Abstract
Background:
Cases of necrotizing enterocolitis occurring within 48 h of packed red blood cell (PRBC) transfusions are increasingly being described in observational studies. Transfusion-associated gut injury is speculated to result from an abnormal mesenteric vascular response to transfusion. However, the mechanism of disruption of the balance between mesenteric vasoconstriction and relaxation following transfusion is not known.
Methods:
Preterm lambs (n = 16, 134 d gestation; term: 145–147 d) were delivered and ventilated for 24 h. All the lambs received orogastric feeds with colostrum. In addition, 10 of these lambs received PRBC transfusions. Vasoreactivity was evaluated in isolated mesenteric arterial rings using norepinephrine and endothelin-1 as vasoconstrictors. Endothelium-dependent (A23187, a calcium ionophore) and endothelium-independent (SNAP) nitric oxide (NO) donors were used as vasorelaxants. Mesenteric arterial endothelial NO synthase (eNOS), soluble guanylyl cyclase (sGC), and phosphodiesterase 5 (PDE5) mRNA analyses and protein assays were performed.
Results:
Transfusion with PRBC significantly increased mesenteric vasoconstriction to norepinephrine and endothelin-1 and impaired relaxation to A23187 and SNAP. Mesenteric arterial eNOS protein decreased following PRBC transfusion. No significant changes were noted in sGC and PDE5 mRNA or protein assays.
Conclusion:
PRBC transfusion in enterally fed preterm lambs promotes mesenteric vasoconstriction and impairs vasorelaxation by reducing mesenteric arterial eNOS.
Similar content being viewed by others
Main
Necrotizing enterocolitis (NEC) is an acute inflammatory necrosis of the bowel that primarily affects preterm infants and remains a leading cause of morbidity and mortality in the neonatal intensive care unit (1,2). Risk factors for NEC include prematurity, intestinal ischemia, delayed enteral feeds, formula feeding, and bacterial stasis. Many studies have linked abnormalities in the intestinal circulation to NEC. An increased incidence of NEC has been noted in babies with left-sided obstructive heart lesions (3). High superior mesenteric artery vascular resistance has been noted in preterm babies who later developed NEC (4). The finding of coagulation necrosis in intestinal specimens obtained at autopsy confirms the role of intestinal ischemia in the pathogenesis of NEC (5).
The newborn intestinal circulation is regulated by a dynamic balance between constrictor (such as catecholamines and endothelin) and dilator (such as nitric oxide (NO)) stimuli. Under steady-state conditions, the balance favors vasodilation due to the abundant production of endothelium-derived NO (6). Disruption of endothelial function may alter this fine balance, favoring constriction that leads to intestinal ischemia and injury.
In the past 3 years, many observational studies have described a temporal association between packed red blood cell transfusions (PRBC) and the development of NEC in very low birth weight neonates (7,8,9,10,11). One of the hypotheses proposed for transfusion-associated gut injury (TRAGI) (7) is a failure of postprandial increase in mesenteric blood flow following a transfusion. In addition, a state of physiological anemia in very low birth weight infants may compromise gut mucosal integrity and predispose them to NEC (12,13). Many institutions have adopted strategies such as withholding enteral feeds before, during, and after PRBC transfusion to prevent TRAGI (14). Withholding enteral nutrition for a prolonged period of time further impairs caloric intake and growth in preterm infants. Understanding its pathogenesis will enable the neonatal provider to develop protocols that reduce the risk of TRAGI without compromising neonatal nutrition.
Our objective was to evaluate changes in mesenteric vascular reactivity and its mediator pathways after PRBC transfusions in enterally fed preterm lambs. We hypothesized that PRBC transfusions would alter mesenteric vasoreactivity in preterm lambs fed expressed breast milk. We evaluated the contractile response of isolated ovine mesenteric arteries to constrictor agents, norepinephrine (NE), and endothelin-1 (ET-1), as well as their relaxation responses to NO donors A23187 (calcium ionophore) and S-nitroso-penicillamine (SNAP). To our knowledge, this is the first study evaluating changes in mesenteric vasoreactivity following transfusion in a preterm, large mammalian model. In addition, we measured the expression of adrenergic and endothelin receptors as well as enzymes of the NO-cyclic guanosine monophosphate pathway in small mesenteric arteries isolated from preterm lambs.
Results
Hematocrits were obtained within the first hour of life and at the end of the 24 h experiment in our transfused animals. The initial hematocrit was 37 ± 9.3% and final hematocrit was 31.9 ± 8.2%. None of the lambs became polycythemic after transfusion, with the maximum hematocrit being 40%.
Isolated Vessel Constriction Responses
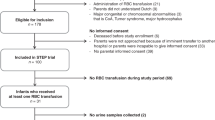
Mesenteric arterial rings (five to six rings per lamb) were isolated from 16 preterm lambs and used for different protocols. All mesenteric arterial rings constricted in a concentration-dependent manner to NE and ET-1 ( Figure 1 ).
Constriction response of ovine mesenteric arteries. (a) Constriction to norepinephrine. Effect of packed red blood cell transfusions on preterm ovine mesenteric artery constriction response to norepinephrine. (b) Constriction to endothelin-1. Preterm fed group (n = 6 lambs) represented by closed squares and fed/transfused group by open circles (n = 10 lambs). *P < 0.05, compared with fed group by ANOVA-repeated measures.
The mesenteric arterial rings isolated from lambs following feeding and PRBC transfusion had significantly increased constriction response to NE ( Figure 1a ) and ET-1 ( Figure 1b ) compared with the preterm fed lambs that were not transfused. Transfusion with PRBC did not alter constriction to potassium chloride ( Figure 2a ).
Constriction response of ovine mesenteric arteries to KCl and LNA. (a) Constriction to potassium (KCl). Effect of enteral feeds and transfusions on preterm ovine mesenteric artery constriction response to 118 mmol/l KCl. (b) Constriction to L-nitroarginine (LNA). Enhancement of norepinephrine (NE)-induced constriction response by pretreatment with 10−3 LNA. Preterm fed group (n = 6) and fed/transfused group (n = 9 for KCl studies and n = 7 for LNA studies).
Increase in NE-induced contractility following inhibition of NO synthase (NOS) was measured to estimate the basal NOS activity in the mesenteric artery (MA). Inhibition of NOS by pretreatment with L-nitroarginine (LNA) enhanced constriction to NE in the fed group of preterm lambs. In sharp contrast, inhibition of NOS by LNA did not enhance constriction to NE following transfusion suggesting an impairment of basal NOS activity ( Figure 2b ). However, this difference in NE constriction in response to LNA between fed and fed/transfused lambs did not reach statistical significance.
Isolated Vessel Relaxation Responses
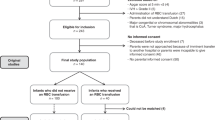
Transfusion with PRBCs impaired relaxation to A23187 in preterm lamb MAs as compared with the enterally fed preterm group ( Figure 3a ). Relaxation to the NO donor SNAP was also significantly impaired by administration of PRBCs ( Figure 3b ).
Relaxation response of ovine mesenteric arteries to nitric oxide donors. (a) Relaxation to A23187. Effect of enteral feeds and transfusions on preterm ovine mesenteric artery relaxation response to nitric oxide donor A23187. (b) Relaxation to SNAP. Preterm fed group (n = 6) represented by closed squares and fed/transfused group (n = 10) by open circles. *P < 0.05 by repeated-measures ANOVA as compared with fed group. SNAP, S-nitroso penicillamine.
mRNA and Protein Assays
Transfusion with PRBCs did not significantly alter adrenergic receptor, (ADRA1A) or endothelin A receptor (ETRA) levels in mesenteric arteries isolated from preterm lambs ( Figure 4a ). Transfusion with PRBCs reduced endothelial NO synthase (eNOS) mRNA levels in mesenteric arteries ( Figure 5a ); however, this difference did not attain statistical significance. No significant differences were noted in mRNA levels for soluble guanylyl cyclase (sGC) or phosphodiesterase 5 (PDE5) between fed and fed-and-transfused preterm lambs ( Figure 5a ).
Reverse-transcriptase PCR mRNA analysis for constrictors: α-adrenergic receptor 1A (ADRA1A) and endothelin receptor A (ETRA) compared with 134-d preterm ovine fetus. Preterm fed group (n = 4) represented in white and fed/transfused group (n = 10) in black.
Changes in mRNA and protein expression of enzymes belonging to the nitric oxide (NO) pathway. (a) Real-time PCR assays for NO pathway soluble guanylyl cyclase (sGC), endothelial NO synthase (eNOS), and phosphodiesterase 5 (PDE5) plotted as fold change compared with 134-d preterm ovine fetus. (b) Protein expression for NO pathway eNOS, sGC, and PDE5 in the two groups normalized to actin. Preterm fed group represented in white (n = 4) and fed/transfused group (n = 10) in black. *P < 0.05 by Fisher"s protected least significant difference.
Protein assays for eNOS, sGC, and PDE5 were normalized to actin ( Figure 5b ). PRBC transfusion significantly decreased eNOS protein in MAs. There was no significant difference in PDE5 and sGC protein between the two groups.
Discussion
Transfusion-associated NEC is being increasingly recognized as a distinct entity (11) and is associated with increased need for surgery as well as higher mortality, compared with NEC not associated with PRBC transfusion (8). In the current study, our results suggest that abnormal mesenteric vasoreactivity seen after PRBC transfusion may be secondary to decreased eNOS protein. This alteration of the NO pathway may be one of the potential contributors to TRAGI.
Mesenteric circulation increases blood flow to the intestines following feeds. Transfusion has been shown to impair this postprandial increase in blood flow velocity in the superior MA (15). Circulating catecholamines (16,17), the sympathetic system, and endothelin (6) are considered to be primary constrictors of the mesenteric circulation. Therefore, we used NE and ET-1 as the constricting agents for isolated mesenteric arterial ring studies. Endothelin-1 is considered to be the primary constrictor stimulus in the intestinal circulation (18). Although it exerts its action through two receptors, (ETRA and ETRB), it has been shown that ETRA-induced vasoconstriction exceeds ETRB-generated vasodilation (6). Catecholamines exert their vasoconstrictive effects on circulation through α-adrenergic receptors. Studies have shown that ADRA1A is the predominant receptor in mesenteric circulation in rats, dogs, and humans (19,20,21). In this study, we have demonstrated that both ADRA1A and ETRA are expressed in the preterm mesenteric circulation and mesenteric arteries respond to the agonists of these receptors in a dose-dependent manner. PRBC transfusion does not alter the expression or synthesis of these two receptors in the preterm lamb.
In neonatal intestine, mesenteric vasorelaxation is predominantly mediated by NO derived from eNOS (22). A23187 is a calcium ionophore that stimulates eNOS and increases NO synthesis in endothelium-dependent relaxation of MA. By contrast, SNAP is an endothelium-independent NO donor that releases NO in the mesenteric arterial smooth muscle cell. The constitutive NO production in the vasculature is controlled by the activity of endothelial NOS (23).
Stewart and Zucker reported the effect of blood products on arterial reactivity and intestinal motility almost 100 y ago (24). Packed red blood cells are transfused to increase oxygen delivery to tissues, but, paradoxically, the opposite effect has been noted (25,26). This phenomenon has been attributed to changes in banked blood, (collectively called “storage lesion”) which include reduced RBC deformability, increased red blood cell adhesion and aggregation, prothrombotic effects of transfusions, and nitric oxide deficiency. In our study, PRBC transfusion with blood stored for 7 d decreased mesenteric vasorelaxation and significantly increased vasoconstriction in preterm, ovine MAs. Changes in contractility were observed with pharmacological stimuli such as NE and ET-1 ( Figure 1 ) but not to maximal constriction induced by potassium chloride ( Figure 2a ). In addition, we did not observe changes in adrenergic/endothelin receptors. These findings suggest that transfusion may not structurally change vascular smooth muscle but instead induces functional changes in mediator pathways (such as NO) in mesenteric vasculature.
There are several limitations to this study. Mesenteric vasoreactivity obtained after 24-h ventilation is likely to be different from values obtained from preterm human infants delivered in the early preterm gestational age (GA) and managed for 2–3 wk ex utero in an intensive care setting. Such intensive care management of preterm lambs in a laboratory setting is very expensive and outside the scope of this study. The GA of 134 d in sheep is approximately equivalent to 32–34 wk in humans as pulmonary and gastrointestinal development is delayed in sheep as compared with the humans (27,28). Sangild et al. postulated that 0.88–0.95 gestation in large farm animals such as sheep and pigs is associated with degrees of gastrointestinal immaturity similar to human infants born at 0.7–0.9 gestation (28). Another study looking at the ontogeny of fasting small intestinal motor activity observed that the low-grade activity seen in infants of <30-wk gestation was similar to the disorganized spiking activity observed in sheep from 0.6 to 0.8 of term infants (29,30). On the basis of this literature, we used 134-d lambs, as this age group was comparable with the corrected gestational age of neonates at highest risk for NEC (31–35 wk) (1,23,31). We only evaluated PRBC collected 7 d before study and did not evaluate the effect of fresh PRBC or PRBC stored for >7 d on mesenteric vasoreactivity. One of the limitations of our model is the lack of anemia in our transfused animals. Very low birth weight neonates with chronic anemia constitute the patient population that has been observed to develop TRAGI. We also administered two PRBC transfusions over a 24-h period in an attempt to induce changes in vascular mediators and reactivity. In a clinical setting, it is likely that most anemic preterm babies receive only one transfusion in the time period preceding TRAGI. We evaluated enteral feeds with expressed breast milk from the ewe. The effect of formula feeds (or frozen breast milk) on mesenteric vasoreactivity was not evaluated. Finally, changes in vasoreactivity observed in isolated vessel rings may not be comparable with the changes in in vivo mesenteric vascular resistance and splanchnic blood flow.
We conclude that PRBC transfusions impair the mesenteric vascular NO pathway and disrupt the delicate balance between vasoconstrictors and dilators in preterm neonatal mesenteric circulation (6). Further studies evaluating the association between age of PRBCs, presence of anemia, changes in mesenteric vasoreactivity, and its relationship to changes in in vivo mesenteric vascular resistance are required to understand the pathogenesis of transfusion-associated intestinal injury.
Methods
The protocol was approved by the Institutional Animal Care Committee of the State University of New York at Buffalo. Time-dated Q-fever seronegative pregnant ewes were purchased from Newlife Pasteur Farms (Attica, NY). Pregnant ewes were fasted for 12 h, sedated with intravenous (i.v.) diazepam (0.25–1.5 mg/kg i.v.) and ketamine (4 mg/kg i.v.), intubated, and anesthetized with 2% isoflurane inhalation. Sixteen lambs were delivered by cesarean section at 134 d (0.91 gestation, term ~145–147 d) GA, intubated, and ventilated for 24 h. This GA was chosen based on the available literature showing that in sheep, preterm delivery at 0.88–0.95 gestation is associated with complications and a degree of gastrointestinal immaturity observed in human infants born at 0.7–0.9 gestation (28). A dose of calfactant 3 ml/kg (Infasurf; ONY, Amhers, NY; a gift from Edmund A. Egan) was administered at birth through the endotracheal tube. Lines were placed in the right carotid artery and jugular vein. Lambs were ventilated with 21–30% oxygen for 24 h to maintain Spo2 between 85 and 95% and PaCo2 between 40 and 50 mmHg. Lambs were sedated with i.v. fentanyl at 2 µg/kg/h. If there was evidence of discomfort (tachycardia, increased blood pressure, or excessive movement), additional doses of fentanyl (2–4 µg/kg) or propofol (2 mg/kg) were administered. Intravenous dextrose 10% solution was administered at 100 ml/kg/d. The composition and rate of i.v. fluids were adjusted based on serum electrolyte values. Intravenous fluid rate was reduced after initiation of enteral feeds. After delivery of the lambs, colostrum was expressed from the ewe and stored in the refrigerator for use over the next 24 h. Starting at 6 h of life, feeds of 5 ml/kg expressed colostrum were administered every 3 h through orogastric tube by gravity. In addition to feeds, 10 of the lambs were transfused twice with packed red cells (10 ml/kg, approximate hematocrit—55%), with each transfusion lasting 2 h and taking place within the first 24 h of life. Adult sheep (ewe) PRBCs stored in standard veterinary blood bags in the refrigerator for 7 d were used for transfusion. All lambs were monitored for a period of 24 h before being euthanized by rapid exsanguination under propofol anesthesia. The abdomen was opened and ileum with attached mesentery was excised and placed in warm aerated Krebs solution. Mesenteric arterial rings adjacent to the distal ileum were collected for isolated vessel studies and frozen for mRNA/protein analysis.
Isolated Vessel Studies
The small mesenteric arterial rings (0.5 mm in diameter) were dissected, washed in Krebs solution (composition in mmol/l: NaCl 119, KCl 5.4, CaCl2 2.5, KH2PO4 0.6, MgSO4 1.2, NaHCO3 25, and glucose 11.7), and mounted in vessel baths aerated with 21% O2 and 6% CO2 to give an estimated pH of 7.4, as described previously (32). The vessel rings were stretched in these baths and isometric tension was measured. A continuous recording of isometric force generation was obtained by tying each vessel ring to a force displacement transducer (model UC2; Statham Instruments, Hato Rey, Puerto Rico) that was connected to a recorder (Gould Instrument Systems, Valley View, OH). Mesenteric arterial rings were pretreated with propranolol (10−6mol/l) to block the β-adrenergic receptors and constricted with increasing titrations of either NE (10−8 to 10−5 mol/l) or ET-1 (10−10 to 10−7 mol/l). These vasoconstrictor agents act through α-adrenergic and endothelin-A receptors. Some mesenteric arterial rings (n = 6 lambs in the control group and 7 in the transfused group) were pretreated with L-nitroarginine (LNA (10−3 mol/l), an antagonist of NOS, to decrease baseline NOS activity before constriction with NE. To study relaxation responses, mesenteric arterial rings were preconstricted with an EC50 concentration of NE and relaxed with increasing concentrations of SNAP (10−8 to 10−5 mol/l) or A23187 (10−8 to 10−6 mol/l). Finally, vessel rings were washed multiple times with Krebs solution. Contractile responses to 118 mmol/l of potassium chloride were obtained to induce maximal constriction. The vessel rings were blotted dry and weighed at the end of each experiment. For constriction curves, responses were normalized to tissue weight (grams of force per gram of weight, g/g) against increasing concentrations of the vasoconstrictor agent. Relaxation was expressed as a percentage of EC50 constriction. All drugs were purchased from Sigma Aldrich (St Louis, MO). SNAP was dissolved in a small quantity of dimethyl sulfoxide and subsequently in water. L-nitro arginine was dissolved in warm Krebs solution using sonication. All other drugs were dissolved in water. Experiments were conducted in a dark room as LNA is sensitive to light.
RNA Isolation
Freshly excised MA tissue adjacent to the ileum was flash frozen in liquid nitrogen and stored at −80 °C until ready for use. Tissues were weighed and homogenized on dry ice. RNA was isolated using RNeasy Mini kit (Qiagen, Valencia, CA) with on column DNAase digestion per manufacturer’s protocol. RNA integrity was assessed using Experion Automated Electrophoresis System (BioRad, Hercules, CA). The RQI (RNA Quality Indicator) for all samples analyzed was >6.8.
Quantitative Reverse-Transcriptase PCR. To assess genomic DNA contamination, a no-reverse transcriptase PCR reaction was performed on the native RNA. RNA (500 ng) was reverse transcribed using iScript cDNA synthesis kit (BioRAD). Three reference genes for normalization were chosen using GeNorm (Biogazelle, Zwijnaarde, Belgium)—ribosomal protein subunits 2 (rps2) and 26 (rps26) and adenosine triphosphate synthetase (ATPsynth). PCR primers for genes of interest—eNOS, sGCB1, and PDE5a—have been described previously (33). ETRA and ADRA1A were chosen using Primer-BLAST Primer Design tool (National Center for Biotechnology Information, Bethesda, MD). All products were verified for appropriate size by gel electrophoresis and sequenced to confirm their identity. PCR was performed in a MyiQ thermal cycler (BioRad) at 95 °C for 4 min, then 40 cycles of 95 °C for 30 s, and finally 60 degrees for 1 min. PCR for PDE5a was similarly performed but with an annealing temperature of 46 °C, as described previously (33). Relative expression was normalized to reference genes using 2(-ΔΔ C(T)) method (34). Results were expressed as fold change compared with the values obtained from six fetal lambs killed at birth at the same gestational age.
Western Blot Analysis
Mesenteric arteries were dissected out, flash frozen in liquid nitrogen, and stored at −80 °C until analysis. Tissues were homogenized in liquid nitrogen using a mortar and pestle and protein isolated using PARIS kit (Ambion Life Technologies, Grand Island, NY) per manufacturer’s protocol. Sixty milligram of tissue was processed and supplemented with a protease inhibitor cocktail (Sigma). Protein concentration was determined using protein assay (BioRad). Total protein (60 µg) was separated on 4–20% SDS-polyacrylamide gels (BioRad) and transferred to nitrocellulose membrane (BioRad). The membranes were then cut to allow simultaneous probing with the antibody of interest and normalization protein. Membranes were blocked in tris-buffered saline Tween, supplemented with 5% nonfat dry milk for 1 h and incubated overnight at 4 °C with primary antibody using the following concentrations: mouse anti PDE5 (BD Transduction, San Jose, CA) at 1:333, mouse anti eNOS (BD Transduction) at 1:1,000, anti-rabbit sGCβ1 (Cayman Chemical, Ann Arbor, MI) at 1:500, and mouse anti-actin (Sigma) at 1:2,000, all in blocking buffer. Blots were washed three times in blocking buffer and incubated at room temperature for 1 h, with appropriate horseradish peroxidase-conjugated secondary antibody (Cell Signaling Technology, Danvers, MA) at 1:1,000 in blocking buffer. Blots were washed four times with blocking buffer and developed using enhanced chemiluminescence western blotting substrate (Pierce, Rockford, IL) according to the manufacturer’s protocol. Blots were visualized using a Fuji Intelligent Imager and Fuji LAS-1000 software and analyzed using FluorChem 8900 software (Alpha Innotech, San Leandro, CA). Blots for each protein of interest (eNOS, sGC, and PDE5) and the corresponding actin were visualized simultaneously for analysis.
Statistical Analysis
Comparison between groups in vascular reactivity was analyzed by repeated-measures ANOVA using Statview 4.0 (Abacus Concepts, Berkley, CA). Real-time PCR and western blot data were analyzed by ANOVA with Fisher"s protected least significant difference post hoc testing. Data are presented as mean ± SEM. Significance was accepted at P < 0.05.
Statement of Financial Support
Funded by grant 1R01HD072929-01(to S.L.) from the National Institute of Child Heath and Human Development andthe Buswell grant (to J.N.) from the State University of New York at Buffalo.
Disclosure
No conflicts of interest, financial or otherwise, are declared by the authors.
References
Neu J . Neonatal necrotizing enterocolitis: an update. Acta Paediatr Suppl 2005;94:100–5.
Kafetzis DA, Skevaki C, Costalos C . Neonatal necrotizing enterocolitis: an overview. Curr Opin Infect Dis 2003;16:349–55.
Polin RA, Pollack PF, Barlow B, et al. Necrotizing enterocolitis in term infants. J Pediatr 1976;89:460–2.
Murdoch EM, Sinha AK, Shanmugalingam ST, Smith GC, Kempley ST . Doppler flow velocimetry in the superior mesenteric artery on the first day of life in preterm infants and the risk of neonatal necrotizing enterocolitis. Pediatrics 2006;118:1999–2003.
Ballance WA, Dahms BB, Shenker N, Kliegman RM . Pathology of neonatal necrotizing enterocolitis: a ten-year experience. J Pediatr 1990;117(1 Pt 2):S6–13.
Nankervis CA, Giannone PJ, Reber KM . The neonatal intestinal vasculature: contributing factors to necrotizing enterocolitis. Semin Perinatol 2008;32:83–91.
Blau J, Calo JM, Dozor D, Sutton M, Alpan G, La Gamma EF . Transfusion-related acute gut injury: necrotizing enterocolitis in very low birth weight neonates after packed red blood cell transfusion. J Pediatr 2011;158:403–9.
Christensen RD, Lambert DK, Henry E, et al. Is “transfusion-associated necrotizing enterocolitis” an authentic pathogenic entity? Transfusion 2010;50:1106–12.
Valieva OA, Strandjord TP, Mayock DE, Juul SE . Effects of transfusions in extremely low birth weight infants: a retrospective study. J Pediatr 2009;155:331–37 e1.
McGrady GA, Rettig PJ, Istre GR, Jason JM, Holman RC, Evatt BL . An outbreak of necrotizing enterocolitis. Association with transfusions of packed red blood cells. Am J Epidemiol 1987;126:1165–72.
Amin SC, Remon JI, Subbarao GC, Maheshwari A . Association between red cell transfusions and necrotizing enterocolitis. J Matern Fetal Neonatal Med 2012;25:Suppl 5:85–9.
Singh R, Visintainer PF, Frantz ID 3rd, et al. Association of necrotizing enterocolitis with anemia and packed red blood cell transfusions in preterm infants. J Perinatol 2011;31:176–82.
Singh R, Shah BL, Frantz ID 3rd . Necrotizing enterocolitis and the role of anemia of prematurity. Semin Perinatol 2012;36:277–82.
El-Dib M, Narang S, Lee E, Massaro AN, Aly H . Red blood cell transfusion, feeding and necrotizing enterocolitis in preterm infants. J Perinatol 2011;31:183–7.
Krimmel GA, Baker R, Yanowitz TD . Blood transfusion alters the superior mesenteric artery blood flow velocity response to feeding in premature infants. Am J Perinatol 2009;26:99–105.
Weinmann A, Post M, Pan J, et al. Tetrahydrobiopterin is present in high quantity in human milk and has a vasorelaxing effect on newborn rat mesenteric arteries. Pediatr Res 2011;69:325–9.
Moonen RM, Villamor E . Developmental changes in mesenteric artery reactivity in embryonic and newly hatched chicks. J Comp Physiol B, Biochem Syst Environ Physiol 2011;181:1063–73.
Nankervis CA, Nowicki PT . Role of endothelin-1 in regulation of the postnatal intestinal circulation. Am J Physiol Gastrointest Liver Physiol 2000;278:G367–75.
Martí D, Miquel R, Ziani K, et al. Correlation between mRNA levels and functional role of alpha1-adrenoceptor subtypes in arteries: evidence of alpha1L as a functional isoform of the alpha1A-adrenoceptor. Am J Physiol Heart Circ Physiol 2005;289:H1923–32.
Martínez-Salas SG, Campos-Peralta JM, Pares-Hipolito J, Gallardo-Ortíz IA, Ibarra M, Villalobos-Molina R . Alpha1A-adrenoceptors predominate in the control of blood pressure in mouse mesenteric vascular bed. Auton Autacoid Pharmacol 2007;27:137–42.
Rudner XL, Berkowitz DE, Booth JV, et al. Subtype specific regulation of human vascular alpha(1)-adrenergic receptors by vessel bed and age. Circulation 1999;100:2336–43.
Nankervis CA, Dunaway DJ, Nowicki PT . Determinants of terminal mesenteric artery resistance during the first postnatal month. Am J Physiol Gastrointest Liver Physiol 2001;280:G678–86.
Llanos AR, Moss ME, Pinzòn MC, Dye T, Sinkin RA, Kendig JW . Epidemiology of neonatal necrotising enterocolitis: a population-based study. Paediatr Perinat Epidemiol 2002;16:342–9.
Stewart GN, Zucker TF . A Comparison of the action of plasma and serum on certain objects used in biological tests for epinephrin. J Exp Med 1913;17:152–73.
Reynolds JD, Ahearn GS, Angelo M, Zhang J, Cobb F, Stamler JS . S-nitrosohemoglobin deficiency: a mechanism for loss of physiological activity in banked blood. Proc Natl Acad Sci USA 2007;104:17058–62.
Gladwin MT, Kim-Shapiro DB . Storage lesion in banked blood due to hemolysis-dependent disruption of nitric oxide homeostasis. Curr Opin Hematol 2009;16:515–23.
Dawes G . Foetal and neonatal physiology - a comparative study of the changes at birth. Chicago, USA: Year Book Medical Publishers, 1968.
Sangild PT . Gut responses to enteral nutrition in preterm infants and animals. Exp Biol Med (Maywood) 2006;231:1695–711.
Bisset WM, Watt JB, Rivers RP, Milla PJ . Ontogeny of fasting small intestinal motor activity in the human infant. Gut 1988;29:483–8.
Bueno L, Ruckebusch Y . Perinatal development of intestinal myoelectrical activity in dogs and sheep. Am J Physiol 1979;237:E61–7.
González-Rivera R, Culverhouse RC, Hamvas A, Tarr PI, Warner BB . The age of necrotizing enterocolitis onset: an application of Sartwell’s incubation period model. J Perinatol 2011;31:519–23.
Lakshminrusimha S, Russell JA, Steinhorn RH, et al. Pulmonary arterial contractility in neonatal lambs increases with 100% oxygen resuscitation. Pediatr Res 2006;59:137–41.
Farrow KN, Groh BS, Schumacker PT, et al. Hyperoxia increases phosphodiesterase 5 expression and activity in ovine fetal pulmonary artery smooth muscle cells. Circ Res 2008;102:226–33.
Livak KJ, Schmittgen TD . Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 2001;25:402–8.
Acknowledgements
The authors thank Melissa Carmen for her help during the in vivo studies and in editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nair, J., Gugino, S., Nielsen, L. et al. Packed red cell transfusions alter mesenteric arterial reactivity and nitric oxide pathway in preterm lambs. Pediatr Res 74, 652–657 (2013). https://doi.org/10.1038/pr.2013.153
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2013.153
This article is cited by
-
Fetal and postnatal ovine mesenteric vascular reactivity
Pediatric Research (2016)
-
Arginine depletion increases susceptibility to serious infections in preterm newborns
Pediatric Research (2015)