Abstract
The factors that determine the ability of metastatic tumor cells to expand and grow in specific secondary site(s) are not yet fully understood. Matrix metalloproteinases (MMP) were identified as potential regulators of the site-specificity of metastasis. We found that lung carcinoma cells ectopically expressing high levels of the receptor for the type I insulin like growth factor receptor (M27R cells) had a significant reduction in MMP-3 expression levels and this coincided with reduced metastasis to the lung. We used these cells to further investigate signaling pathways regulating MMP-3 expression and the role that MMP-3 plays in lung metastasis. We show that ectopic IκB kinase ɛ (IKKɛ) expression in these cells partly restored MMP-3 expression levels and also sensitized MMP-3 transcription to induction by phorbol 12-myristate 13-acetate (PMA). This increase in MMP-3 production was due to increased activation of several signal transduction mediators, including protein kinase C alpha, ERK2, Akt and the transcription factor p65. Furthermore, reconstitution of MMP-3 expression in M27R cells restored their ability to colonize the lung whereas silencing of MMP-3 in M27 cells reduced metastases. Collectively, our results implicate IKKɛ as a central regulator of PMA-induced cell signaling and MMP-3 expression and identify MMP-3 as an enabler of tumor cell expansion in the lung.
Similar content being viewed by others
Introduction
The predilection of some cancers to metastasize to specific secondary sites has been recognized for decades and its molecular basis remains the subject of intense investigation.1, 2, 3 Recent evidence suggests that the ultimate site of metastases is regulated by unique gene expression signatures of clonal subpopulations that exist within primary tumors. The genes constituting these distinct signatures generally encode proteins known to mediate cell growth, motility and invasion, implying that different organs have distinct requirements for tumor expansion within their microenvironment.4
The matrix metalloproteinases (MMPs) have been identified in several gene expression signatures associated with site-specific metastasis.1,2 These zinc-dependent peptidases and their endogenous inhibitors, the tissue inhibitors of metalloproteinases (TIMPs), play a central role in the extracellular matrix remodeling required for tumor invasion, expansion, angiogenesis and metastasis, and have also been identified as regulators of tumor survival and growth.4,5 MMP-3 is a 54- kDa stromelysin (stromelysin 1) with a broad substrate specificity that can cleave fibronectin and several collagens. MMP-3 has been implicated in the progression of primary malignancies of the lung,6, 7, 8 but its role in site-specific lung metastasis has not been defined. Huang et al.9 recently identified MMP-3 as one of several proteins that contribute to vascular destabilization in the lung during the pre-metastatic phase of melanoma dissemination.
Under physiological conditions, MMP-3 is produced by several types of cells including fibroblasts and macrophages10 and its expression can be induced by inflammatory mediators such as IL-1 and TNF-α. The MMP-3 promoter contains an AP-1 and a PEA3 binding site that act together to activate MMP-3 transcription.11,12 MMP-3 expression can also be upregulated downstream of NFκB activation.13,14 Interestingly, Borghaei et al.15,16 have also identified a polymorphic site in the MMP-3 promoter to which the NFκB subunits p50 and p65 can bind to inhibit transcription.
IKKɛ is a phorbol 12-myristate 13-acetate (PMA)-inducible IκB kinase (IKK)-related kinase.17,18 Although a homolog of IKKα and IKKβ, its role in signaling in the canonical NFκB pathway, appears to be distinct. Unlike IKKα and IKKβ, which phosphorylate IκBα on serines 32 and 36, resulting in IκBα proteosomal degradation and NFκB activation, IKKɛ phosphorylates IκBα only on Ser36, although it can also phosphorylate Ser32 when PMA-activated.17,19, 20, 21, 22 In some cells, PMA-induced NFκB activation can be blocked by a dominant negative mutant of IKKɛ,17 identifying it as essential for NFκB activation by phorbol esters. IKKɛ can also directly phosphorylate the NFκB subunits cRel23 and p65 and can translocate to the nucleus to co-activate transcription of NFκB-target genes.13 Uniquely to IKKɛ, it has been identified as a central mediator of the interferon response to viral infection.24
Other known substrates of IKKɛ are Akt, a mediator of cell survival,25, 26, 27 and the transcription factor cJun.28 Recently, IKKɛ was identified as an oncogene in breast cancer,29 where it was shown to phosphorylate the tumor suppressor CYLD,30 leading to cellular transformation. Although activation of any of these pathways could contribute to malignant transformation, the contribution of IKKɛ to the metastatic phenotype has not, to date, been elucidated.
The type 1 insulin-like growth factor (IGF) system is known to contribute to malignant transformation and promote tumor progression. Ligand binding to the IGF-I receptor (IGF-IR) activates several signal transduction pathways known to play a role in cellular transformation and maintenance of the malignant phenotype, including the PI3K/Akt and MAPK pathways,31 which are known to be deregulated in multiple cancers. Altered expression of IGF system components can therefore be an initiating event in cellular transformation and/or contribute to cancer progression.32
Previously, we have shown that the overexpression of IGF-IR in murine lung carcinoma M27 cells (M27R cells) altered the metastatic phenotype of the cells, resulting in the acquisition of a liver-colonizing potential.33 As we show here, this was associated with an unexpected loss of the lung-colonizing potential of these cells. Gene expression profiling previously revealed profound changes to expression levels of multiple genes in these cells, including genes coding for MMPs.34 In particular, we found that MMP-3, -9 and -13 levels were significantly reduced and subsequently identified PKC-α downregulation as the major mechanism underlying reduced MMP-9, but not MMP-3 expression.34 Here, we investigated the signaling pathway involved in the downregulation of MMP-3 in M27R cells and evaluated the effect that altered MMP-3 expression has on the metastatic phenotype.
Results
Loss of the lung-metastasizing potential in carcinoma cells ectopically expressing IGF-IR
M27 cells are a non-clonal subline of the Lewis lung carcinoma with high lung-metastasizing potential from primary subcutaneous tumors or following tail vein injection.35 We previously reported that the ectopic expression of hIGF-IR in these cells (M27R) resulted in the acquisition of a liver-metastasizing potential.36 Intriguingly, however, we found that these cells when inoculated via the tail vein, had a markedly reduced ability to colonize the lung, relative to wild-type M27 cells, as reflected in reduced numbers of visible metastases (Figures 1a and b) and lung weights (Figure 1c) and confirmed in formalin-fixed, paraffin-embedded lung sections stained with hematoxylin and eosin (Figure 1d). These results suggested that the ectopic expression of IGF-IR, although providing a growth advantage to these tumor cells in the liver, also impaired their lung-metastasizing ability.
Loss of the lung-metastasizing potential in M27 cells ectopically expressing IGF-IR. Mice were injected via the tail vein with 105 tumor cells and the lungs removed 18 days later and fixed in Bouin’s solution. Shown are the numbers of visible metastases counted on the surface of the lungs (a and b) and lung weights (c). Representative images of hematoxylin and eosin-stained sections prepared from formalin-fixed, paraffin-embedded lung fragments are shown in (d). Mag: images on left- × 50; images on right (enlarged view of same metastases)- × 400. LU: lung. T: tumor. *P<0.001.
Downregulation of IKKɛ in tumor cells with ectopic overexpression of IGF-IR
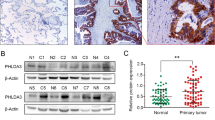
The MMP profiles of tumor cells are known to dictate their ability to invade and expand in a target organ. We previously reported that MMP-3 expression levels in M27R cells were markedly reduced.34 Here, we used these cells to investigate signaling pathways involved in the altered expression of MMP-3 and the link between reduced MMP-3 expression levels and the observed reduction in lung metastasis. Because MMP-3 was shown to be regulated downstream of the NFκB pathway,13 we first compared expression levels of mediators of this pathway in M27 and M27R cells, using reverse transcriptase polymerase chain reaction (RT–PCR) and quantitative real time PCR (qPCR). We found that IKKɛ expression levels but not those of other mediators of the NFκB signaling pathway were significantly downregulated in these cells relative to controls (Figures 2a and b), as was also confirmed by western blotting (Figure 2c).
Tumor cells ectopically expressing IGF-IR have reduced IKKɛ expression levels. Expression of NFκB signal transduction mediators was measured using RT–PCR (a) and for a more selected group qPCR (b). Shown in (a) are representative results of three RT-PCR assays performed and in (b) means and s.d. of results obtained in three separate qPCR assays (each performed in triplicates), normalized to GAPDH and expressed as a ratio relative to wild-type M27 cells that were assigned a value of 1. Shown in (c) are representative results of three immunoblots performed on total cell lysates. *P<0.05.
Constitutive and PMA-inducible MMP-3 expression are restored by reconstitution of IKKɛ expression
We next asked whether reduced IKKɛ expression could be the underlying cause for the observed reduction in MMP-3 levels. M27R cells were stably transfected with full-length mIKKɛ cDNA and increased IKKɛ expression was confirmed by immunoblotting (M27R/IKKɛ cells, Figure 3a). When MMP-3 expression in the mIKKɛ overexpressing cells was measured by qPCR, we found a sevenfold increase in mRNA expression levels relative to vector control cells (M27R/MOCK) (Figure 3b), confirming that IKKɛ in these cells was functional and acted as a transcriptional activator of MMP-3. This basal increase in MMP-3 expression, although it was not reflected in a measurable increase in MMP-3 production levels (Figure 4b) could be significantly augmented when M27R/IKKɛ cells were stimulated with PMA (30-fold increase in expression relative to PMA-stimulated M27R cells, Figure 4a) and this also translated into a measurable increase in MMP-3 production, as revealed by immunoblotting performed on tumor-cell-conditioned medium (Figure 4b). This effect of PMA was not observed in wild-type or control, vector-transfected M27R cells, suggesting that IKKɛ was essential for the stimulatory effect of PMA. IKKɛ expression also sensitized MMP-3 expression to induction by TNF-α. When treated with TNF-α, MMP-3 expression in M27R/IKKɛ, but not in M27R/MOCK cells, was increased twofold relative to basal levels (Figure 4c). Interestingly, M27R cells overexpressing IKKɛ did not have a significantly increased ability to colonize the lungs (Supplementary Figure S1). This suggests that in the absence of pre-activation of IKKɛ signaling by an inflammatory mediator, MMP-3 production in these cells may not have reached the levels required to significantly alter the course of lung metastasis.
Increased MMP-3 expression levels in M27R cells ectopically expressing IKKɛ. M27R cells were transfected with a plasmid vector expressing full length murine IKKɛ (M27R/IKKɛ) or an empty vector (M27R/MOCK). Shown in (a) is a representative result of two immunoblots performed using 200 μg of cell lysate per lane. Shown in (b) are MMP-3 expression levels expressed as the means (±s.e.m.) of five experiments normalized to GAPDH and expressed relative to non-transfected M27R cells that were assigned a value of 1. *P<0.05.
Ectopic IKKɛ expression sensitizes MMP-3 transcription to induction by PMA and TNF-α. Shown in (a) are MMP-3 expression levels measured by qPCR following a 4h stimulation of the cells with 100 nM PMA. Shown in (b) is a representative result of two immunoblots performed on 200 μg of conditioned media proteins that were obtained from cells stimulated (or not) for 24 h with 500 nM PMA and in (c) results of qPCR performed on tumor cells stimulated (or not) for 4 h with 10 nM TNF-α. Results in a and c are expressed as means (±s.e.m.) of three experiments, normalized to GAPDH and relative to non-transfected and non-stimulated M27R cells that were assigned a value of 1. *P<0.05, **P<0.01.
IKKɛ- dependent MMP-3 induction requires PKCα activity
To identify the signal transduction pathway(s) activated by PMA (a known inducer of PKCs) in our cells, we first analyzed the effect of PKC inhibitors on this activation. Cells were treated prior to PMA stimulation with Ro 31–8220—a broad-spectrum PKC inhibitor (Supplementary Figure S2A) and subsequently with the inhibitor Go6976 that more specifically targets the activities of PKCα, PKCβ and PKCμ (Figure 5a). These inhibitors blocked MMP-3 induction by PMA in M27R/IKKe cells, in a dose-dependent manner and the same effects were seen in wild-type M27 cells (Supplementary Figures S2B and C), indicating that similar regulatory mechanisms were likely at play in both cell types. Furthermore, the silencing of PKCα by short interfering RNA (siRNA) (Supplementary Figure S3) significantly reduced the ability of PMA to stimulate MMP-3 expression (Figure 5b) in M27R/IKKe cells, identifying PKCα as the major PKC involved in transcriptional activation of MMP-3 in these cells. Interestingly, we observed that the silencing of PKCα in M27 cells had no measurable effect on basal MMP-3 levels (Supplementary Figure S4), suggesting that the mediators involved in maintenance of basal MMP-3 expression levels and those regulating PMA-inducible MMP-3 transcription may be distinct.
MMP-3 induction by PMA requires PKC-α activity. M27R/IKKɛ cells were serum-starved overnight, treated (or not) with the indicated concentration of Go6976 for 30 min and stimulated with 100 nM PMA for 4 h in the presence of the inhibitor. Shown in (a) are results of qPCR expressed as the means (±s.e.m.) of three experiments, normalized to GAPDH and relative to non-stimulated and untreated cells that were assigned a value of 1. Shown in (b) are MMP-3 mRNA levels as measured by qPCR in cells that were transiently transfected for 48 h with 30 nM PKCα siRNA followed by a 4-h stimulation with 100 nM PMA. The results are expressed as the mean ratios (±s.e.m.) of MMP-3 mRNA levels relative to non-stimulated M27R/IKKɛ cells that were transiently transfected with a control, scrambled sequence and assigned a value of 1 (n=6). *P<0.05, ***P<0.005.
PMA-induced MMP-3 upregulation in M27R/IKKɛ cells involves both Akt and MEK signaling
Multiple signal transduction pathways can be activated downstream of PKCα. We used chemical inhibitors of MEK (PD98059) and PI3K (LY294002) to evaluate their role in signaling upstream of MMP-3. A dose-dependent inhibition of MMP-3 upregulation was observed with both inhibitors (Figures 6a and d), implicating both pathways in transcriptional activation of MMP-3. This was confirmed when the cells were stimulated with PMA and ERK (Figures 6b and c) and Akt (Figures 6e and f) phosphorylation levels were analyzed by immunoblotting, revealing an increase in p-ERK2 and p-Akt levels in M27R/IKKe cells relative to M27R cells.
ERK, Akt and NFκB signaling are involved in MMP-3 induction by PMA. M27R/IKKɛ cells were serum-starved overnight and treated (or not) with the indicated concentrations of PD98059 (a), LY294002 (d) or JSH-23 (g) for 3 h (a and d) or 90 min (g) prior to stimulation with 100 nM PMA for 4 h (a, d and g) or the indicated time intervals (b, c, e and f). Results of qPCR (a, d and g) are expressed as the means (±s.e.m.) of three experiments, normalized to GAPDH. Results of immunoblotting (b and e) are representative of three experiments and are expressed as mean fold increase (±s.e.m.) relative to non-stimulated cells that were assigned a value of 1. *P<0.05, **P<0.01.
The transcription factor p65 is also involved in PMA-induced MMP-3 expression
IKKɛ can activate several transcription factors including p65. When JSH-23—an inhibitor of the nuclear translocation of p65—was used to treat PMA-stimulated M27R/IKKɛ cells, MMP-3 induction was inhibited in a dose-dependent manner (Figure 6g). A similar effect was seen in (wt) M27 cells, where a reduction was also observed in the high basal MMP-3 levels following inhibitor treatment (Supplementary Figure S5). This indicated that p65 activation was a requirement for the basal expression as well as for PMA-mediated upregulation of MMP-3.
MMP-3 expression is required for lung colonization by M27 cells
To determine whether the loss of the lung-metastasizing potential in M27R cells was due to reduced MMP-3 expression levels, the cells were transduced with a retrovirus expressing full-length murine MMP-3 cDNA (M27R/MMP-3/RV cells) or a β-galactosidase cDNA (M27R/βgal), as control. Increased MMP-3 expression in the transduced cells was confirmed by immunoblotting and zymography (Figure 7a). When these cells were injected into mice via the tail vein, their ability to generate visible lung metastases was significantly increased relative to controls (Figures 7b and c), as also confirmed by histology (Figure 7d). This increase was site-specific, because the number of liver metastasis formed by these cells when injected via the intrasplenic/portal route was not significantly altered (Supplementary Figure S6), suggesting that MMP-3 facilitates metastasis, selectively in the lung. Increased lung metastasis was also observed with a clonal subpopulation of M27R cells that were transfected with a plasmid vector expressing MMP-3 cDNA (but not M27R cells transfected with an empty vector—M27R/CONT cells) and consequently produced increased MMP-3 levels, as confirmed by immunoblotting (Figures 7e–g). Conversely, M27 cells in which MMP-3 expression was silenced using shRNA had a significantly reduced ability to form lung metastases following intravenous injection of the cells, as compared with control cells transfected with a scrambled sequence (Figures 8a–c). Together, these results identify MMP-3 as essential for the growth of the tumor cells in the lung.
Increased MMP-3 expression restores the ability of M27R cells to colonize the lungs. Mice were injected intravenouly with 2 × 105 M27R cells that were transduced with retroviral particles (M27R/MMP-3/RV, a–d) or with a clonal subpopulation selected from mMMP-3 transfectants (M27R/MMP-3, e–g). Cells transduced with retroviral particles expressing β galactosidase (M27R/βgal, a–d) or a vector-transfected population (e–g), were used as controls, respectively. Shown in (a-top and e) are results of immunoblotting and in (a-bottom) of zymography performed on tumor-conditioned media. Shown in (c) and (g) are the lungs of tumor-injected mice removed 24 (c) or 29 (g) days following tumor injection and in (b) and (f) the number of visible metastases counted per lung (bar denotes median). Representative images obtained from hematoxylin and eosin-stained formalin-fixed, paraffin-embedded sections of the lungs are shown in (d) Mag. × 20 *P<0.05 **P<0.01.
MMP-3 is required for lung metastasis of M27 cells. Mice were injected via the tail vein with 2 × 105 M27 cells that were stably transfected with MMP-3 shRNA or a scrambled sequence as control. Lungs were removed 19 days later and fixed in Bouin’s solution prior to enumeration of lung metastases. Shown in (a) are the results of immunoblotting performed on media conditioned by the indicated cells. Shown in (b) are the numbers of visible metastases counted per lung in each group (bars denote medians) and in (c) the lungs obtained from each injection group. **P<0.01.
Discussion
Taken together, our results show that the loss of the lung-metastasizing potential in M27R cells was due, at least in part, to reduced MMP-3 expression levels and that this reduction, in turn, was the consequence of the downregulated expression of IKKɛ in these cells.
Gene expression profiles1, 2, 3,37 have consistently identified MMPs in gene sets associated with site-specific metastasis, indicating that distinct MMPs can contribute to tumor cell potential to colonize specific sites and implying that the unique extracellular matrix composition in different organ sites dictates the requirement for specific extracellular matrix degrading proteinases for tumor cell expansion. Our results suggest that MMP-3 plays a role in facilitating tumor growth preferentially in the lung. Huang et al.9 have shown that human breast carcinoma MBA-MB-231 cells had reduced spontaneous lung metastasis in mice with targeted reductions in MMP-3, MMP-10 and angiopoietin 2 expression levels in the lungs because of reduced vascular permeability and tumor extravasation. Several other correlative studies have also linked MMP-3 expression levels and lung cancer growth.6,7 The dependency on MMP-3 for expansion in the lung could be because of the ability of this proteinase to degrade several major components uniquely present in the lung extracellular matrix, including proteoglycans and to a lesser extent, elastin,38,39 or to an MMP-3-mediated vascular destabilization that renders the lung microenvironment more amenable to tumor infiltration, as suggested by Huang et al.9 MMP-3 may also enhance lung metastasis indirectly by activating other MMPs such as MMP-9 in a proteolytic cascade.40 While stroma-derived MMP-3 may play an important role in preparing the microenvironment during the premetastatic stages of spontaneous metastasis, as shown by Huang et al.9 for B16/F10 and MDA-MB-231 cells, MMP-3 produced by the tumor cells could further accelerate tumor expansion once dissemination to the lungs has occurred.
In a previous study, we have shown that the ectopic expression of the hIGF-IR in lung carcinoma M27 cells altered their MMP profile so that MMP-3, -9 and -13 expression levels were downregulated, whereas MMP-2 and -14 levels were upregulated, resulting in altered invasive/metastatic phenotypes of the cells.34, 35, 36 We have subsequently shown that the expression of MMP-9, but not of MMP-3, in M27R cells could be partially restored by ectopic expression of PKCα.34 Our present results identify IKKɛ as the additional mediator required for transcriptional activation of MMP-3 in these cells, and show that it mediated this effect by enhancing ERK, Akt and NFκB signaling.
In agreement with our results, Sweeney et al.28 also documented a downregulation of MMP-3 expression in IKKɛ−/− synoviocytes. In that study, cJUN, but not IκBα phosphorylation by IKKɛ was observed downstream of TNF-α stimulation,28 whereas in M27R/IKKɛ cells, we observed that transcriptional activation of MMP-3 by PMA was dependent on NFκB signaling. This suggests that the function of IKKɛ in MMP-3 regulation may be cell context- and also stimulus-dependent.
Peters et al.17 identified IKKɛ as part of a novel, PMA-inducible IκB kinase complex and have shown that a dominant-negative IKKɛ could inhibit PMA, but not TNF-α-induced NFκB activation. Their data also demonstrated that in the absence of PMA, IKKɛ could only phosphorylate IκBα on Ser36 and that following PMA stimulation, both Ser36 and Ser32 were phosphorylated, resulting in a fully activated kinase.17 However, in that study, the signal transduction pathway(s) leading to IKKɛ activation downstream of PMA were not identified.
Our results identify PKC-α as a mediator of NFκB activation downstream of PMA. This is consistent with other studies where PKCs have been implicated in NFκB activation,41, 42, 43 although the precise mechanism(s) have not been elucidated. In a study by Shinohara et al.,44 PKCβ was shown to mediate B-cell receptor-dependent NFκB activation through the formation of a protein complex that recruits and activates the IKK complex. Data from other studies also suggest that scaffolding proteins are assembled in a stimulus-specific manner to direct non-canonical IKK activity.45 This raises the possibility that in M27R/IKKɛ cells, PKC-α may be involved in mobilizing IKKɛ into a protein complex, where it can be activated and contribute to transcriptional regulation of MMP-3 (a proposed model is depicted in Figure 9).
A proposed model for the coordinated regulation of MMP-3 transcription by IKKɛ. A diagrammatic representation is shown based on our and other data for potential mechanisms of action of IKKɛ in transcriptional regulation of MMP-3. PMA-mediated activation of PKCα results in the formation of a protein complex that recruits IKKɛ to the plasma membrane where it can be further activated and directly phosphorylate Akt. PI3K activity is required for the recruitment of Akt to the plasma membrane and this may be provided by the presence of IGF-IR. Phospho-Akt can activate the canonical IKK pathway, resulting in nuclear translocation of the p65 transcription factor. The requirement for ERK pathway activation in MMP-3 induction by PMA may indicate that it (1) acts together with p65 to enhance signaling and/or (2) it is required for Akt-mediated activation of p65, as was also shown with the p38 MAPK.58
Our results implicate both Akt and ERK in IKKɛ-mediated MMP-3 upregulation in our cells. In other studies, IKKɛ was shown to directly activate Akt in a PI3K-dependent25 or independent27 manner. Our findings that ERK and Akt activation downstream of PMA were detectable in cells with low IKKɛ expression but increased further in the presence of increased IKKɛ level suggests that IKKɛ-dependent and independent (possibly IGF-IR mediated) activation of these pathways may have occurred in parallel and this was required for increased MMP-3 production.
The MMP-3 promoter has AP-1 and NFκB binding sites. We found that JSH-23, an inhibitor of p65 translocation, blocked PMA-induced MMP-3 synthesis in M27R/IKKɛ cells, implicating p65 in transcriptional activation of MMP-3 downstream of IKKɛ signaling. The activation of p65 downstream of PI3K/Akt46,47 and the Raf/MEK/ERK pathways48,49 has been reported by others. Interestingly, however, in our cells, ERK and Akt phosphorylation were not in themselves sufficient to trigger MMP-3 synthesis in response to PMA in the absence of IKKɛ. This suggests that p65 activation occurred downstream of IKKɛ, with ERK and Akt enhancing the p65-initiated signal.
Various physiological stimuli could mimic the effect of PMA in vivo, in the lung, during tumor growth. Included among them are inflammatory cytokines that can activate and act in concert with PKC to induce intracellular signaling and gene expression.50,51 Therefore, changes in the tumor microenvironment, including the accumulation of inflammatory cells such as neutrophils and macrophages52,53 could contribute to increased MMP-3 production in tumor cells that already express high IKKɛ levels, enhancing their invasion and local expansion in a selective manner.
Taken together, our data identify IKKɛ as a molecule involved in integrating and amplifying signals generated by different signal transduction pathways and show that this can result in important phenotype changes, such as an altered MMP profile. They reveal therefore a hitherto unappreciated role for IKKɛ as a potential regulator of tumor cell invasion and site-specific metastasis.
Materials and methods
Cells
M27 and M27R (previously M27IGFIR) cells are variant cell lines derived from the Lewis lung carcinoma that were generated in our laboratory. Their origin, culture conditions and metastatic phenotypes have been previously described.33,35 M27R/IKKɛ cells were generated by stably transfecting M27R cells with the full-length murine IKKɛ cDNA expressed in the pUNO plasmid (Invitrogen, Carlsbad, CA, USA). M27R/MOCK cells were transfected at the same time with the empty vector and used as a negative control in all the experiments. The transfected cells were selected with 100 μg/ml of blasticidin (InvivoGen, San Diego, CA, USA).
Antibodies and reagents
The mouse monoclonal anti MMP-3 antibody was from R&D Systems (Minneapolis, MN, USA), the rabbit polyclonal antibody to IKKɛ from Cell Signaling Technology (Danvers, MA, USA), the mouse monoclonal antibody to β-actin from Sigma Aldrich (St Louis, MO, USA), antibodies to Akt, p-Akt, ERK and p-ERK from Cell Signaling Technology and the polyclonal rabbit antibodies to USF2 and p65 from Santa Cruz Biotechnology (Santa Cruz, CA, USA). All restriction enzymes were obtained from New England Biolabs (Ipswich, MA, USA). PMA was from Sigma-Aldrich Canada (Oakville, ON, Canada). The inhibitors Ro31–8220, Go6976 and JSH-23 were from Calbiochem (Gibbstown, NJ, USA) and PD98059 and LY294002 were from Cell Signaling Technology.
Plasmids and transfection
Full-length murine MMP-3 cDNA was extracted from pCMV6 (Origene, Rockville, MD, USA) and cloned into the XbaI and EcoRV sites of pcDNA3.1 (Invitrogen Life Technologies, Eugene, OR, USA). To generate retroviral particles expressing MMP-3, a MMP-3 cDNA fragment was extracted from the pCMV6 plasmid using Phusion high fidelity polymerase (New England Biolabs) and the primer set described in Supplementary Table 1. The fragment was digested with BamHI and EcoRI, cloned into the pQXiPuro vector and virus particles were produced using the LnxE packaging cell line (as described by Geiling et al.54).
All transfections were performed using Lipofectamine 2000 (Invitrogen). M27R cells stably transfected with pcDNA3.1 expressing full-length murine MMP-3 were selected using 200 μg/ml hygromycin that was added 48 h after transfection and the transfectants cloned by the limiting dilution and screened by qPCR to select clones with high MMP-3 expression levels. MMP-3 expression and activity levels were confirmed by western blotting and zymography, respectively (see below).
To generate a population of cells stably expressing MMP-3, we used retroviral particles produced in the LnxE cells. The cells were grown to 80% confluency and transfected with the pQxiPuro vector expressing full-length mouse MMP-3 or β galactosidase cDNA. Supernatants containing virus particles were collected 48 and 62 h later, filtered and added to M27R cells. The transduced cells were selected by the addition of 2 μg/ml puromycin, 48 h post infection.
To silence MMP-3 expression, M27 cells were transfected with MMP-3 shRNA (Origene, Rockville, MD, USA). A scrambled shRNA sequences was used as control. Transfectants were selected using 2 μg/ml puromycin and the drug-resistant cells cloned and screened by RT–PCR to identify clones with reduced MMP-3 expression. MMP-3 silencing was confirmed by immunoblotting performed on conditioned media.
Polymerase chain reaction
RNA was extracted using Trizol (Invitrogen) and cDNA synthesized as we previously described.55 Semiquantitative RT–PCR was performed using a standard procedure, as we previously described.34 qPCR was performed using the MyiQ2 Real-time PCR Detection system (BioRad, Hercules, CA, USA). The cDNAs were diluted 1:10 (MMP-3 and PKC-α) or 1:100 (GAPDH) and 2 μl added to 23 μl of the qPCR mix containing the BioRad iQ SYBR green supermix (BioRad) and the primers (Supplementary Table S1) at a concentration of 320 nM. Samples were denatured for 3 min at 95 °C, amplified for 40 cycles (denaturation at 95 °C for 10 s followed by annealing at 57 °C (GAPDH), 59 °C (PKC-α) or 60 °C (IKKɛ and MMP-3) for 30 s) followed by a final extension step for 1 min at 95 °C. The normalized expression levels (ddCt) were calculated using the BioRad iQ5 software with the modified equation initially introduced by Livak et al.56 Each experiment was performed in triplicates.
Short interfering RNA
PKC-α siRNA (s71688) and a scrambled control (negative control #1 siRNA, cat # 4390843) were obtained from Ambion (Foster City, CA, USA) and used at the indicated concentrations to transfect tumor cells that were plated in 6-well plates at a density of 2 × 105 cells/well, 24 h earlier. RNA was extracted 48 h later and PKC-α expression levels were analyzed by qPCR.
Immunoblotting
Cells were lysed as we described in detail elsewhere57 or tumor-conditioned media were collected and concentrated 100-fold using centrifugal filters (Millipore, County Cork, Ireland). Proteins were separated by polyacrylamide gel electrophoresis on 10% SDS gels, transferred onto a nitrocellulose membrane and the blots incubated overnight with the primary antibodies diluted 1:1000 followed by a 2-h incubation with the secondary antibodies diluted 1:10000. The gels were imaged and densitometry performed on the bands using an Alpha Imager gel documentation system (Alpha Innotech, San Leandro, CA, USA) or an LAS4000 imagequant system (GE Healthcare, Baie d’Urfe, QC, Canada).
Zymography
Concentrated (100 × ) conditioned media proteins were separated by SDS polyacrylamide gel electrophoresis using 10% polyacrylamide gels containing also 0.1% β casein. The gels were washed twice for 30 min in a 50 mM Tris HCl buffer containing 0.2 M NaCl, 5 mM CaCl2, 0.02% NaN3 and 2.5% Triton X-100, pH 7.5 and then overnight at 37 °C, with shaking, in the same buffer but without Triton X-100. Gels were stained with 0.5% Coomasie brilliant blue R-250 for 1 h and destained with a solution of 40% methanol and 10% acetic until clearings indicating β casein proteolysis were visible. The gels were imaged using the Alpha Imager gel documentation system.
Cell stimulation and inhibitor treatment
Cells were serum-starved for 18 h prior to PMA or TNF-α (Invitrogen) stimulation. Stimulation was with 100 nM PMA for 5 h prior to RNA extraction and with 500 nM PMA for 18 h prior to protein analysis. TNF-α was added at a concentration of 10 nM and the cells incubated for 4 h prior to RNA extraction. Where indicated, the cells were treated with the specified concentrations of the chemical inhibitors for 30 (Ro31–8220 and Go6976), 90 (JSH-23) or 180 (LY294002 and PD98059) min prior to PMA stimulation.
Experimental lung metastasis assay
All mouse experiments were carried out in strict accordance with the recommendations as outlined in the Canadian Council on Animal Care (CCAC) ‘Guide to the Care and Use of Experimental Animals’ and under the conditions and procedures approved by the Animal Care Committee of McGill University (AUP number: 5260). To generate experimental lung metastases, female C57BL/6 mice (8–12-week old) obtained from Charles River Laboratories (St Constant, QC, Canada) were injected via the tail vein with 2 × 105 cells in RPMI and euthanized 19 days later. Lungs were fixed in Bouin’s fixative and lung metastases visible on the surface of the lungs were enumerated. Paraffin sections of formalin-fixed lung fragments were hematoxylin and eosin-stained and used to compare tumor loads.
Experimental liver metastasis assay
Experimental liver metastases were generated by intrasplenic/portal injections of 2 × 105 tumor cells, followed by splenectomy, as previously described.55 Animals were sacrificed 19 days later and visible metastases on the surface of the liver were enumerated without prior fixation.
Statistical analyses
All data obtained from in vitro experiments were analyzed using the Student t-test. The non-parametric Mann–Whitney test was used to analyze metastasis data.
Acknowledgements
This work was supported by grant MOP-80201 from the Canadian Institute for Health Research (to PB) by a McGill Integrated Cancer Research Training Program fellowship and a FRSQ fellowship (both to ES) and by a MITACS internship (to MP).
References
Minn AJ, Gupta GP, Siegel PM, Bos PD, Shu WP, Giri DD et al. Genes that mediate breast cancer metastasis to lung. Nature 2005; 436: 518–524.
Bos PD, Zhang XHF, Nadal C, Shu WP, Gomis RR, Nguyen DX et al. Genes that mediate breast cancer metastasis to the brain. Nature 2009; 459: 1005–U137.
Kang YB, Siegel PM, Shu WP, Drobnjak M, Kakonen SM, Cordon-Cardo C et al. A multigenic program mediating breast cancer metastasis to bone. Cancer Cell 2003; 3: 537–549.
Hanahan D, Weinberg RA . Hallmarks of cancer: the next generation. Cell 2011; 144: 646–674.
Kessenbrock K, Plaks V, Werb Z . Matrix metalloproteinases: regulators of the tumor microenvironment. Cell 2010; 141: 52–67.
Thomas P, Khokha R, Shepherd FA, Feld R, Tsao MS . Differential expression of matrix metalloproteinases and their inhibitors in non-small cell lung cancer. J Pathol 2000; 190: 150–156.
Michael M, Babic B, Khokha R, Tsao M, Ho J, Pintilie M et al. Expression and prognostic significance of metalloproteinases and their tissue inhibitors in patients with small-cell lung cancer. J Clin Oncol 1999; 17: 1802–1808.
Beom JL, Sung SJ, Song YC, Choong SL . Expression of metastasis-associated molecules in non-small cell lung cancer and their prognostic significance. Mol Med Rep 2010; 3: 43–49.
Huang YJ, Song N, Ding YP, Yuan SP, Li XH, Cai HC et al. Pulmonary vascular destabilization in the premetastatic phase facilitates lung metastasis. Cancer Res 2009; 69: 7529–7537.
Constantin A, Lauwers-Cancès V, Navaux F, Abbal M, Van Meerwijk J, Mazières B et al. Stromelysin 1 (matrix metalloproteinase 3) and HLA-DRB1 gene polymorphisms: Association with severity and progression of rheumatoid arthritis in a prospective study. Arthritis and Rheum 2002; 46: 1754–1762.
Sharrocks AD, Brown AL, Ling Y, Yates PR . The ETS-domain transcription factor family. Int J Biochem Cell Biol 1997; 29: 1371–1387.
Carrère S, Verger A, Flourens A, Stehelin D, Duterque-Coquillaud M . Erg proteins, transcription factors of the Ets family, form homo, heterodimers and ternary complexes via two distinct domains. Oncogene 1998; 16: 3261–3268.
Moreno R, Sobotzik J-M, Schultz C, Schmitz ML . Specification of the NF-kappa B transcriptional response by p65 phosphorylation and TNF-induced nuclear translocation of IKK epsilon. Nucleic Acids Res 2010; 38: 6029–6044.
Bond M, Chase AJ, Baker AH, Newby AC . Inhibition of transcription factor NF-κB reduces matrix metalloproteinase-1, -3 and -9 production by vascular smooth muscle cells. Cardiovasc Res 2001; 50: 556–565.
Borghaei RC, Rawlings PL Jr, Javadi M, Woloshin J . NF-κB binds to a polymorphic repressor element in the MMP-3 promoter. Biochem Biophys Res Commun 2004; 316: 182–188.
Borghaei RC, Gorski G, Javadi M, Chambers M . NF-κB AND ZBP-89 regulate MMP-3 expression via a polymorphic site in the promoter. Biochem Biophys Res Commun 2009; 382: 4.
Peters RT, Liao S-M, Maniatis T . IKKμ Is Part of a Novel PMA-Inducible IºB Kinase Complex. Mol Cell 2000; 5: 513–522.
Shimada T, Kawai T, Takeda K, Matsumoto M, Inoue J-i, Tatsumi Y et al. IKK-i, a novel lipopolysaccharide-inducible kinase that is related to IκB kinases. Int Immunol 1999; 11: 1357–1362.
Brockman JA, Scherer DC, McKinsey TA, Hall SM, Qi X, Lee WY et al. Coupling of a signal response domain in I kappa B alpha to multiple pathways for NF-kappa B activation. Mol Cell Biol 1995; 15: 2809–2818.
Brown K, Gerstberger S, Carlson L, Franzoso G, Siebenlist U . Control of I-kappa-B-alpha proteolysis by site specific, signal-induced phosphorylation. Science 1995; 267: 1485–1488.
Traenckner EBM, Pahl HL, Henkel T, Schmidt KN, Wilk S, Baeuerle PA . Phosphorylation of human I-kappa-B-alpha on serine 32 and serine 36 controls I-kappa-B-alpha proteolysis and NF-kappa-B activation in response to diverse stimuli. EMBO J 1995; 14: 2876–2883.
DiDonato J, Mercurio F, Rosette C, WuLi J, Suyang H, Ghosh S et al. Mapping of the inducible I kappa B phosphorylation sites that signal its ubiquitination and degradation. Mol Cell Biol 1996; 16: 1295–1304.
Harris J, Oliere S, Sharma S, Sun Q, Lin R, Hiscott J et al. Nuclear accumulation of cRel following C-terminal phosphorylation by TBK1/IKK epsilon. J Immunol 2006; 177: 2527–2535.
Sharma S, tenOever BR, Grandvaux N, Zhou G-P, Lin R, Hiscott J . Triggering the interferon antiviral response through an IKK-related pathway. Science 2003; 300: 1148–1151.
Xie X, Zhang D, Zhao B, Lu M-K, You M, Condorelli G et al. IκB kinase ɛ and TANK-binding kinase 1 activate AKT by direct phosphorylation. Proc Natl Acad Sci 2011; 108: 6474–6479.
Ou Y-H, Torres M, Ram R, Formstecher E, Roland C, Cheng T et al. TBK1 directly engages Akt/PKB survival signaling to support oncogenic transformation. Mol Cell 2011; 41: 458–470.
Guo JP, Coppola D, Cheng JQ . IKBKE protein activates akt independent of phosphatidylinositol 3-kinase/PDK1/mTORC2 and the pleckstrin homology domain to sustain malignant transformation. J Biol Chem 2011; 286: 37389–37398.
Sweeney SE, Hammaker D, Boyle DL, Firestein GS . Regulation of c-Jun phosphorylation by the IκB kinase-ɛ complex in fibroblast-like synoviocytes. J Immunol 2005; 174: 6424–6430.
Boehm JS, Zhao JJ, Yao J, Kim SY, Firestein R, Dunn IF et al. Integrative genomic approaches identify IKBKE as a breast cancer oncogene. Cell 2007; 129: 1065–1079.
Hutti JE, Shen RR, Abbott DW, Zhou AY, Sprott KM, Asara JM et al. Phosphorylation of the tumor suppressor CYLD by the breast cancer oncogene IKKɛ promotes cell transformation. Mol Cell 2009; 34: 461–472.
Samani AA, Yakar S, LeRoith D, Brodt P . The role of the IGF system in cancer growth and metastasis: Overview and recent insights. Endocr Rev 2007; 28: 20–47.
Seccareccia E, Brodt P . The role of the insulin-like growth factor-I receptor in malignancy: an update. Growth Hor IGF Res 2012; 22: 193–199.
Brodt P, Fallavollita L, Khatib A-M, Samani AA, Zhang D . Cooperative regulation of the invasive and metastatic phenotypes by different domains of the type I insulin-like growth factor receptor β subunit. J Biol Chem 2001; 276: 33608–33615.
Li S, Zhang DL, Yang L, Burnier JV, Wang N, Lin RT et al. The IGF-I receptor can alter the matrix metalloproteinase repertoire of tumor cells through transcriptional regulation of PKC-alpha. Mol Endocrinol 2009; 23: 2013–2025.
Brodt P . Characterization of two highly metastatic variants of Lewis lung carcinoma with different organ specificities. Cancer Res 1986; 46: 2442–2448.
Long L, Rubin R, Brodt P . Enhanced invasion and liver colonization by lung carcinoma cells overexpressing the type 1 insulin-like growth factor receptor. Exp Cell Res 1998; 238: 116–121.
Landemaine T, Jackson A, Bellahcene A, Rucci N, Sin S, Martin Abad B et al. A six-gene signature predicting breast cancer lung metastasis. Cancer Res 2008; 68: 6092–6099.
Murphy G, Cockett MI, Ward RV, Docherty AJ . Matrix metalloproteinase degradation of elastin, type IV collagen and proteoglycan. A quantitative comparison of the activities of 95 kDa and 72 kDa gelatinases, stromelysins-1 and -2 and punctuated metalloproteinase (PUMP). Biochemical J 1991; 277: 277–279.
Park JB, Kong CG, Suhl KH, Chang ED, Riew KD . The increased expression of matrix metalloproteinases associated with elastin degradation and fibrosis of the ligamentum flavum in patients with lumbar spinal stenosis. Clin Orthop Surg 2009; 1: 81–89.
Vandooren J, Van den Steen PE, Opdenakker G . Biochemistry and molecular biology of gelatinase B or matrix metalloproteinase-9 (MMP-9): the next decade. Crit Rev Biochem Mol Biol 2013; 48: 222–272.
Holden NS, Squires PE, Kaur M, Bland R, Jones CE, Newton R . Phorbol ester-stimulated NF-kappa B-dependent transcription: Roles for isoforms of novel protein kinase C. Cell Signal 2008; 20: 1338–1348.
Krappmann D, Patke A, Heissmeyer V, Scheidereit C . B-cell receptor- and phorbol ester-induced NF-kappa B and c-Jun N-terminal kinase activation in B cells requires novel protein kinase C's. Mol Cel Biol 2001; 21: 6640–6650.
Zhang J, Ping PP, Vondriska TM, Tang XL, Wang GW, Cardwell EM et al. Cardioprotection involves activation of NF-kappa B via PKC-dependent tyrosine and serine phosphorylation of I kappa B-alpha. Am J Physiol Heart Circ Physiol 2003; 285: H1753–H1758.
Shinohara H, Yasuda T, Aiba Y, Sanjo H, Hamadate M, Watarai H et al. PKC beta regulates BCR-mediated IKK activation by facilitating the interaction between TAK1 and CARMA1. J Exp Med 2005; 202: 1423–1431.
Chau T-L, Gioia R, Gatot J-S, Patrascu F, Carpentier I, Chapelle J-P et al. Are the IKKs and IKK-related kinases TBK1 and IKK-epsilon similarly activated? Trends Biochem Sci 2008; 33: 171–180.
Lu YB, Wahl LM . Production of matrix metalloproteinase-9 by activated human monocytes involves a phosphatidylinositol-3 kinase/Akt/IKK alpha/NF-kappa B pathway. J Leukoc Biol 2005; 78: 259–265.
Ozes ON, Mayo LD, Gustin JA, Pfeffer SR, Pfeffer LM, Donner DB . NF-kappa B activation by tumour necrosis factor requires the Akt serine-threonine kinase. Nature 1999; 401: 82–85.
Wang XF, Wang QD, Hu WQ, Evers BM . Regulation of phorbol ester-mediated TRAF1 induction in human colon cancer cells through a PKC/RAF/ERK/NF-kappa B-dependent pathway. Oncogene 2004; 23: 1885–1895.
Hwang YP, Yun HJ, Kim HG, Han EH, Lee GW, Jeong HG . Suppression of PMA-induced tumor cell invasion by dihydroartemisinin via inhibition of PKC alpha/Raf/MAPKs and NF-kappa B/AP-1-dependent mechanisms. Biochem Pharmacol 2010; 79: 1714–1726.
Kim H, Zamel R, Bai XH, Liu M . PKC activation induces inflammatory response and cell death in human bronchial epithelial cells. PLoS ONE 2013; 8: e64182.
Leppanen T, Tuominen RK, Moilanen E . Protein kinase C and its inhibitors in the regulation of inflammation: inducible nitric oxide synthase as an example. Basic Clin Pharmacol Toxicol 2014; 114: 37–43.
Heinrich EL, Walser TC, Krysan K, Liclican EL, Grant JL, Rodriguez NL et al. The inflammatory tumor microenvironment, epithelial mesenchymal transition and lung carcinogenesis. Cancer Microenviron 2012; 5: 5–18.
Qian BZ, Li J, Zhang H, Kitamura T, Zhang J, Campion LR et al. CCL2 recruits inflammatory monocytes to facilitate breast-tumour metastasis. Nature 2011; 475: 222–225.
Geiling B, Vandal G, Posner AR, de Bruyns A, Dutchak KL, Garnett S et al. A modular lentiviral and retroviral construction system to rapidly generate vectors for gene expression and gene knockdown in vitro and in vivo. PLoS ONE 2013; 8: 10.
Burnier JV, Wang N, Michel RP, Hassanain M, Li S, Lu Y et al. Type IV collagen-initiated signals provide survival and growth cues required for liver metastasis. Oncogene 2011; 30: 3766–3783.
Livak KJ, Schmittgen TD . Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method. Methods 2001; 25: 402–408.
Zhang DL, Bar-Eli M, Meloche S, Brodt P . Dual regulation of MMP-2 expression by the type 1 insulin-like growth factor receptor—The phosphatidylinositol 3-kinase/Akt and Raf/ERK pathways transmit opposing signals. J Biol Chem 2004; 279: 19683–19690.
Madrid LV, Mayo MW, Reuther JY, Baldwin AS . Akt stimulates the transactivation potential of the RelA/p65 subunit of NF-κB through utilization of the IκB kinase and activation of the mitogen-activated protein kinase p38. J Biol Chem 2001; 276: 18934–18940.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Oncogenesis website
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Seccareccia, E., Pinard, M., Wang, N. et al. The inhibitor of kappa B kinase-epsilon regulates MMP-3 expression levels and can promote lung metastasis. Oncogenesis 3, e116 (2014). https://doi.org/10.1038/oncsis.2014.28
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/oncsis.2014.28
This article is cited by
-
Glucosamine sulfate suppresses the expression of matrix metalloproteinase-3 in osteosarcoma cells in vitro
BMC Complementary and Alternative Medicine (2016)