, Petersen KF, Shulman GI. Lipid-induced insulin resistance: unravelling the mechanism. Lancet. 2010;375:2267–77.
Valsesia A, Saris WH, Astrup A, Hager J, Masoodi M. Distinct lipid profiles predict improved glycemic control in obese, nondiabetic patients after a low-caloric diet intervention: the Diet, Obesity and Genes randomized trial. Am J Clin Nutr. 2016;104:566–75.
Stinkens R, Goossens GH, Jocken JWE, Blaak EE. Targeting fatty acid metabolism to improve glucose metabolism. Obes Rev. 2015;16:715–57.
Coen PM, Goodpaster BH. Role of intramyocelluar lipids in human health. Trends Endocrinol Metab. 2012;23:391–8.
Tonks KT, Coster AC, Christopher MJ, Chaudhuri R, Xu A, Gagnon-Bartsch J, et al. Skeletal muscle and plasma lipidomic signatures of insulin resistance and overweight/obesity in humans. Obesity. 2016;24:908–16.
Mika A, Sledzinski T. Alterations of specific lipid groups in serum of obese humans: a review. Obes Rev. 2017;18:247–72.
Rauschert S, Uhl O, Koletzko B, Kirchberg F, Mori TA, Huang R-C, et al. Lipidomics reveals associations of phospholipids with obesity and insulin resistance in young adults. J Clin Endocrinol Metab. 2016;101:871–9.
Meikle PJ, Wong G, Barlow CK, Weir JM, Greeve MA, MacIntosh GL, et al. Plasma lipid profiling shows similar associations with prediabetes and type 2 diabetes. PLoS One. 2013;8:e74341–11.
Weir JM, Wong G, Barlow CK, Greeve MA, Kowalczyk A, Almasy L, et al. Plasma lipid profiling in a large population-based cohort. J Lipid Res. 2013;54:2898–908.
Rhee EP, Cheng S, Larson MG, Walford GA, Lewis GD, McCabe E, et al. Lipid profiling identifies a triacylglycerol signature of insulin resistance and improves diabetes prediction in humans. J Clin Invest. 2011;121:1402–11.
Kulkarni H, Meikle PJ, Mamtani M, Weir JM, Almeida M, Diego V, et al. Plasma lipidome is independently associated with variability in metabolic syndrome in Mexican American families. J Lipid Res. 2014;55:939–46.
Barber MN, Risis S, Yang C, Meikle PJ, Staples M, Febbraio MA, et al. Plasma lysophosphatidylcholine levels are reduced in obesity and type 2 diabetes. PLoS ONE. 2012;7:e41456–12.
Floegel A, Stefan N, Yu Z, Mühlenbruch K, Drogan D, Joost H-G, et al. Identification of serum metabolites associated with risk of type 2 diabetes using a targeted metabolomic approach. Diabetes. 2013;62:639–48.
Pietiläinen KH, Sysi-Aho M, Rissanen A, Seppänen-Laakso T, Yki-Jarvinen H, Kaprio J, et al. Acquired obesity is associated with changes in the serum lipidomic profile independent of genetic effects – a monozygotic twin study. PLoS ONE. 2007;2:e218–14.
Stefan N, Fritsche A, Schick F, Häring H-U. Phenotypes of prediabetes and stratification of cardiometabolic risk. Lancet Diabetes Endocrinol. 2016;4:789–98.
Goossens G, Moors C, Jocken J, van der Zijl N, Jans A, Konings E, et al. Altered skeletal muscle fatty acid handling in subjects with impaired glucose tolerance as compared to impaired fasting glucose. Nutrients. 2016;8:164–15.
Bird SR, Hawley JA. Update on the effects of physical activity on insulin sensitivity in humans. BMJ Open Sport Exerc Med. 2016;2:e000143.
Zheng J, Woo S-L, Hu X, Botchlett R, Chen L, Huo Y, et al. Metformin and metabolic diseases: a focus on hepatic aspects. Front Med. 2015;9:173–86.
Blanco-Rojo R, Alcala-Diaz JF, Wopereis S, Perez-Martinez P, Quintana-Navarro GM, Marin C, et al. The insulin resistance phenotype (muscle or liver) interacts with the type of diet to determine changes in disposition index after 2 years of intervention: the CORDIOPREV-DIAB randomised clinical trial. Diabetologia. 2016;59:67–76.
Larsen TM, Dalskov S-M, van Baak M, Jebb SA, Papadaki A, Pfeiffer AFH, et al. Diets with high or low protein content and glycemic index for weight-loss maintenance. N Engl J Med. 2010;363:2102–13.
Abdul-Ghani MA, Matsuda M, Balas B, DeFronzo RA. Muscle and liver insulin resistance indexes derived from the oral glucose tolerance test. Diabetes Care. 2007;30:89–94.
Forouhi NG, Koulman A, Sharp SJ, Imamura F. Differences in the prospective association between individual plasma phospholipid saturated fatty acids and incident type 2 diabetes: the EPIC-InterAct case-cohort study. Lancet Diabetes Endocrinol. 2014;2:810–8.
Goossens GH. The metabolic phenotype in obesity: fat mass, body fat distribution, and adipose tissue function. Obes Facts. 2017;10:207–15.
Wang X, Magkos F, Mittendorfer B. Sex differences in lipid and lipoprotein metabolism: it’s not just about sex hormones. J Clin Endocrinol Metab. 2011;96:885–93.
Kontush A, Lhomme M, Chapman MJ. Unraveling the complexities of the HDL lipidome. J Lipid Res. 2013;54:2950–63.
Ferrannini E, Natali A, Camastra S, Nannipieri M, Mari A, Adam K-P, et al. Early metabolic markers of the development of dysglycemia and type 2 diabetes and their physiological significance. Diabetes. 2013;62:1730–7.
Wang-Sattler R, Yu Z, Herder C, Messias AC, Floegel A, He Y, et al. Novel biomarkers for pre-diabetes identified by metabolomics. Mol Syst Biol. 2012;8:615–11.
Felder TK, Ring-Dimitriou S, Auer S, Soyal SM, Kedenko L, Rinnerthaler M, et al. Specific circulating phospholipids, acylcarnitines, amino acids and biogenic amines are aerobic exercise markers. J Sci Med Sport. 2017;20:700–5.
Klingler C, Zhao X, Adhikary T, Li J, Xu G, Häring H-U, et al. Lysophosphatidylcholines activate PPARδ and protect human skeletal muscle cells from lipotoxicity. Biochim Biophys Acta. 2016;1861:1980–92.
Rzehak P, Hellmuth C, Uhl O, Kirchberg FF, Peissner W, Harder U, et al. Rapid growth and childhood obesity are strongly associated with LysoPC(14:0). Ann Nutr Metab. 2014;64:294–303.
Kim JY, Park JY, Kim OY, Ham BM, Kim H-J, Kwon DY, et al. Metabolic profiling of plasma in overweight/obese and lean men using ultra performance liquid chromatography and Q-TOF mass spectrometry (UPLC-Q-TOF MS). J Proteome Res. 2010;9:4368–75.
Magkos F, Patterson BW, Mohammed BS, Klein S, Mittendorfer B. Women produce fewer but triglyceride-richer very low-density lipoproteins than men. J Clin Endocrinol Metab. 2007;92:1311–8.
Sparks JD, Sparks CE, Adeli K. Selective hepatic insulin resistance, VLDL overproduction, and hypertriglyceridemia. Arterioscler Thromb Vasc Biol. 2012;32:2104–12.
Magkos F, Fabbrini E, Mohammed BS, Patterson BW, Klein S, Mittendorfer B. Estrogen deficiency after menopause does not result in male very-low-density lipoprotein metabolism phenotype. J Clin Endocrinol Metab. 2010;95:3377–84.
Santaren ID, Watkins SM, Liese AD, Wagenknecht LE, Rewers MJ, Haffner SM, et al. Serum pentadecanoic acid (15:0), a short-term marker of dairy food intake, is inversely associated with incident type 2 diabetes and its underlying disorders. Am J Clin Nutr. 2014;100:1532–40.
Yilmaz M, Claiborn KC, Hotamisligil GS. De novo lipogenesis products and endogenous lipokines. Diabetes. 2016;65:1800–7.
Weijers RNM. Lipid composition of cell membranes and its relevance in type 2 diabetes mellitus. Curr Diabetes Rev. 2012;8:390–400.
Holman RT, Adams CE, Nelson RA, Grater S, Jaskiewicz JA, Johnson SB, et al. Patients with anorexia-nervosa demonstrate deficiencies of selected essential fatty-acids, compensatory changes in nonessential fatty-acids and decreased fluidity of plasma-lipids. J Nutr. 1995;125:901–7.
Andersson A, Nälsén C, Tengblad S, Vessby B. Fatty acid composition of skeletal muscle reflects dietary fat composition in humans. Am J Clin Nutr. 2002;76:1222–9.
Author contributions
WHMS and AA designed the DiOGenes clinical study; AV, AA, WHMS and TH designed the lipidomics studies; EEB designed and led the present study; NV and BWvdK conducted the statistical analyses; JWEJ, NV and MMJvG supervised the lipidomics data analyses; BWvdK wrote the manuscript. All authors contributed to revising the article critically for important intellectual content and gave their final approval of the version to be published. EEB is the guarantor of this work.
Funding
This study was supported by the European Commission, Food Quality and Safety Priority of the Sixth Framework Program (FP6-2005-513946), through a grant from the Maastricht University Medical Center and Nestlé Institute of Health Sciences, Lausanne, Switzerland.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
AV is a full-time employee at Nestlé Institute of Health Sciences SA. WHMS reports having received research support from several food companies such as Nestlé, DSM, Unilever, Nutrition et Sante and Danone as well as Pharmaceutical companies such as GSK, Novartis and Novo Nordisk; he is an unpaid scientific advisor for the International Life Science Institute, ILSI Europe. AA reports grants and personal fees from Global Dairy Platform, personal fees from McCain Foods, McDonald’s, Arena Pharmaceuticals Inc., Basic Research, Dutch Beer Knowledge Institute, Netherlands, Gelesis, Novo Nordisk, Denmark, Orexigen Therapeutics Inc., S-Biotek, Denmark, Twinlab and Vivus Inc., grants from Arla Foods, Denmark, Danish Dairy Research Council and Nordea Foundation, Denmark, outside the submitted work, and royalties received for the book first published in Danish as 'Verdens Bedste Kur' (Politiken; Copenhagen, Denmark), and subsequently published in Dutch as 'Het beste dieet ter wereld' (Kosmos Uitgevers; Utrecht/Antwerpen, Netherlands), in Spanish as 'Plan DIOGENES para el control del peso. La dieta personalizada inteligente' (Editorial Evergra ́ficas; Léon, Spain) and in English as 'World’s Best Diet' (Penguin, Australia). EEB receives grant support from food industry such as DSM, Danone, Friesland Campina, Avebe and Sensus, partly within the context of public–private consortia and has received funding from pharmaceutical companies like Novartis. She is involved in several task forces/expert groups related to the International Life Science Institute, ILSI Europe.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
van der Kolk, B.W., Vogelzangs, N., Jocken, J.W.E. et al. Plasma lipid profiling of tissue-specific insulin resistance in human obesity. Int J Obes 43, 989–998 (2019). https://doi.org/10.1038/s41366-018-0189-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0189-8
This article is cited by
-
Hepatic insulin resistance and muscle insulin resistance are characterized by distinct postprandial plasma metabolite profiles: a cross-sectional study
Cardiovascular Diabetology (2024)
-
Body composition and body fat distribution in tissue-specific insulin resistance and in response to a 12-week isocaloric dietary macronutrient intervention
Nutrition & Metabolism (2024)
-
Precision nutrition for targeting pathophysiology of cardiometabolic phenotypes
Reviews in Endocrine and Metabolic Disorders (2023)
-
Metabolic phenotyping in people living with obesity: Implications for dietary prevention
Reviews in Endocrine and Metabolic Disorders (2023)
-
Sexual dimorphism in cardiometabolic health: the role of adipose tissue, muscle and liver
Nature Reviews Endocrinology (2021)