Abstract
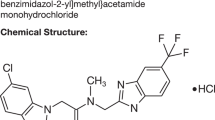
The neurosteroid pregnenolone and its sulfated derivative enhance learning and memory in rodents. Pregnenolone sulfate also positively modulates NMDA receptors and could thus ameliorate hypothesized NMDA receptor hypofunction in schizophrenia. Furthermore, clozapine increases pregnenolone in rodent hippocampus, possibly contributing to its superior efficacy. We therefore investigated adjunctive pregnenolone for cognitive and negative symptoms in patients with schizophrenia or schizoaffective disorder receiving stable doses of second-generation antipsychotics in a pilot randomized, placebo-controlled, double-blind trial. Following a 2-week single-blind placebo lead-in, patients were randomized to pregnenolone (fixed escalating doses to 500 mg/day) or placebo, for 8 weeks. Primary end points were changes in BACS and MCCB composite and total SANS scores. Of 21 patients randomized, 18 completed at least 4 weeks of treatment (n=9/group). Pregnenolone was well tolerated. Patients receiving pregnenolone demonstrated significantly greater improvements in SANS scores (mean change=10.38) compared with patients receiving placebo (mean change=2.33), p=0.048. Mean composite changes in BACS and MCCB scores were not significantly different in patients randomized to pregnenolone compared with placebo. However, serum pregnenolone increases predicted BACS composite scores at 8 weeks in the pregnenolone group (rs=0.81, p=0.022). Increases in allopregnanolone, a GABAergic pregnenolone metabolite, also predicted BACS composite scores (rs=0.74, p=0.046). In addition, baseline pregnenolone (rs=−0.76, p=0.037), pregnenolone sulfate (rs=−0.83, p=0.015), and allopregnanolone levels (rs=−0.83, p=0.015) were inversely correlated with improvements in MCCB composite scores, further supporting a possible role for neurosteroids in cognition. Mean BACS and MCCB composite scores were correlated (rs=0.74, p<0.0001). Pregnenolone may be a promising therapeutic agent for negative symptoms and merits further investigation for cognitive symptoms in schizophrenia.
Similar content being viewed by others
INTRODUCTION
Cognitive and negative symptoms in schizophrenia are frequently severe and strongly correlated with decreased functional outcome and quality of life (Buchanan, 2006; Buchanan et al, 2005; Green, 2006; Green et al, 2000; Harvey et al, 2004; Kirkpatrick et al, 2006; Marder, 2006; Marder and Fenton, 2004), but effective pharmacological interventions remain limited for these symptom domains (Buchanan, 2007; Buchanan et al, 2005, 2007; Carter et al, 2008; Kirkpatrick et al, 2006). Although first- and second-generation antipsychotic agents have been reported to produce improvements in cognitive and negative symptoms, the emerging scientific consensus appears to be that these effects are generally modest in scope, and that significant disabling symptoms frequently persist despite positive symptom reduction (Buchanan et al, 2005; Keefe et al, 2007; Kirkpatrick et al, 2006). New treatment strategies are therefore necessary to address these important dimensions of schizophrenia symptomatology.
The neurosteroid pregnenolone may represent a promising and mechanistically novel agent for cognitive and negative symptoms in schizophrenia. Pregnenolone (Flood et al, 1992) and its sulfated derivative, pregnenolone sulfate (Akwa et al, 2001; Darnaudery et al, 2002; Flood et al, 1995; Ladurelle et al, 2000; Mayo et al, 1993; Meziane et al, 1996; Pallares et al, 1998; Vallee et al, 1997, 2001), enhance learning and memory in animal models at concentrations that are physiologically relevant and known to be present in human brain (Marx et al, 2006c; Weill-Engerer et al, 2002). For example, acute administration of pregnenolone or pregnenolone sulfate to rodents, delivered either i.c.v., i.p., or by direct hippocampal injection, results in behavioral performance increases in the T-maze, the Morris water maze, and the Y-maze (Akwa et al, 2001; Flood et al, 1992, 1995; Vallee et al, 1997). Pregnenolone sulfate positively modulates glutamatergic N-methyl-D-aspartate (NMDA) receptors (Bowlby, 1993; Irwin et al, 1994; Wu et al, 1991), enhances long-term potentiation in rat hippocampus (Sliwinski et al, 2004), and prevents learning and memory deficits induced by NMDA receptor antagonists, including MK-801 and DAP-V (Akwa et al, 2001; Cheney et al, 1995; Mathis et al, 1994, 1996; Romeo et al, 1994). Treatment with pregnenolone, which is metabolized to pregnenolone sulfate in humans following acute administration (Morley et al, 1997; Roberts, 1995), may thus represent a logical strategy for the amelioration of hypothesized NMDA receptor hypofunction in schizophrenia (Coyle, 2006; Javitt, 2004, 2007; Millan, 2005; Rujescu et al, 2006). Pregnenolone sulfate also increases acetylcholine release in multiple rodent brain regions (Darnaudery et al, 1998, 2002; Mayo et al, 1993; Pallares et al, 1998; Vallee et al, 1997) and prevents the memory-impairing effects of the muscarinic cholinergic receptor antagonist scopolamine (Meziane et al, 1996; Vallee et al, 2001), actions consistent with cognitive enhancement. In addition, clozapine markedly increases pregnenolone levels in rodent hippocampus, representing a candidate mechanism for its superior efficacy (Marx et al, 2006a). Converging evidence thus suggests that pregnenolone may have potential utility for the treatment of cognitive and negative symptoms in schizophrenia.
Despite the availability of pregnenolone as a dietary supplement in the United States, very few clinical trials have investigated its use. Studies conducted in the 1940s and 1950s showed that pregnenolone 25–500 mg/day was safe and well tolerated in humans (Davison et al, 1950; Freeman et al, 1950a; Guest et al, 1950; Henderson et al, 1950; McGavack et al, 1951; Pincus and Hoagland, 1944, 1945a, 1945b). A number of these earlier studies treated patients with inflammatory diseases, such as rheumatoid arthritis, and several reported improvements in symptoms and overall functioning following pregnenolone. According to these earlier reports, pregnenolone was very well tolerated with minimal side effects, and did not affect weight, heart rate, blood pressure (even in patients with hypertension), menstrual cycle, or glucose levels (either in diabetics or non-diabetics). In a more recent investigation, pregnenolone at low doses (15–30 mg/day) was generally well tolerated in healthy volunteers with no significant side effects compared with placebo (Meieran et al, 2004). Evidence to date thus suggests that pregnenolone has a favorable safety profile, although controlled trials remain very limited.
In this pilot study, we thus investigated pregnenolone as an adjunctive therapeutic strategy for cognitive and negative symptoms in patients with schizophrenia or schizoaffective disorder with an escalating fixed-dose approach, achieving a total dose of 500 mg/day (approaching the highest well tolerated dose reported in the existing literature) in the last 4 weeks of the study administered in divided doses (Freeman et al, 1950b; McGavack et al, 1951). Although human pharmacokinetic studies addressing acute administration are extremely few, a single oral dose of pregnenolone 175 mg approximately doubles serum levels over the course of 4–8 h (Roberts, 1995). As pregnenolone levels decrease by approximately 60% with age (Morley et al, 1997; Roberts, 1995), and as we estimated that the mean study participant age would be greater than 40, we predicted that our dosing strategy of 500 mg/day of pregnenolone in the last 4 weeks of the study would likely produce pregnenolone levels that are close to those observed in young adulthood or up to twofold higher than typical young adult levels.
METHODS
This pilot investigation was a placebo-controlled, double-blind, parallel group, randomized trial of adjunctive pregnenolone for the treatment of cognitive and negative symptoms in patients with schizophrenia or schizoaffective disorder. Following a single-blind 2-week placebo lead-in phase (all patients), subjects were randomized to 8 weeks of treatment with adjunctive pregnenolone or placebo. Patients received a total of six study visits, which took place every 2 weeks. In addition, subjects received staggered telephone check-in calls to assess potential side effects every 2 weeks (ie, during alternate weeks when a study visit did not take place). The trial was conducted at a single site, the Durham Veterans Affairs Medical Center in Durham, North Carolina. The protocol was approved by the local institutional review board and conducted under FDA Investigational New Drug (IND) no. 71 768. The ClinicalTrials.gov number for this study was NCT00560937.
Subjects
Subjects were outpatients between the ages of 18 and 65 years with schizophrenia or schizoaffective disorder diagnosed by DSM-IV/DSM-IV-TR criteria using the Structured Clinical Interview (First et al, 1996) and medical records. All subjects were between the ages of 18 and 65 years and provided informed consent. Duration of illness was more than 1 year for all enrolled patients. To be eligible for the trial, patients had to be taking a second-generation antipsychotic (aripiprazole, olanzapine, quetiapine, or risperidone) for at least 8 weeks, with no changes in antipsychotic dosing in the preceding 4 weeks. Patients receiving first-generation antipsychotics were excluded from this pilot investigation. Concomitant psychiatric medications were permissible (antidepressants, mood stabilizers, anticholinergics, and other), provided that patients were receiving stable doses of all of these medications in the 4 weeks preceding the trial and throughout the entire duration of the study. Any change in psychiatric medications at any point during the study rendered a patient ineligible to continue participation. Exclusionary were unstable medical or neurological illness, alcohol or other substance dependence within the last month (other than nicotine), use of oral contraceptives or other hormonal supplementation such as estrogen (although early studies suggested no effects on menstrual cycle, alterations in downstream pregnenolone metabolites, such as estradiol, could theoretically impact the efficacy of oral contraceptives or estrogen replacement), active expression of suicidal or homicidal ideation, pregnancy or breast-feeding, and known allergy to study medication.
During the screening visit (Visit 1), patients received a physical exam, vital signs, and electrocardiogram (EKG), as well as baseline laboratory measures consisting of serum electrolytes, glucose, creatinine, blood urea nitrogen (chemistry 7 panel), liver function tests, complete blood count (CBC), urinalysis, urine toxicology test, thyroid stimulating hormone (TSH), and prolactin, and serum pregnancy test if female. These tests were also repeated at the completion of the study (Visit 6). In addition, patients received an interim EKG 4 weeks post-randomization, as well as a serum pregnancy test if female (Visit 4). Patients also received a chemistry 7 panel, CBC, and liver function tests at Visits 2, 3, 4, and 5 (ie, at all study visits). Psychiatric symptoms were assessed at baseline using the Scale for the Assessment of Negative Symptoms (Andreasen, 1983), the Positive and Negative Symptom Scale (PANSS) (Kay et al, 1987), the Calgary Depression Rating Scale (CDRS) (Addington et al, 1990), the Clinical Global Impression Improvement (CGI-I) and Severity (CGI-S) scales, the Barnes Akathisia Scale (BAS) (Barnes, 1989), the Simpson Angus Scale for Extrapyramidal Symptoms (SAS) (Simpson and Angus, 1970), the Quality of Life Scale (QOL) (Heinrichs et al, 1984), and the Hillside Adverse Events Form. Each side effect query was rated with the latter assessment instrument on a Likert scale with regard to both intensity and relationship to study drug. In addition, potential side effects were also assessed with this instrument during a scheduled phone check-in call every 2 weeks, which was staggered to study visits. Side effects were thus assessed at weekly intervals (either in person at a scheduled study visit or by phone check-in) using a structured rating scale. One research nurse with 5 years of experience in the conduction of schizophrenia clinical trials completed both psychiatric and cognitive assessments throughout the study, and was trained to one point of divergence on each PANSS item.
Cognitive symptoms were assessed by the Brief Assessment of Cognition in Schizophrenia (BACS) (Keefe et al, 2004, 2008) and the MATRICS Consensus Cognitive Battery (MCCB), (Nuechterlein and Green, 2006; Nuechterlein et al, 2008). To the best of our knowledge, no clinical trial to date has reported both of these cognitive assessments within the same study. The MCCB became available shortly before enrollment for this study. Given the advancement that the MCCB assessment tool represents in incorporating the latest expert opinion in this area, inclusion of the MCCB battery was judged imperative for this pilot investigation and provided an opportunity to obtain initial data with both cognitive instruments. The BACS and MCCB batteries were administered 2 weeks following the screening visit (following the completion of the 2-week placebo lead-in phase at Visit 2), and at two 4-week intervals thereafter (at mid point following randomization at Visit 4 and at the final visit (Visit 6). The BACS cognitive battery uses the following assessments in the respective targeted domains (Keefe et al, 2004, 2008): list learning (verbal memory), digit sequencing task (working memory), token motor task (motor speed), verbal fluency (processing speed), symbol coding (attention and processing speed), and the Tower of London test (executive functions/reasoning and problem solving). The MCCB uses the following assessments: Trail Making Test, Part A and the symbol coding subtest of the BACS (both assess speed of processing), the Hopkins Verbal Learning Test-Revised, immediate recall (three learning trials only) (verbal learning), the Wechsler Memory Scale, 3rd ed., spatial span subtest (working memory, nonverbal), the Letter-Number Span test (working memory, verbal), the Neuropsychological Assessment Battery, mazes subtest (reasoning and problem solving), the Brief Visuospatial Memory Test-Revised (visual learning), the Category Fluency Test (animal naming) (speed of processing), the Mayer-Salovey-Caruso Emotional Intelligence Test, managing emotions branch (social cognition), and the Continuous Performance Test, Identical Pairs version (attention/vigilance). Of note, the symbol coding subtest of the BACS was administered only once per visit at Visits 2, 4, and 6, although it is a component of both the BACS and MCCB cognitive batteries, to avoid potentially confounding practice effects.
Study drug (pregnenolone 50 mg (PREG)) and matching placebo identical in appearance was obtained from Douglas Laboratories (Pittsburgh, PA, USA), which provided certificates of analysis for pregnenolone 50 mg tablets and matching placebo. Study drug was dispensed every 2 weeks at each study visit at fixed escalating doses as follows:
Visit 1: Two-week single-blind placebo lead-in phase, one placebo tablet twice each day (all pts),
Visit 2: Randomization to PREG 50 mg twice each day (100 mg/day total) or placebo for 2 weeks,
Visit 3: PREG 150 mg twice each day (300 mg/day total) or placebo for 2 weeks,
Visit 4: PREG 250 mg twice each day (500 mg/day total) or placebo for 2 weeks,
Visit 5: PREG 250 mg twice each day (500 mg/day total) or placebo continued for 2 weeks.
Patients thus received PREG 500 mg/day in divided doses during the last 4 weeks of the study. Patients also received the Hillside Adverse Events Form at Visits 2–6, and during staggered telephone check-in calls every 2 weeks, beginning 1 week into the single-blind placebo lead-in phase.
Neurosteroid Analyses
Pregnenolone and allopregnanolone levels in serum were determined by a highly sensitive and specific gas chromatography/mass spectrometry (GC/MS) method in the negative ion chemical ionization mode, as described earlier (Marx et al, 2006d, 2006e). One ml of serum was extracted three times in ethyl acetate before high performance liquid chromatography (HPLC) purification using tetrahydrofuran, ethanol, and hexane in the mobile phase. All samples were injected in duplicate. The mean coefficients of variation for pregnenolone and allopregnanolone were 1.9 and 4.9%, respectively. The limit of detection with this method was 2 pg for both pregnenolone and allopregnanolone. Pregnenolone sulfate levels in serum were determined by radioimmunoassay as described earlier (Porcu et al, 2008), with modifications. Antiserum for pregnenolone sulfate (MP Biomedicals, Orangeburg, NY, USA) was diluted 1 : 300 to allow quantification of high pregnenolone sulfate levels observed in this study following treatment with adjunctive pregnenolone. The sensitivity of the assay was 50 pg; the mean intra-assay coefficient of variation was 13.1%. All other serum steroid levels were determined using the commercially available radioimmunoassay kits according to the manufacturer's directions (progesterone, cortisol, testosterone, free testosterone, and DHEAS: Diagnostic System Laboratories, Webster, TX, USA). DHEA serum levels were determined using a kit from ICN Pharmaceuticals (Costa Mesa, CA, USA).
Statistical Analysis
Primary end points in this pilot investigation were changes from baseline at Visit 2 following a 2-week placebo lead-in period (all patients) to final assessment at Visit 6 in cognitive symptoms (as assessed by BACS and MCCB composite scores) and negative symptoms (as assessed by SANS total scores). If the final Visit 6 assessment was missing for a subject (8 weeks of treatment with pregnenolone or placebo post-randomization), Visit 4 was carried forward for BACS, MCCB, SANS, and other psychiatric assessments (4 weeks of treatment with pregnenolone or placebo post-randomization). Student's t-tests were conducted on the change scores between treatment groups in this proof-of-concept study (two-tailed-α p=0.05 for each statistical test). Spearman's correlation coefficients were determined to assess the relationship between increases in serum pregnenolone levels and cognitive and psychiatric improvements, as well as the relationship between baseline neurosteroid levels and changes in these outcome measures following treatment with pregnenolone. Paired t-tests were used to assess pregnenolone and pregnenolone metabolite level changes in serum post-treatment.
RESULTS
Subject Characterization
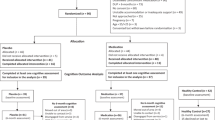
Of 28 subjects who received a screening visit, 21 met entry criteria and were randomized at Visit 2 to 8 weeks of treatment with adjunctive pregnenolone or placebo, following a 2-week single-blind placebo lead-in phase for all patients. The number of subjects who completed 4 or more weeks of treatment with pregnenolone or placebo post-randomization was 18 (86%), with 17 patients completing the entire 8-week study post-randomization (81%). One patient randomized to the placebo group completed only 4 weeks of the study secondary to requiring an increase in antipsychotic dose, thus excluding this subject from continued participation (Visit 4 assessments were thus carried forward for the statistical analyses). Baseline demographic and clinical characteristics are presented in Table 1. The mean age of subjects was 49.43 years (±12.19 SD) for the placebo group and 52.68 years (± 6.31 SD) for the pregnenolone group. The study sample contained only one female subject, reflecting the approximate demographic of the population with psychotic disorders treated at the Durham Veterans Affairs Medical Center.
Of 18 randomized subjects completing at least 4 weeks of the study, 3 were treated with aripiprazole, 8 with olanzapine, 3 with quetiapine, and 4 with risperidone (Table 1). Three of the 21 patients who were randomized did not complete at least 4 weeks of treatment with pregnenolone or placebo for the following reasons: (1) one patient began truck-driving school shortly after randomization at Visit 2 and his new schedule and location could not accommodate study visits; (2) one patient arrived intoxicated at Visit 4 following heavy alcohol and cocaine use that morning, and had taken his oral hypoglycemic without breakfast. He subsequently sustained an episode of hypoglycemia requiring medical attention that was believed to be unrelated to study drug, per internal medicine physician evaluation on the day of the event; and (3) one patient received an increase in antipsychotic prescribed by the subject's regular psychiatrist between Visit 2 and Visit 3, hence making the patient ineligible to continue in the study.
Missing data were addressed in the following manner. For cognitive assessments, any missing subscale was imputed as directed by BACS and MCCB guidelines, and these imputed values are included in the cognitive subscale tables for the BACS and MCCB described below. There were relatively few missing cognitive data for either the BACS or MCCB instruments, and testing sessions were generally very well tolerated. For the BACS, 1% of the total number of administered subscales was missing and required imputation (one symbol coding test and two token motor tests). For the MCCB, 1.5% of the total number of administered subscales was missing (two continuous performance tests (CPT) and five social cognition tests (MSCEIT)). One patient received BACS and MCCB cognitive batteries and CGI assessments at baseline, but could not complete several other rating scales (PANSS, SANS, Calgary Depression Rating Scale) secondary to a scheduling conflict. As sleep deprivation for 20–25 h significantly impacts cognitive testing performance in a manner comparable with a blood alcohol level of 0.10% (Dawson and Reid, 1997; Lamond and Dawson, 1999), cognitive data for one patient who reported sleep deprivation for the preceding 24 h at the final study visit could not be used; this patient's interim cognitive assessments from Visit 4 were thus carried forward for the statistical analyses. Other missing assessments were addressed through case-wise deletion (3 WRAT and 1 Calgary Depression Rating Scale), as were three outlying steroid levels greater than 2.4 SDs above the mean that were omitted from analyses as per statistical consultation. Of the serum estradiol and free testosterone levels determined at baseline and at the final study visit in both the pregnenolone and placebo groups (n=35; one randomized patient did not reach the final study visit as described above), six estradiol and two free testosterone levels were below the limits of detection of the RIA kits used in this investigation (8 and 0.15 pg/ml, respectively), and are thus not included in Table 5.
Pregnenolone Significantly Reduces SANS Scores Compared with Placebo
Baseline SANS scores were similar in both the pregnenolone and placebo groups (50.75±12.21 and 47.56±12.09 SD, respectively). Patients randomized to pregnenolone completing at least 4 weeks of treatment post-randomization demonstrated significantly improved SANS scores (mean change 10.38±10.18 SD) compared with patients receiving placebo (mean change 2.33±4.42 SD), unpaired Student's t-test of SANS change from baseline t=2.16, df 15, p=0.048, Table 2. Pregnenolone thus outperformed placebo by approximately 8 points on the SANS assessment, a difference that may be clinically relevant. SANS subscales are also provided in Table 2, although this information should be interpreted with caution given the small number of subjects in this study. This table does, however, provide data for future hypothesis testing with regard to domains of the SANS that may be responsive to a pregnenolone intervention. In the subscale analyses, uncorrected for multiple comparisons in this exploratory investigation, patients randomized to pregnenolone demonstrated significantly greater improvements in the ‘affect’ subscale of the SANS (t=2.33, df 15, p=0.035). There was also a trend for improvements in the ‘alogia’ SANS subscale (t=1.83, df=15, p=0.087) in the pregnenolone group.
BACS and MCCB Assessments
The mean composite changes in BACS and MCCB scores at 8 weeks compared with baseline were not significantly different in patients randomized to pregnenolone compared with the placebo group. The mean improvements in BACS composite scores in the pregnenolone group (z-score change 0.60±0.78 SD) were nonsignificantly greater than those in the placebo group (z-score change 0.22±0.47 SD) by a z-score of approximately 0.4 and approached a medium effect size in this small pilot study (p=0.22, t=1.27, df=16), Table 3. Individual BACS subscales are also presented in Table 3 for descriptive purposes to inform future hypothesis testing. BACS subscales that may demonstrate improvements in the pregnenolone group compared with the placebo group are verbal memory and the Tower of London tests (both with z-score improvements 0.61 greater than placebo), followed by the token motor and digit sequencing tasks in which the pregnenolone group demonstrated z-score improvements of 0.42 and 0.25, respectively, greater than placebo (Table 3). Mean improvements in MCCB composite scores were the same post-treatment in the pregnenolone (mean t-score change 7.00±8.87 SD) and placebo groups (mean t-score change 7.00±4.95 SD), a finding that appears driven by improvements in the MSCEIT subscale in the placebo group (Table 4). MCCB subscales that may demonstrate improvement include attention/vigilance (t-score improvement 6.89 greater than placebo), working memory (t-score improvement 4.00 greater than placebo), and verbal learning (t-score improvement 2.67 greater than placebo). Composite MCCB scores and BACS composite scores administered at baseline and post-treatment were positively correlated (Spearman's correlation coefficient 0.74, p<0.0001, n=36).
In the group randomized to pregnenolone, increases in serum levels of this neurosteroid predicted improvements in BACS composite scores (Spearman's rs=0.81, n=8, p=0.022), suggesting that peripheral pregnenolone levels may potentially have biomarker utility for the assessment of clinical response (Figure 1a). Serum pregnenolone levels tended to nonsignificantly predict improvements in MCCB composite scores (Spearman's rs=0.62, n=8, p=0.115), data not shown. Spearman's correlation coefficients were determined (rather than Pearson correlation coefficients) to reduce the influence of outliers. Serum increases in the GABAergic neurosteroid allopregnanolone also predicted improvements in BACS composite scores, Figure 1b (Spearman's rs=0.74, n=8, p=0.046). Serum increases in pregnenolone sulfate levels did not predict improvements in the BACS or MCCB composite scores (p>0.05 for both assessments). However, baseline pregnenolone sulfate levels were inversely correlated with improvements in MCCB composite scores (Spearman's rs=−0.83, n=8, p=0.015), suggesting that patients with lower pregnenolone sulfate levels at baseline experienced greater cognitive improvements as assessed by the MCCB following treatment with adjunctive pregnenolone (Figure 1c). Similarly, baseline pregnenolone (Spearman's rs=−0.76, n=8, p=0.037) and allopregnanolone (Spearman's rs=−0.83, n=8, p=0.015) levels were also inversely associated with improvements in MCCB composite scores. There was a trend for baseline pregnenolone levels to be inversely associated with improvements in BACS composite scores (r=−0.71, n=8, p=0.058).
(a) Increases in serum pregnenolone following treatment with this neurosteroid are correlated with improvements in cognitive performance, as assessed by composite BACS z-scores. (b) Increases in serum allopregnanolone following treatment with pregnenolone are correlated with cognitive improvement, as assessed by composite BACS z-scores. (c) Baseline pregnenolone sulfate levels are inversely associated with cognitive improvement, as assessed by composite MCCB t-scores.
Psychiatric Assessments
Patients randomized to pregnenolone demonstrate significantly improved final CGI-I scores (2.11±0.33 SD), compared with the group randomized to placebo (2.89±0.78 SD), unpaired Student's t-test p=0.015, t=2.75, df=16 (CGI-I of 2=much improved; CGI-I of 3=minimally improved), Table 5. The change was not reflected in CGI-S scores, however, with both pregnenolone and placebo showing persistent moderate symptoms (4.00±0.50 and 4.00±0.00 at baseline, respectively; 3.89±0.33 and 4.00±0.00 post-treatment, respectively), Table 5. PANSS scores were decreased by 4.43±3.59 more points in the pregnenolone group compared with the placebo group, but this finding was not significant (p=0.24, t=1.23, df=15), Table 5. There was a trend for pregnenolone administration to decrease the positive symptom subscale of the PANSS (p=0.069, t=1.96, df=15), but not the negative symptom or general subscales (Table 5). Negative symptom subscale scores of the PANSS were significantly correlated with total SANS scores in this pilot investigation (Spearman's r=0.58, p=0.0004, n=33, xy pairs consisting of baseline and week 8 scores for all patients for whom these data are available). Other psychiatric assessments did not show significant differences following treatment with pregnenolone compared with placebo (see Table 5 for summary of clinical rating scales).
Pregnenolone Administration Results in Increases in Serum Pregnenolone and Specific Downstream Metabolite Levels, Including the GABAergic Neurosteroid Allopregnanolone
Paired t-tests were used to determine if pregnenolone administration alters the serum concentrations of a number of downstream metabolites, including the GABAergic neurosteroid allopregnanolone and the NMDA receptor modulator pregnenolone sulfate. Treatment with pregnenolone resulted in fourfold elevations in serum levels of pregnenolone (paired t-test p=0.017, t=3.11, df=7), tripled serum pregnenolone sulfate levels (paired t-test p<0.0001, t=10.44, df=8), and increased the GABAergic neurosteroid allopregnanolone fivefold (paired t-test p=0.009, t=3.59, df=7) (Table 6). Pregnenolone administration also increased serum progesterone over fourfold and DHEAS levels by approximately 16% (Table 6). Treatment with pregnenolone did not increase serum testosterone, free testosterone, cortisol, DHEA, estradiol, or androstenedione levels (Table 6).
Side Effect Profiles in Patients Randomized to Pregnenolone and Placebo
There were no significant changes in most laboratory parameters, including glucose, triglycerides, HDL, TSH, and prolactin post-treatment compared with baseline in the pregnenolone group (Table 7). Cholesterol levels were significantly decreased following treatment with pregnenolone compared with baseline (paired t-test t=3.53, df=8, p=0.008); however, not all blood draws were conducted in a fasting state. Serum LDL levels were also significantly reduced in the pregnenolone group post-treatment (paired t-test t=5.16, df=6, p=0.002). There was no change in EKG QTc interval following treatment with pregnenolone (Table 7). Pregnenolone was very well tolerated. The only side effects present in the pregnenolone group to a greater degree than the placebo group were two reports of mild restlessness, one report of mild muscle pain/stiffness, and one report of mild cold extremities (Table 8).
DISCUSSION
The main finding of this pilot randomized placebo-controlled trial is that adjunctive pregnenolone significantly reduces negative symptoms in patients with schizophrenia or schizoaffective disorder as assessed by the SANS. In addition to the SANS, the two other primary end points for this study were the BACS and MCCB cognitive assessment batteries. The mean composite changes in BACS and MCCB scores post-treatment compared with baseline were not significantly different in patients randomized to pregnenolone compared with the placebo group. However, increases in serum pregnenolone and allopregnanolone levels predicted BACS composite scores post-treatment in the pregnenolone group. In addition, patients randomized to pregnenolone who demonstrated lower pregnenolone sulfate, pregnenolone, and allopregnanolone levels at baseline showed greater improvements in MCCB composite scores. These data suggest that adjunctive pregnenolone may have utility for negative symptoms and merits further investigation for cognitive symptoms in schizophrenia. Patients receiving adjunctive pregnenolone also demonstrated significantly improved CGI-I scores, although CGI-S scores remained unchanged. These findings, related results, and potential pregnenolone mechanisms of action are discussed below.
Adjunctive Pregnenolone Significantly Reduces Negative Symptoms
Treatment with adjunctive pregnenolone significantly reduced negative symptoms as assessed by SANS scores in patients with schizophrenia or schizoaffective disorder compared with placebo. Although these results should be interpreted with caution given small sample sizes, a significant effect on negative symptoms following pregnenolone treatment is encouraging and merits further investigation. In our exploratory analyses, individual subscales of the SANS were also investigated. Results suggest that the greatest improvements in negative symptoms following adjunctive pregnenolone occurred in the ‘affective flattening or blunting’ domain, with the next most pronounced improvements occurring in the ‘alogia’ and ‘anhedonia-asociality’ subscales. The change in ‘affective flattening or blunting’ was significantly greater in the pregnenolone group, uncorrected for multiple comparisons in this pilot study. As greater negative symptom improvement in the pregnenolone group appeared to occur among SANS subscales containing items that may overlap with depressive symptomatology (‘affective flattening or blunting’ and ‘anhedonia-asociality’), it is perhaps worth noting that patients with depressive symptoms demonstrate reductions in cerebrospinal fluid (CSF) pregnenolone levels (George et al, 1994). It is therefore possible that supplementation with pregnenolone may be particularly efficacious for negative symptoms with potential affective dimensions. Replication of these findings in a larger cohort of patients will thus be necessary to confirm potential pregnenolone effects on specific SANS subscale scores as well as total SANS scores, and to investigate the mechanism(s) of action contributing to the possible mitigation of negative symptoms by this neurosteroid.
A number of pregnenolone characteristics may play roles in the production of the aforementioned potential therapeutic effects. For example, pregnenolone enhances myelination (Koenig et al, 1995), increases neuritic outgrowth (Fontaine-Lenoir et al, 2006), and impacts microtubule polymerization and stability (Fontaine-Lenoir et al, 2006; Hsu et al, 2006; Murakami et al, 2000), actions that may be relevant to the pathophysiology of schizophrenia (Benitez-King et al, 2004; Glantz and Lewis, 2000; Hakak et al, 2001; Tkachev et al, 2007). Furthermore, we have determined earlier that clozapine markedly elevates pregnenolone levels in rat hippocampus and serum to a greater degree than other second-generation antipsychotics at doses producing comparable striatal D2 receptor occupancies, representing a candidate mechanism for its superior efficacy (Marx et al, 2006a). Recent evidence that clozapine enhances the binding of the translocator protein involved in the rate-limiting step leading to pregnenolone formation from cholesterol (formerly referred to as the peripheral-type benzodiazepine receptor, (Lacapere and Papadopoulos, 2003)) supports a role for this neurosteroid in clozapine mechanisms of action (Danovich et al, 2008). In addition, pregnenolone is present in human brain tissue at physiologically relevant concentrations in the nanomolar range that are greater than 10-fold higher than those frequently observed in serum or plasma (Marx et al, 2006c) and known to positively impact learning and memory (Flood et al, 1992). Pregnenolone is elevated in posterior cingulate and parietal cortex in patients with schizophrenia compared with control subjects, a finding that may represent compensatory changes and/or drug effects (Marx et al, 2006c), given earlier evidence that pharmacological agents such as clozapine and olanzapine elevate neurosteroids (Barbaccia et al, 2001; Marx et al, 2003, 2006a, 2006b). As neurosteroid induction may contribute to the therapeutic efficacy of certain antipsychotics, it is therefore logical to target pregnenolone as an adjunctive strategy in patients with schizophrenia.
On the basis of a strong rationale for possible NMDA receptor hypofunction in schizophrenia (Coyle, 2006; Javitt, 2004, 2007; Millan, 2005; Rujescu et al, 2006), a number of earlier investigations using compounds with modulatory activities at NMDA receptors such as D-serine (Heresco-Levy et al, 2005; Tsai et al, 1998, 1999), glycine (Buchanan et al, 2007; Heresco-Levy et al, 1996, 1999, 2004; Javitt et al, 2001), and D-cycloserine (Buchanan et al, 2007; Cascella et al, 1994; Duncan et al, 2004; Goff et al, 1995, 1996, 1999a, 1999b; Rosse et al, 1996; van Berckel et al, 1996) have been undertaken, with somewhat mixed findings. Because our data demonstrate that adjunctive pregnenolone administration significantly elevates serum levels of pregnenolone sulfate, a positive NMDA receptor modulator, it is possible that metabolism to this neurosteroid may contribute to its therapeutic efficacy for negative symptoms through this mechanism. It is unknown, however, if pregnenolone-induced increases in serum pregnenolone sulfate also lead to elevated pregnenolone sulfate levels in human brain. A rodent investigation suggests this may be the case (Wang et al, 1997), but the accurate determination of pregnenolone sulfate levels in brain tissue has also been the subject of several recent inquiries addressing possible confounding methodological challenges in the quantification of this neurosteroid (Ebner et al, 2006; Higashi et al, 2003a, 2003b; Liere et al, 2004; Liu et al, 2003; Schumacher et al, 2008). It is therefore possible that other mechanisms contribute to potential pregnenolone effects on negative symptoms that are unrelated to the NMDA receptor modulatory actions of its sulfated metabolite.
Adjunctive Pregnenolone and Cognition in Schizophrenia
Serum increases in pregnenolone in the group randomized to this neurosteroid are significantly correlated with cognitive improvement following this intervention as determined by the BACS assessment battery, a finding that may be encouraging with regard to the therapeutic potential of pregnenolone for cognitive symptoms in schizophrenia. This correlation may also highlight the biomarker potential of serum pregnenolone levels in predicting therapeutic response. Along these lines, lower baseline pregnenolone sulfate, pregnenolone, and allopregnanolone levels are also associated with greater improvements in MCCB composite scores. It is therefore possible that the determination of peripheral neurosteroid levels may have predictive utility for the identification of schizophrenia patients who would potentially benefit from a pregnenolone intervention and for the prediction of clinical efficacy.
This is the first report to the best of our knowledge to compare the BACS and MCCB cognitive assessment batteries within the same clinical trial. In this study, the composite scores of the BACS and MCCB assessments are positively correlated (Spearman's rs=0.74, n=36, p<0.0001). Treatment with adjunctive pregnenolone nonsignificantly improved composite BACS scores compared with placebo by a z-score of approximately 0.4, approaching a medium effect size if replicated in future studies adequately powered to detect this difference. There was no difference in mean composite MCCB t-score changes in the pregnenolone group compared with the placebo group post-treatment, a finding that appears to be driven by improved performances on the MSCEIT (social cognition domain test) by the placebo group. It is not clear why the placebo group outperformed the pregnenolone group on this particular MCCB measure, and this finding may have been impacted by a relatively larger number of missing MSCEIT assessments compared with other MCCB subscales. Larger randomized controlled trials will clearly be required to confirm initial findings regarding the potential for cognitive enhancement following treatment with pregnenolone.
Adjunctive Pregnenolone and Other Psychiatric Outcome Measures
Patients randomized to pregnenolone demonstrate significantly greater improvements in CGI-I scores, demonstrating a mean post-treatment CGI-I score of 2.11 (2=much improved) compared with mean CGI-I scores of 2.89 in patients receiving placebo (3=minimally improved). A significant finding in this overall improvement measure (p<0.015) is potentially encouraging in a pilot investigation of this size, but this result will require replication in a larger study, particularly as changes in the CGI-S measure were similar in both groups. Another measure of general patient functioning, the Heinrich Carpenter Quality of Life Scale, was not significantly altered post-treatment in this initial proof-of-concept trial, but an improvement of 5.27 points in the pregnenolone group compared with the placebo group was in the predicted direction (with possibly the greatest improvement in the ‘interpersonal and social work’ subscale). Together these findings suggest a potential signal for overall improvement following pregnenolone administration, but adequately powered controlled trials will be required to test this possibility.
With regard to PANSS total scores, patients randomized to pregnenolone demonstrated slightly greater improvements in this outcome measure compared with placebo (4.43 points), but the finding was not statistically significant. The negative symptom subscale of the PANSS was nonsignificantly improved to a modest degree by 1.53 points in the pregnenolone group compared with the placebo group. This result is not necessarily surprising, however, as the SANS demonstrates greater sensitivity for the assessment of this symptom domain compared with the PANSS negative symptom subscale, and hence the absence of a statistically significant effect may reflect limited power in this initial study of nine subjects per group. Nonetheless, the negative symptom subscale of the PANSS was significantly correlated with the SANS. Finally, there was a trend for treatment with pregnenolone to reduce the positive symptom subscale of the PANSS (p<0.07), a finding that merits further investigation.
Pregnenolone Levels in Serum and Pregnenolone Metabolism Profiles: Candidate Biomarkers and Potential Relevance to Mechanisms of Action
Adjunctive pregnenolone elevates serum pregnenolone levels
Pregnenolone administration in this study results in approximately fourfold elevations in serum pregnenolone to physiologically relevant nanomolar levels. Preclinical data support the possibility that elevations of pregnenolone levels to this extent could have significant beneficial effects. For example, pregnenolone enhances learning and memory in rodent models at even lower concentrations than the nanomolar serum concentrations achieved in the current investigation (Flood et al, 1992). As pregnenolone is lipophilic and readily crosses the blood–brain barrier, it is likely that brain concentrations of pregnenolone in humans are also elevated following pregnenolone administration, as suggested by animal studies (Wang et al, 1997). Furthermore, we have demonstrated earlier that serum pregnenolone levels are closely correlated with hippocampal pregnenolone levels in rats (Marx et al, 2006a), and that CSF pregnenolone levels in humans are correlated with temporal cortex pregnenolone levels within the same subject cohort (Naylor et al, 2008). Serum pregnenolone (and possibly other neurosteroids) may thus serve as a proxy or surrogate marker for brain pregnenolone levels, potentially providing data that may be relevant to the prediction of clinical response.
Pregnenolone metabolism to other neurosteroids
Metabolism to pregnenolone sulfate: Our data demonstrate that pregnenolone administration triples serum levels of its sulfated derivative, pregnenolone sulfate. Pregnenolone sulfate levels attained in serum following pregnenolone administration are very consistent with doses required to achieve its positive effects on learning and memory in rodent models (Akwa et al, 2001; Flood et al, 1992, 1995; Mathis et al, 1996; Meziane et al, 1996). Furthermore, recent evidence suggests that pregnenolone sulfate may positively modulate NMDA receptors at concentrations in the nanomolar range at binding sites distinct from a number of known NMDA receptor targets (Johansson et al, 2008). Pregnenolone sulfate in the nanomolar range also enhances long-term potentiation (Sliwinski et al, 2004) and influences GABA release (Mtchedlishvili and Kapur, 2003) in rodents. In addition to these actions, pregnenolone sulfate may increase neurogenesis in rodent hippocampus (Mayo et al, 2005). In this study, patients with lower serum pregnenolone sulfate levels at baseline demonstrated greater cognitive improvements as assessed by the MCCB. It is therefore possible that a subset of patients with schizophrenia may demonstrate relative pregnenolone sulfate deficits (as well as lower baseline pregnenolone and allopregnanolone levels) that are potentially restored to optimal levels with pregnenolone administration. Pregnenolone metabolism to pregnenolone sulfate could thus result in a number of additional mechanistic contributions for this neurosteroid and its effects on cognitive and negative symptoms, including the amelioration of hypothesized NMDA receptor hypofunction.
Metabolism to the GABAergic neurosteroid allopregnanolone: Pregnenolone administration results in fivefold elevations in serum allopregnanolone levels in this pilot investigation, and it is possible that pregnenolone metabolism to this downstream GABAergic neurosteroid metabolite may play a role in its therapeutic efficacy. Supporting this possibility, increases in allopregnanolone predicted cognitive improvement as assessed by BACS composite scores. Given compelling evidence for a GABAergic deficit in patients with schizophrenia (Benes and Berretta, 2001; Benes et al, 2007; Guidotti et al, 2005; Lewis et al, 2003, 2004, 2005) and the fact that allopregnanolone potentiates GABAA receptor responses to a greater degree than benzodiazepines or barbiturates (Majewska et al, 1986; Morrow et al, 1987, 1990), it is possible that pregnenolone metabolism to the GABAergic neurosteroid allopregnanolone may contribute to its mechanism(s) of action.
Allopregnanolone elevations resulting from treatment with pregnenolone may also play a role in other physiological processes related to schizophrenia, as this GABAergic neurosteroid enhances neurogenesis (Wang et al, 2005) and shows multiple pronounced neuroprotective properties (Djebaili et al, 2005; Griffin et al, 2004; Lockhart et al, 2002; Mellon et al, 2008; Sayeed et al, 2006; Xilouri and Papazafiri, 2006). In addition, it enhances myelination (Ghoumari et al, 2003) and possesses anticonvulsant actions (Kokate et al, 1994, 1996). Furthermore, allopregnanolone shows multiple anti-inflammatory effects (He et al, 2004; VanLandingham et al, 2007) and decreases apoptosis (Charalampopoulos et al, 2004, 2006; Xilouri and Papazafiri, 2006), actions that may be relevant to schizophrenia (Dickerson et al, 2007; Glantz et al, 2006; Jarskog et al, 2005; Knight et al, 2007; Lencz et al, 2007). Finally, allopregnanolone levels are decreased in postmortem brain tissue from patients with Alzheimer's disease (Marx et al, 2006e), and hence the restoration of allopregnanolone levels by precursor loading with pregnenolone may be a logical approach for a number of disorders in which the disruption of cognition is a salient characteristic.
Metabolism to progesterone intermediary: Abundant evidence demonstrates that progesterone plays an important role in a number of brain functions in addition to its well-characterized non-central nervous system effects. Progesterone is present in both male and female human brain in nanomolar concentrations (Lacroix et al, 1987; Lanthier and Patwardhan, 1986; Weill-Engerer et al, 2002). Progesterone administration results in pronounced neuroprotective effects in rodent models of traumatic brain injury (Djebaili et al, 2004, 2005; He et al, 2004; Jones et al, 2005; Robertson et al, 2006; Roof et al, 1997), and also positively impacts myelination processes (Azcoitia et al, 2003; Ghoumari et al, 2003; Ibanez et al, 2003; Koenig et al, 1995; Schumacher et al, 2000) and dendritic outgrowth during development (Sakamoto et al, 2001). Extending these rodent investigations, a recent randomized controlled clinical trial reported that intravenous progesterone for 3 days reduced 30-day mortality rates by over 50% in acute moderate-to-severe traumatic brain injury (Wright et al, 2007), strongly supporting a neuroprotective role for this neurosteroid. This pivotal study has been described as the first successful clinical trial of a pharmacological agent for traumatic brain injury in 40 years, with no adverse events attributable to the intervention (Stein, 2008; Wright et al, 2007). Furthermore, these promising clinical findings have recently been replicated, and also extended to demonstrate enduring therapeutic progesterone effects 6 months following traumatic brain injury (Xiao et al, 2008).
In this study, pregnenolone administration results in elevated progesterone levels, a finding that is not surprising as progesterone is an allopregnanolone precursor and a pregnenolone metabolite, hence representing an intermediary neurosteroid in the biosynthetic pathway. The mean serum progesterone elevations to 2.17 ng/ml following adjunctive pregnenolone in this pilot study represent levels that are somewhat higher than typical male serum progesterone ranges defined by the commercially available radioimmunoassay kit used in this investigation (serum range for males 0.10–1.17 ng/ml), but less than or comparable with those achieved in human male brain (Lacroix et al, 1987; Lanthier and Patwardhan, 1986; Weill-Engerer et al, 2002). It is also possible that induction of this neurosteroid intermediary may be relevant to pregnenolone mechanisms of action primarily because it is readily metabolized to the neuroprotective GABAergic neurosteroid allopregnanolone, a possibility supported by animal models of stroke (Sayeed et al, 2006) and seizures (Kokate et al, 1999).
Possible metabolism to DHEAS: DHEAS levels are significantly increased following pregnenolone administration, but the magnitude of this effect is relatively modest (approximately 16%). Given less pronounced increases in serum DHEAS levels following treatment with pregnenolone as well as the small sample size of the current pilot study, this result will require replication in a larger cohort of subjects. Nonetheless, an earlier investigation determined that DHEA administration significantly attenuated negative symptoms in patients with schizophrenia and resulted in concomitant elevations of its sulfated derivative, DHEAS (Strous et al, 2003). It is therefore possible that pregnenolone metabolism to DHEAS may be relevant to its therapeutic mechanism(s) of action.
Absence of conversion to other steroids: Pregnenolone administration for 8 weeks to patients with schizophrenia or schizoaffective disorder did not result in downstream elevations of cortisol, testosterone, free testosterone, DHEA, androstenedione, or estradiol (Table 6). As pregnenolone is a potential precursor to a number of steroids, pregnenolone could theoretically be metabolized to all of these molecules. Our data suggest, however, that pregnenolone metabolism is weighted toward biosynthetic pathways resulting in pregnenolone sulfate and allopregnanolone formation, rather than toward glucocorticoid or sex steroid synthesis involving testosterone or estradiol.
Tolerability and Safety
Pregnenolone was very well tolerated at the doses used in this pilot randomized controlled trial. Side effects reported at greater frequency than placebo included two instances of mild restlessness, one instance of mild cold extremities, and one instance of mild muscle pain/stiffness. No patients receiving pregnenolone experienced a serious adverse event related to study medication. Patients randomized to pregnenolone did not demonstrate significant weight gain, blood pressure, or pulse rate changes during the course of this study. Glucose levels were unchanged, as were serum electrolyte panels, TSH, prolactin levels, and liver function tests. Cholesterol levels were significantly decreased following 8 weeks of treatment with pregnenolone, but this result should be interpreted with caution, as not all blood draws were conducted in a fasting state. Interestingly, serum LDL levels were significantly decreased following adjunctive pregnenolone, a finding that may merit further investigation. As anticipated, pregnenolone serum levels at the completion of the study achieved or slightly exceeded pregnenolone levels observed in young adulthood (Morley et al, 1997).
Limitations
One of the main limitations of this pilot clinical trial is small sample size, and these initial results will clearly require replication in a larger cohort. In addition, only patients receiving second-generation antipsychotics were enrolled in this investigation, and hence it is unclear if these results are potentially generalizable to patients receiving first-generation agents. Only one female patient was enrolled in this study, constituting another limitation with regard to generalizability. The presence of other psychiatric medications in addition to second-generation antipsychotics was not exclusionary, possibly representing a confounding element, although no dose changes were permitted 4 weeks before the study and throughout the study duration. The optimal dosing for pregnenolone is not clear and pharmacokinetic data are currently very limited. Our dosing strategy in this study was very well tolerated and resulted in a significant reduction in negative symptoms and a possible signal for cognitive symptoms, but it is not known at present if other dosing approaches could potentially be more efficacious. These issues will need to be addressed in larger controlled studies. Using the current preliminary data to estimate statistical power requirements, a future investigation to begin to test hypotheses generated in this proof-of-concept study would optimally include at least 88 subjects (44 per group) to detect significant improvements in cognitive assessment composite scores following treatment with pregnenolone. A co-primary functional outcome measure would also be advantageous. Fewer patients would be required to test the hypothesis that pregnenolone significantly attenuates negative symptoms in schizophrenia. Other areas that will need to be addressed in future studies include potential sources of variability in neurosteroid levels, which may be impacted by factors such as age, smoking status, and concurrent medication use.
Summary
The results of this pilot randomized controlled trial investigating adjunctive pregnenolone as a treatment strategy for negative and cognitive symptoms in schizophrenia are promising and merit further study in a larger cohort of patients to attempt to replicate these initial findings. Pregnenolone was very well tolerated in this study and showed no untoward effects on weight, blood pressure, pulse, glucose, cholesterol, prolactin, or other monitored laboratory parameters. Candidate mechanisms for pregnenolone efficacy are diverse, and a number of theoretically coherent possibilities are supported by the existing preclinical and clinical literature. If these initial pilot findings are confirmed in larger randomized controlled trials, pregnenolone may represent a novel therapeutic advance for the treatment of cognitive and negative symptoms in schizophrenia.
References
Addington D, Addington J, Schissel B (1990). A depression rating scale for schizophrenics. Schizophr Res 3: 247–251.
Akwa Y, Ladurelle N, Covey DF, Baulieu EE (2001). The synthetic enantiomer of pregnenolone sulfate is very active on memory in rats and mice, even more so than its physiological neurosteroid counterpart: distinct mechanisms? Proc Natl Acad Sci USA 98: 14033–14037.
Andreasen N (1983). Scale for the Assessment of Negative Symptoms (SANS). University of Iowa: Iowa City.
Azcoitia I, Leonelli E, Magnaghi V, Veiga S, Garcia-Segura LM, Melcangi RC (2003). Progesterone and its derivatives dihydroprogesterone and tetrahydroprogesterone reduce myelin fiber morphological abnormalities and myelin fiber loss in the sciatic nerve of aged rats. Neurobiol Aging 24: 853–860.
Barbaccia ML, Affricano D, Purdy RH, Maciocco E, Spiga F, Biggio G (2001). Clozapine, but not haloperidol, increases brain concentrations of neuroactive steroids in the rat. Neuropsychopharmacology 25: 489–497.
Barnes TR (1989). A rating scale for drug-induced akathisia. Br J Psychiatry 154: 672–676.
Benes FM, Berretta S (2001). GABAergic interneurons: implications for understanding schizophrenia and bipolar disorder. Neuropsychopharmacology 25: 1–27.
Benes FM, Lim B, Matzilevich D, Walsh JP, Subburaju S, Minns M (2007). Regulation of the GABA cell phenotype in hippocampus of schizophrenics and bipolars. Proc Natl Acad Sci USA 104: 10164–10169.
Benitez-King G, Ramirez-Rodriguez G, Ortiz L, Meza I (2004). The neuronal cytoskeleton as a potential therapeutical target in neurodegenerative diseases and schizophrenia. Curr Drug Targets CNS Neurol Disord 3: 515–533.
Bowlby MR (1993). Pregnenolone sulfate potentiation of N-methyl-D-aspartate receptor channels in hippocampal neurons. Mol Pharmacol 43: 813–819.
Buchanan RW (2006). Important steps in the development of cognitive-enhancing drugs in schizophrenia. Am J Psychiatry 163: 1867–1869.
Buchanan RW (2007). Persistent negative symptoms in schizophrenia: an overview. Schizophr Bull 33: 1013–1022.
Buchanan RW, Davis M, Goff D, Green MF, Keefe RS, Leon AC et al (2005). A summary of the FDA-NIMH-MATRICS workshop on clinical trial design for neurocognitive drugs for schizophrenia. Schizophr Bull 31: 5–19.
Buchanan RW, Javitt DC, Marder SR, Schooler NR, Gold JM, McMahon RP et al (2007). The Cognitive and Negative Symptoms in Schizophrenia Trial (CONSIST): the efficacy of glutamatergic agents for negative symptoms and cognitive impairments. Am J Psychiatry 164: 1593–1602.
Carter CS, Barch DM, Buchanan RW, Bullmore E, Krystal JH, Cohen J et al (2008). Identifying cognitive mechanisms targeted for treatment development in schizophrenia: an overview of the first meeting of the Cognitive Neuroscience Treatment Research to Improve Cognition in Schizophrenia Initiative. Biol Psychiatry 64: 4–10.
Cascella NG, Macciardi F, Cavallini C, Smeraldi E (1994). D-cycloserine adjuvant therapy to conventional neuroleptic treatment in schizophrenia: an open-label study. J Neural Transm Gen Sect 95: 105–111.
Charalampopoulos I, Alexaki VI, Tsatsanis C, Minas V, Dermitzaki E, Lasaridis I et al (2006). Neurosteroids as endogenous inhibitors of neuronal cell apoptosis in aging. Ann NY Acad Sci 1088: 139–152.
Charalampopoulos I, Tsatsanis C, Dermitzaki E, Alexaki VI, Castanas E, Margioris AN et al (2004). Dehydroepiandrosterone and allopregnanolone protect sympathoadrenal medulla cells against apoptosis via antiapoptotic Bcl-2 proteins. Proc Natl Acad Sci USA 101: 8209–8214.
Cheney DL, Uzunov D, Guidotti A (1995). Pregnenolone sulfate antagonizes dizocilpine amnesia: role for allopregnanolone. Neuroreport 6: 1697–1700.
Coyle JT (2006). Glutamate and schizophrenia: beyond the dopamine hypothesis. Cell Mol Neurobiol 26: 365–384.
Danovich L, Veenman L, Leschiner S, Lahav M, Shuster V, Weizman A et al (2008). The influence of clozapine treatment and other antipsychotics on the 18 kDa translocator protein, formerly named the peripheral-type benzodiazepine receptor, and steroid production. Eur Neuropsychopharmacol 18: 24–33.
Darnaudery M, Koehl M, Pallares M, Le Moal M, Mayo W (1998). The neurosteroid pregnenolone sulfate increases cortical acetylcholine release: a microdialysis study in freely moving rats. J Neurochem 71: 2018–2022.
Darnaudery M, Pallares M, Piazza PV, Le Moal M, Mayo W (2002). The neurosteroid pregnenolone sulfate infused into the medial septum nucleus increases hippocampal acetylcholine and spatial memory in rats. Brain Res 951: 237–242.
Davison R, Koets P, Snow WG, Gabrielson CLG (1950). Effects of delta 5 pregnenolone in rheumatoid arthritis. Arch Intern Med 85: 365–389.
Dawson D, Reid K (1997). Fatigue, alcohol and performance impairment. Nature 388: 235.
Dickerson F, Stallings C, Origoni A, Boronow J, Yolken R (2007). C-reactive protein is associated with the severity of cognitive impairment but not of psychiatric symptoms in individuals with schizophrenia. Schizophr Res 93: 261–265.
Djebaili M, Guo Q, Pettus EH, Hoffman SW, Stein DG (2005). The neurosteroids progesterone and allopregnanolone reduce cell death, gliosis, and functional deficits after traumatic brain injury in rats. J Neurotrauma 22: 106–118.
Djebaili M, Hoffman SW, Stein DG (2004). Allopregnanolone and progesterone decrease cell death and cognitive deficits after a contusion of the rat pre-frontal cortex. Neuroscience 123: 349–359.
Duncan EJ, Szilagyi S, Schwartz MP, Bugarski-Kirola D, Kunzova A, Negi S et al (2004). Effects of D-cycloserine on negative symptoms in schizophrenia. Schizophr Res 71: 239–248.
Ebner MJ, Corol DI, Havlikova H, Honour JW, Fry JP (2006). Identification of neuroactive steroids and their precursors and metabolites in adult male rat brain. Endocrinology 147: 179–190.
First M, Spitzer R, Gibbon M, Williams J (1996). Structured clinical interview for DSM-IV axis I disorders-patient edition (SCID-I/P, version 2.0).
Flood JF, Morley JE, Roberts E (1992). Memory-enhancing effects in male mice of pregnenolone and steroids metabolically derived from it. Proc Natl Acad Sci USA 89: 1567–1571.
Flood JF, Morley JE, Roberts E (1995). Pregnenolone sulfate enhances post-training memory processes when injected in very low doses into limbic system structures: the amygdala is by far the most sensitive. Proc Natl Acad Sci USA 92: 10806–10810.
Fontaine-Lenoir V, Chambraud B, Fellous A, David S, Duchossoy Y, Baulieu EE et al (2006). Microtubule-associated protein 2 (MAP2) is a neurosteroid receptor. Proc Natl Acad Sci USA 103: 4711–4716.
Freeman H, Pincus G, Bachrach S, Johnson CW, McCabe GE, MacGilpin H (1950a). Oral steroid medication in rheumatoid arthritis. J Clin Endocrinol Metab 10: 1523–1532.
Freeman H, Pincus G, Johnson CW, Bachrach S, McCabe GE, MacGilpin H (1950b). Therapeutic efficacy of delta5-pregnenolone in rheumatoid arthritis. JAMA 142: 1124–1127.
George MS, Guidotti A, Rubinow D, Pan B, Mikalauskas K, Post RM (1994). CSF neuroactive steroids in affective disorders: pregnenolone, progesterone, and DBI. Biol Psychiatry 35: 775–780.
Ghoumari AM, Ibanez C, El-Etr M, Leclerc P, Eychenne B, O'Malley BW et al (2003). Progesterone and its metabolites increase myelin basic protein expression in organotypic slice cultures of rat cerebellum. J Neurochem 86: 848–859.
Glantz LA, Gilmore JH, Lieberman JA, Jarskog LF (2006). Apoptotic mechanisms and the synaptic pathology of schizophrenia. Schizophr Res 81: 47–63.
Glantz LA, Lewis DA (2000). Decreased dendritic spine density on prefrontal cortical pyramidal neurons in schizophrenia. Arch Gen Psychiatry 57: 65–73.
Goff DC, Henderson DC, Evins AE, Amico E (1999a). A placebo-controlled crossover trial of D-cycloserine added to clozapine in patients with schizophrenia. Biol Psychiatry 45: 512–514.
Goff DC, Tsai G, Levitt J, Amico E, Manoach D, Schoenfeld DA et al (1999b). A placebo-controlled trial of D-cycloserine added to conventional neuroleptics in patients with schizophrenia. Arch Gen Psychiatry 56: 21–27.
Goff DC, Tsai G, Manoach DS, Coyle JT (1995). Dose-finding trial of D-cycloserine added to neuroleptics for negative symptoms in schizophrenia. Am J Psychiatry 152: 1213–1215.
Goff DC, Tsai G, Manoach DS, Flood J, Darby DG, Coyle JT (1996). D-cycloserine added to clozapine for patients with schizophrenia. Am J Psychiatry 153: 1628–1630.
Green MF (2006). Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. J Clin Psychiatry 67: e12.
Green MF, Kern RS, Braff DL, Mintz J (2000). Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the ‘right stuff’? Schizophr Bull 26: 119–136.
Griffin LD, Gong W, Verot L, Mellon SH (2004). Niemann-Pick type C disease involves disrupted neurosteroidogenesis and responds to allopregnanolone. Nat Med 10: 704–711.
Guest CM, Kammerer WH, Cecil RL, Berson SA (1950). Epinephrine, pregnenolone and testosterone in the treatment of rheumatoid arthritis. JAMA 143: 338–344.
Guidotti A, Auta J, Davis JM, Dong E, Grayson DR, Veldic M et al (2005). GABAergic dysfunction in schizophrenia: new treatment strategies on the horizon. Psychopharmacology (Berl) 180: 191–205.
Hakak Y, Walker JR, Li C, Wong WH, Davis KL, Buxbaum JD et al (2001). Genome-wide expression analysis reveals dysregulation of myelination-related genes in chronic schizophrenia. Proc Natl Acad Sci USA 98: 4746–4751.
Harvey PD, Green MF, Keefe RS, Velligan DI (2004). Cognitive functioning in schizophrenia: a consensus statement on its role in the definition and evaluation of effective treatments for the illness. J Clin Psychiatry 65: 361–372.
He J, Evans CO, Hoffman SW, Oyesiku NM, Stein DG (2004). Progesterone and allopregnanolone reduce inflammatory cytokines after traumatic brain injury. Exp Neurol 189: 404–412.
Heinrichs DW, Hanlon TE, Carpenter Jr WT (1984). The Quality of Life Scale: an instrument for rating the schizophrenic deficit syndrome. Schizophr Bull 10: 388–398.
Henderson E, Weinberg M, Wright WA (1950). Pregnenolone. J Clin Endocrinol Metab 10: 455–474.
Heresco-Levy U, Ermilov M, Lichtenberg P, Bar G, Javitt DC (2004). High-dose glycine added to olanzapine and risperidone for the treatment of schizophrenia. Biol Psychiatry 55: 165–171.
Heresco-Levy U, Javitt DC, Ebstein R, Vass A, Lichtenberg P, Bar G et al (2005). D-serine efficacy as add-on pharmacotherapy to risperidone and olanzapine for treatment-refractory schizophrenia. Biol Psychiatry 57: 577–585.
Heresco-Levy U, Javitt DC, Ermilov M, Mordel C, Horowitz A, Kelly D (1996). Double-blind, placebo-controlled, crossover trial of glycine adjuvant therapy for treatment-resistant schizophrenia. Br J Psychiatry 169: 610–617.
Heresco-Levy U, Javitt DC, Ermilov M, Mordel C, Silipo G, Lichtenstein M (1999). Efficacy of high-dose glycine in the treatment of enduring negative symptoms of schizophrenia. Arch Gen Psychiatry 56: 29–36.
Higashi T, Daifu Y, Ikeshima T, Yagi T, Shimada K (2003a). Studies on neurosteroids XV. Development of enzyme-linked immunosorbent assay for examining whether pregnenolone sulfate is a veritable neurosteroid. J Pharm Biomed Anal 30: 1907–1917.
Higashi T, Sugitani H, Yagi T, Shimada K (2003b). Studies on neurosteroids XVI. Levels of pregnenolone sulfate in rat brains determined by enzyme-linked immunosorbent assay not requiring solvolysis. Biol Pharm Bull 26: 709–711.
Hsu HJ, Liang MR, Chen CT, Chung BC (2006). Pregnenolone stabilizes microtubules and promotes zebrafish embryonic cell movement. Nature 439: 480–483.
Ibanez C, Shields SA, El-Etr M, Leonelli E, Magnaghi V, Li WW et al (2003). Steroids and the reversal of age-associated changes in myelination and remyelination. Prog Neurobiol 71: 49–56.
Irwin RP, Lin SZ, Rogawski MA, Purdy RH, Paul SM (1994). Steroid potentiation and inhibition of N-methyl-D-aspartate receptor-mediated intracellular Ca++ responses: structure-activity studies. J Pharmacol Exp Ther 271: 677–682.
Jarskog LF, Glantz LA, Gilmore JH, Lieberman JA (2005). Apoptotic mechanisms in the pathophysiology of schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 29: 846–858.
Javitt DC (2004). Glutamate as a therapeutic target in psychiatric disorders. Mol Psychiatry 9: 984–997.
Javitt DC (2007). Glutamate and schizophrenia: phencyclidine, N-Methyl-D-aspartate receptors, and dopamine-glutamate interactions. Int Rev Neurobiol 78: 69–108.
Javitt DC, Silipo G, Cienfuegos A, Shelley AM, Bark N, Park M et al (2001). Adjunctive high-dose glycine in the treatment of schizophrenia. Int J Neuropsychopharmacol 4: 385–391.
Johansson T, Frandberg PA, Nyberg F, Le Greves P (2008). Molecular mechanisms for nanomolar concentrations of neurosteroids at NR1/NR2B receptors. J Pharmacol Exp Ther 324: 759–768.
Jones NC, Constantin D, Prior MJ, Morris PG, Marsden CA, Murphy S (2005). The neuroprotective effect of progesterone after traumatic brain injury in male mice is independent of both the inflammatory response and growth factor expression. Eur J Neurosci 21: 1547–1554.
Kay SR, Fiszbein A, Opler LA (1987). The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13: 261–276.
Keefe RS, Bilder RM, Davis SM, Harvey PD, Palmer BW, Gold JM et al (2007). Neurocognitive effects of antipsychotic medications in patients with chronic schizophrenia in the CATIE Trial. Arch Gen Psychiatry 64: 633–647.
Keefe RS, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L (2004). The Brief Assessment of Cognition in Schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res 68: 283–297.
Keefe RS, Harvey PD, Goldberg TE, Gold JM, Walker TM, Kennel C et al (2008). Norms and standardization of the Brief Assessment of Cognition in Schizophrenia (BACS). Schizophr Res 102: 108–115.
Kirkpatrick B, Fenton WS, Carpenter Jr WT, Marder SR (2006). The NIMH-MATRICS consensus statement on negative symptoms. Schizophr Bull 32: 214–219.
Knight JG, Menkes DB, Highton J, Adams DD (2007). Rationale for a trial of immunosuppressive therapy in acute schizophrenia. Mol Psychiatry 12: 424–431.
Koenig HL, Schumacher M, Ferzaz B, Thi AN, Ressouches A, Guennoun R et al (1995). Progesterone synthesis and myelin formation by Schwann cells. Science 268: 1500–1503.
Kokate TG, Banks MK, Magee T, Yamaguchi S, Rogawski MA (1999). Finasteride, a 5alpha-reductase inhibitor, blocks the anticonvulsant activity of progesterone in mice. J Pharmacol Exp Ther 288: 679–684.
Kokate TG, Cohen AL, Karp E, Rogawski MA (1996). Neuroactive steroids protect against pilocarpine- and kainic acid-induced limbic seizures and status epilepticus in mice. Neuropharmacology 35: 1049–1056.
Kokate TG, Svensson BE, Rogawski MA (1994). Anticonvulsant activity of neurosteroids: correlation with gamma-aminobutyric acid-evoked chloride current potentiation. J Pharmacol Exp Ther 270: 1223–1229.
Lacapere JJ, Papadopoulos V (2003). Peripheral-type benzodiazepine receptor: structure and function of a cholesterol-binding protein in steroid and bile acid biosynthesis. Steroids 68: 569–585.
Lacroix C, Fiet J, Benais JP, Gueux B, Bonete R, Villette JM et al (1987). Simultaneous radioimmunoassay of progesterone, androst-4-enedione, pregnenolone, dehydroepiandrosterone and 17-hydroxyprogesterone in specific regions of human brain. J Steroid Biochem 28: 317–325.
Ladurelle N, Eychenne B, Denton D, Blair-West J, Schumacher M, Robel P et al (2000). Prolonged intracerebroventricular infusion of neurosteroids affects cognitive performances in the mouse. Brain Res 858: 371–379.
Lamond N, Dawson D (1999). Quantifying the performance impairment associated with fatigue. J Sleep Res 8: 255–262.
Lanthier A, Patwardhan VV (1986). Sex steroids and 5-en-3 β-hydroxysteroids in specific regions of the human brain and cranial nerves. J Steroid Biochem 25: 445–449.
Lencz T, Morgan TV, Athanasiou M, Dain B, Reed CR, Kane JM et al (2007). Converging evidence for a pseudoautosomal cytokine receptor gene locus in schizophrenia. Mol Psychiatry 12: 572–580.
Lewis DA, Glantz LA, Pierri JN, Sweet RA (2003). Altered cortical glutamate neurotransmission in schizophrenia: evidence from morphological studies of pyramidal neurons. Ann NY Acad Sci 1003: 102–112.
Lewis DA, Hashimoto T, Volk DW (2005). Cortical inhibitory neurons and schizophrenia. Nat Rev Neurosci 6: 312–324.
Lewis DA, Volk DW, Hashimoto T (2004). Selective alterations in prefrontal cortical GABA neurotransmission in schizophrenia: a novel target for the treatment of working memory dysfunction. Psychopharmacology (Berl) 174: 143–150.
Liere P, Pianos A, Eychenne B, Cambourg A, Liu S, Griffiths W et al (2004). Novel lipoidal derivatives of pregnenolone and dehydroepiandrosterone and absence of their sulfated counterparts in rodent brain. J Lipid Res 45: 2287–2302.
Liu S, Sjovall J, Griffiths WJ (2003). Neurosteroids in rat brain: extraction, isolation, and analysis by nanoscale liquid chromatography-electrospray mass spectrometry. Anal Chem 75: 5835–5846.
Lockhart EM, Warner DS, Pearlstein RD, Penning DH, Mehrabani S, Boustany RM (2002). Allopregnanolone attenuates N-methyl-D-aspartate-induced excitotoxicity and apoptosis in the human NT2 cell line in culture. Neurosci Lett 328: 33–36.
Majewska MD, Harrison NL, Schwartz RD, Barker JL, Paul SM (1986). Steroid hormone metabolites are barbiturate-like modulators of the GABA receptor. Science 232: 1004–1007.
Marder SR (2006). Drug initiatives to improve cognitive function. J Clin Psychiatry 67 (Suppl 9): 31–35; discussion 36–42.
Marder SR, Fenton W (2004). Measurement and Treatment Research to Improve Cognition in Schizophrenia: NIMH MATRICS initiative to support the development of agents for improving cognition in schizophrenia. Schizophr Res 72: 5–9.
Marx CE, Shampine LJ, Duncan GE, VanDoren MJ, Grobin AC, Massing MW et al (2006a). Clozapine markedly elevates pregnenolone in rat hippocampus, cerebral cortex, and serum: candidate mechanism for superior efficacy? Pharmacol Biochem Behav 84: 598–608.
Marx CE, Shampine LJ, Khisti RT, Trost WT, Bradford DW, Grobin AC et al (2006b). Olanzapine and fluoxetine administration and coadministration increase rat hippocampal pregnenolone, allopregnanolone and peripheral deoxycorticosterone: implications for therapeutic actions. Pharmacol Biochem Behav 84: 609–617.
Marx CE, Stevens RD, Shampine LJ, Uzunova V, Trost WT, Butterfield MI et al (2006c). Neuroactive steroids are altered in schizophrenia and bipolar disorder: relevance to pathophysiology and therapeutics. Neuropsychopharmacology 31: 1249–1263.
Marx CE, Trost WT, Shampine L, Behm FM, Giordano LA, Massing MW et al (2006d). Neuroactive steroids, negative affect, and nicotine dependence severity in male smokers. Psychopharmacology (Berl) 186: 462–472.
Marx CE, Trost WT, Shampine LJ, Stevens RD, Hulette CM, Steffens DC et al (2006e). The neurosteroid allopregnanolone is reduced in prefrontal cortex in Alzheimer's disease. Biol Psychiatry 60: 1287–1294.
Marx CE, VanDoren MJ, Duncan GE, Lieberman JA, Morrow AL (2003). Olanzapine and clozapine increase the GABAergic neuroactive steroid allopregnanolone in rodents. Neuropsychopharmacology 28: 1–13.
Mathis C, Paul SM, Crawley JN (1994). The neurosteroid pregnenolone sulfate blocks NMDA antagonist-induced deficits in a passive avoidance memory task. Psychopharmacology (Berl) 116: 201–206.
Mathis C, Vogel E, Cagniard B, Criscuolo F, Ungerer A (1996). The neurosteroid pregnenolone sulfate blocks deficits induced by a competitive NMDA antagonist in active avoidance and lever-press learning tasks in mice. Neuropharmacology 35: 1057–1064.
Mayo W, Dellu F, Robel P, Cherkaoui J, Le Moal M, Baulieu EE et al (1993). Infusion of neurosteroids into the nucleus basalis magnocellularis affects cognitive processes in the rat. Brain Res 607: 324–328.
Mayo W, Lemaire V, Malaterre J, Rodriguez JJ, Cayre M, Stewart MG et al (2005). Pregnenolone sulfate enhances neurogenesis and PSA-NCAM in young and aged hippocampus. Neurobiol Aging 26: 103–114.
McGavack TH, Chevalley J, Weissberg J (1951). The use of delta 5-pregnenolone in various clinical disorders. J Clin Endocrinol Metab 11: 559–577.
Meieran SE, Reus VI, Webster R, Shafton R, Wolkowitz OM (2004). Chronic pregnenolone effects in normal humans: attenuation of benzodiazepine-induced sedation. Psychoneuroendocrinology 29: 486–500.
Mellon SH, Gong W, Schonemann MD (2008). Endogenous and synthetic neurosteroids in treatment of Niemann-Pick Type C disease. Brain Res Rev 57: 410–420.
Meziane H, Mathis C, Paul SM, Ungerer A (1996). The neurosteroid pregnenolone sulfate reduces learning deficits induced by scopolamine and has promnestic effects in mice performing an appetitive learning task. Psychopharmacology (Berl) 126: 323–330.
Millan MJ (2005). N-Methyl-D-aspartate receptors as a target for improved antipsychotic agents: novel insights and clinical perspectives. Psychopharmacology (Berl) 179: 30–53.
Morley JE, Kaiser F, Raum WJ, Perry III HM, Flood JF, Jensen J et al (1997). Potentially predictive and manipulable blood serum correlates of aging in the healthy human male: progressive decreases in bioavailable testosterone, dehydroepiandrosterone sulfate, and the ratio of insulin-like growth factor 1 to growth hormone. Proc Natl Acad Sci USA 94: 7537–7542.
Morrow AL, Pace JR, Purdy RH, Paul SM (1990). Characterization of steroid interactions with gamma-aminobutyric acid receptor-gated chloride ion channels: evidence for multiple steroid recognition sites. Mol Pharmacol 37: 263–270.
Morrow AL, Suzdak PD, Paul SM (1987). Steroid hormone metabolites potentiate GABA receptor-mediated chloride ion flux with nanomolar potency. Eur J Pharmacol 142: 483–485.
Mtchedlishvili Z, Kapur J (2003). A presynaptic action of the neurosteroid pregnenolone sulfate on GABAergic synaptic transmission. Mol Pharmacol 64: 857–864.
Murakami K, Fellous A, Baulieu EE, Robel P (2000). Pregnenolone binds to microtubule-associated protein 2 and stimulates microtubule assembly. Proc Natl Acad Sci USA 97: 3579–3584.
Naylor JC, Hulette CM, Steffens DC, Shampine LJ, Ervin JF, Payne VM et al (2008). Cerebrospinal fluid dehydroepiandrosterone levels are correlated with brain dehydroepiandrosterone levels, elevated in Alzheimer's disease, and related to neuropathological disease stage. J Clin Endocrinol Metab 93: 3173–3178.
Nuechterlein K, Green MF (2006). MATRICS Consensus Cognitive Battery (MCCB). MATRICS Assessments Inc.: Los Angeles.
Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD et al (2008). The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. Am J Psychiatry 165: 203–213.
Pallares M, Darnaudery M, Day J, Le Moal M, Mayo W (1998). The neurosteroid pregnenolone sulfate infused into the nucleus basalis increases both acetylcholine release in the frontal cortex or amygdala and spatial memory. Neuroscience 87: 551–558.
Pincus G, Hoagland H (1944). Effects of administered pregnenolone on fatiguing psychomotor performance. J Aviation Med 15: 98–115.
Pincus G, Hoagland H (1945a). Effects on industrial production of the administration of Δ5 pregnenolone to factory workers, I. Psychosomatic Medicine 7: 342–346.
Pincus G, Hoagland H (1945b). Effects on industrial production of the administration of Δ5 pregnenolone to factory workers, II. Psychosomatic Medicine 7: 347–352.
Porcu P, O'Buckley TK, Morrow AL, Adinoff B (2008). Differential hypothalamic-pituitary-adrenal activation of the neuroactive steroids pregnenolone sulfate and deoxycorticosterone in healthy controls and alcohol-dependent subjects. Psychoneuroendocrinology 33: 214–226.
Roberts E (1995). Pregnenolone—from Selye to Alzheimer and a model of the pregnenolone sulfate binding site on the GABAA receptor. Biochem Pharmacol 49: 1–16.
Robertson CL, Puskar A, Hoffman GE, Murphy AZ, Saraswati M, Fiskum G (2006). Physiologic progesterone reduces mitochondrial dysfunction and hippocampal cell loss after traumatic brain injury in female rats. Exp Neurol 197: 235–243.
Romeo E, Cheney DL, Zivkovic I, Costa E, Guidotti A (1994). Mitochondrial diazepam-binding inhibitor receptor complex agonists antagonize dizocilpine amnesia: putative role for allopregnanolone. J Pharmacol Exp Ther 270: 89–96.
Roof RL, Hoffman SW, Stein DG (1997). Progesterone protects against lipid peroxidation following traumatic brain injury in rats. Mol Chem Neuropathol 31: 1–11.
Rosse RB, Fay-McCarthy M, Kendrick K, Davis RE, Deutsch SI (1996). D-cycloserine adjuvant therapy to molindone in the treatment of schizophrenia. Clin Neuropharmacol 19: 444–450.
Rujescu D, Bender A, Keck M, Hartmann AM, Ohl F, Raeder H et al (2006). A pharmacological model for psychosis based on N-methyl-D-aspartate receptor hypofunction: molecular, cellular, functional and behavioral abnormalities. Biol Psychiatry 59: 721–729.
Sakamoto H, Ukena K, Tsutsui K (2001). Effects of progesterone synthesized de novo in the developing Purkinje cell on its dendritic growth and synaptogenesis. J Neurosci 21: 6221–6232.
Sayeed I, Guo Q, Hoffman SW, Stein DG (2006). Allopregnanolone, a progesterone metabolite, is more effective than progesterone in reducing cortical infarct volume after transient middle cerebral artery occlusion. Ann Emerg Med 47: 381–389.
Schumacher M, Akwa Y, Guennoun R, Robert F, Labombarda F, Desarnaud F et al (2000). Steroid synthesis and metabolism in the nervous system: trophic and protective effects. J Neurocytol 29: 307–326.
Schumacher M, Liere P, Akwa Y, Rajkowski K, Griffiths W, Bodin K et al (2008). Pregnenolone sulfate in the brain: a controversial neurosteroid. Neurochem Int 52: 522–540.
Simpson GM, Angus JW (1970). A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl 212: 11–19.
Sliwinski A, Monnet FP, Schumacher M, Morin-Surun MP (2004). Pregnenolone sulfate enhances long-term potentiation in CA1 in rat hippocampus slices through the modulation of N-methyl-D-aspartate receptors. J Neurosci Res 78: 691–701.
Stein DG (2008). Progesterone exerts neuroprotective effects after brain injury. Brain Res Rev 57: 386–397.
Strous RD, Maayan R, Lapidus R, Stryjer R, Lustig M, Kotler M et al (2003). Dehydroepiandrosterone augmentation in the management of negative, depressive, and anxiety symptoms in schizophrenia. Arch Gen Psychiatry 60: 133–141.
Tkachev D, Mimmack ML, Huffaker SJ, Ryan M, Bahn S (2007). Further evidence for altered myelin biosynthesis and glutamatergic dysfunction in schizophrenia. Int J Neuropsychopharmacol 10: 557–563.
Tsai G, Yang P, Chung LC, Lange N, Coyle JT (1998). D-serine added to antipsychotics for the treatment of schizophrenia. Biol Psychiatry 44: 1081–1089.
Tsai GE, Yang P, Chung LC, Tsai IC, Tsai CW, Coyle JT (1999). D-serine added to clozapine for the treatment of schizophrenia. Am J Psychiatry 156: 1822–1825.
Vallee M, Mayo W, Darnaudery M, Corpechot C, Young J, Koehl M et al (1997). Neurosteroids: deficient cognitive performance in aged rats depends on low pregnenolone sulfate levels in the hippocampus. Proc Natl Acad Sci USA 94: 14865–14870.
Vallee M, Shen W, Heinrichs SC, Zorumski CF, Covey DF, Koob GF et al (2001). Steroid structure and pharmacological properties determine the anti-amnesic effects of pregnenolone sulphate in the passive avoidance task in rats. Eur J Neurosci 14: 2003–2010.
van Berckel BN, Hijman R, van der Linden JA, Westenberg HG, van Ree JM, Kahn RS (1996). Efficacy and tolerance of D-cycloserine in drug-free schizophrenic patients. Biol Psychiatry 40: 1298–1300.
VanLandingham JW, Cekic M, Cutler S, Hoffman SW, Stein DG (2007). Neurosteroids reduce inflammation after TBI through CD55 induction. Neurosci Lett 425: 94–98.
Wang JM, Johnston PB, Ball BG, Brinton RD (2005). The neurosteroid allopregnanolone promotes proliferation of rodent and human neural progenitor cells and regulates cell-cycle gene and protein expression. J Neurosci 25: 4706–4718.
Wang MD, Wahlstrom G, Backstrom T (1997). The regional brain distribution of the neurosteroids pregnenolone and pregnenolone sulfate following intravenous infusion. J Steroid Biochem Mol Biol 62: 299–306.
Weill-Engerer S, David JP, Sazdovitch V, Liere P, Eychenne B, Pianos A et al (2002). Neurosteroid quantification in human brain regions: comparison between Alzheimer's and nondemented patients. J Clin Endocrinol Metab 87: 5138–5143.
Wright DW, Kellermann AL, Hertzberg VS, Clark PL, Frankel M, Goldstein FC et al (2007). ProTECT: a randomized clinical trial of progesterone for acute traumatic brain injury. Ann Emerg Med 49: 391–402.
Wu FS, Gibbs TT, Farb DH (1991). Pregnenolone sulfate: a positive allosteric modulator at the N-methyl-D-aspartate receptor. Mol Pharmacol 40: 333–336.
Xiao G, Wei J, Yan W, Wang W, Lu Z (2008). Improved outcomes from the administration of progesterone for patients with acute severe traumatic brain injury: a randomized controlled trial. Crit Care 12: R61.
Xilouri M, Papazafiri P (2006). Anti-apoptotic effects of allopregnanolone on P19 neurons. Eur J Neurosci 23: 43–54.
Acknowledgements
This work was supported by the following sources: The VA Mid-Atlantic Mental Illness, Research, Education, and Clinical Center, VA Advanced Research Career Development Award (CEM), K23 MH65080 (CEM), National Alliance for Research on Schizophrenia and Affective Disorders (CEM), Durham VA REAP (PI Roger D. Madison, PhD), R37AA10564 (ALM), VA Career Development Award (JLS). We thank Gillian Parke for her excellent assistance with this project.
Author information
Authors and Affiliations
Corresponding author
Additional information
DISCLOSURE OF COMPENSATION OVER THE LAST 3 YEARS/CONFLICT OF INTEREST
Dr Marx has no compensation to disclose over the last 3 years. Dr Marx is a co-applicant on a pending US patent application on the use of neurosteroids for the treatment of central nervous system disorders. She is an unpaid scientific advisor and board member of NeuroScience Pharmaceuticals. Dr Keefe has received compensation from the following sources: Astra-Zeneca, Cyberonics, Gabriel Pharmaceuticals, Organon Pharmaceuticals, Otsuka, Pfizer, Saegis, Abbott, Acadia, BiolineRx, Bristol-Myers Squibb, Cephalo, Cortex, Dainippon Sumitomo Pharmaceutical, Eli Lilly, Johnson & Johnson, Lundbeck, Memory Pharmaceuticals, Merck, Orexigen, Sanofi/Aventis, Shering-Plough, Wyeth, and Xenoport. Dr Keefe is a contributor to a pending US patent application on the use of neurosteroids for the treatment of central nervous system disorders. Dr Keefe receives royalties for two of the cognitive test batteries used in this study, the BACS and the MATRICS Consensus Cognitive Battery. Dr Buchanan has received compensation from the following sources: Astra-Zeneca, GlaxoSmithKline, Janssen, Merck, Natixis Bleichroeder, Organon, Ortho-McNeil, Pfizer, Sanofi-Aventis, Solvay Pharmaceuticals, and Wyeth. Dr Hamer has received compensation from the following sources: Acadia, Allergan, Alpharma, Astra-Zeneca, Cenerx, Corcept, EnabledMD, Epix, Johnson & Johnson, Pfizer, Schwartz, Solvay Pharmaceuticals, Sanofi-Aventis, Takeda, and Wyeth. Dr Kilts, Dr Bradford, Dr Strauss, Dr Naylor, Dr Payne, Ms Leimone, Dr Dunn, Dr Porcu, Dr Morrow, and Mr Shampine have no compensation to disclose over the last 3 years. Dr Lieberman has received compensation from the following sources: Astra-Zeneca, Eli Lilly, Forest Laboratories, GlaxoSmithKline, Pfizer, Wyeth, Solvay Pharmaceuticals, Bristol-Myers Squibb, Janssen, and Repligen. Dr Savitz has received compensation from the following sources: Astra-Zeneca, Sanofi-Aventis, Janssen, and Pfizer.
Rights and permissions
About this article
Cite this article
Marx, C., Keefe, R., Buchanan, R. et al. Proof-of-Concept Trial with the Neurosteroid Pregnenolone Targeting Cognitive and Negative Symptoms in Schizophrenia. Neuropsychopharmacol 34, 1885–1903 (2009). https://doi.org/10.1038/npp.2009.26
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2009.26
Keywords
This article is cited by
-
Novel neurosteroid therapeutics for post-partum depression: perspectives on clinical trials, program development, active research, and future directions
Neuropsychopharmacology (2024)
-
Negative symptoms and neurocognition in drug-naïve schizophrenia: moderating role of plasma neutrophil gelatinase-associated lipocalin (NGAL) and interferon-gamma (INF-γ)
European Archives of Psychiatry and Clinical Neuroscience (2023)
-
Effects of Blockade of Cholinesterase on Negative Disorders in Schizophrenia
Neuroscience and Behavioral Physiology (2022)
-
Alteration of the steroidogenesis in boys with autism spectrum disorders
Translational Psychiatry (2020)
-
Biomarker screening for antenatal depression in women who underwent caesarean section: a matched observational study with plasma Lipidomics
BMC Psychiatry (2019)