Abstract
Given the key role CD8+ T cells play in controlling viral infection, strategies to enhance these responses may have important clinical applications. We found that in vivo CD137 stimulation with an agonistic monoclonal antibody enhanced the primary CD8+ T cell response to influenza type A viral infection in mice. Stimulation of CD137 increased the absolute number of CD8+ T cells to influenza epitopes in the lungs of infected animals, preferentially expanded CD8+ T cells that recognized nondominant epitopes and greatly enhanced direct ex vivo cytotoxicity. CD137 stimulation also restored the CD8+ T cell response to the immunodominant influenza epitope in CD28−/− mice. Thus, in vivo CD137 stimulation enhances and broadens the CD8+ T cell response to influenza virus and can restore the CD8+ T cell response when CD28 costimulation is absent. This suggests that CD137 stimulation may be useful as a strategy to enhance the CD8+ T cell response to viruses.
Similar content being viewed by others
Main
CD8+ T cells are critical in the control and clearance of viral infections. Strategies that enhance CD8+ T cell responses therefore may prove invaluable as therapeutic strategies against viral infections and for vaccine development. One such strategy is the exploitation of CD8+ T cell costimulation to enhance primary CD8+ T cell responses against viruses. CD137 (also known as 4-1BB) is a member of the tumor necrosis factor receptor (TNFR) family that is expressed on activated T1,2 and NK cells3. Its ligand, CD137L, is found on activated B cells, macrophages and dendritic cells4,5,6. CD137 can costimulate T cell activation and proliferation1,4,7,8 and may enhance the survival of activated T cells5,9. Costimulation through CD137 preferentially induces T helper type 1 (TH1) responses10 and CD8+ T cell proliferation11,12 and can mediate costimulation in vitro in the absence of CD2813,14,15. Stimulation of CD137 provides protection against tumors by enhancing antitumor T cell responses16 and is required for optimal CD8+ T cell responses to viruses12,17. These data suggest that stimulating CD137 may enhance cytotoxic CD8+ T cell responses in vivo.
Here, we examined directly the in vivo effect of CD137 costimulation on the primary CD8+ T cell response to respiratory influenza type A viral infection. We found that although CD137 costimulation enhanced the CD8+ T cell response to the immunodominant nucleoprotein NP(366–374) epitope, the effect was more marked with CD8+ T cells specific for the matrix 1 M1(128–135), nonstructural 2 NS2(114–121) and polymerase 2 PA(224–233) epitopes, thereby broadening the CD8+ T cell response. In influenza virus–infected CD28−/− mice that had reduced CD8+ T cell responses to the immunodominant NP(366–374) peptide, CD137 stimulation resulted in the restoration of this response to wild-type amounts. Thus, costimulation of CD137 may prove useful as a strategy to augment antiviral CD8+ T cell responses.
Results
Effects of CD137 stimulation on CD8+ T cell responses
To assess the effects of CD137 stimulation on CD8+ T cell responses to respiratory influenza type A virus infection, we examined the virus-specific CD8+ T cell response in the lungs of influenza virus–infected mice. We used a total lung digestion procedure to isolate pulmonary lymphocytes18,19 that allowed the analysis of individual mice. Stimulation of CD137 with an agonistic monoclonal antibody (mAb) decreased the frequency of NP(366–374)-specific CD8+ T cells as a percentage of total recovered CD8+ T cells from the lungs; this was measured by NP(366–374) tetramer staining (6.32 ± 1.06% CD137 mAb–treated versus 9.23 ± 1.56% untreated, n = 16) (Fig. 1a,b). No cells stained positive for Sendai virus–specific NP(324–332) tetramer, which was used as a negative control. Isotype control mAb–treated mice (8.86 ± 3.78%, n = 6) did not differ from untreated animals. Costimulation of CD137, however, increased the absolute number of pulmonary NP(366–374)-specific CD8+ T cells (4.19 × 105 ± 1.34 × 105 CD137 mAb–treated versus 2.45 × 105 ± 0.77 × 105 untreated per lung, n = 16) (Fig. 1c). Isotype control mAb–treated mice did not differ from untreated animals (1.40 × 105 ± 0.70 × 105, n = 6).
Pulmonary lymphocytes were collected from CD137 mAb–treated mice 10 days after intranasal infection with PR8 influenza virus and were stained with CD8 mAb and Db-NP(366–374) tetramers. (a) Representative FACS plots showing NP(366–374) tetramer staining cells in the lung lymphocytes of untreated, CD137 mAb–treated or isotype control mAb–treated mice. Numbers indicate the percentages of CD8+ T cells that stained positive for the NP(366–374) tetramer. (b) Pooled data showing the frequency of pulmonary lymphocytes that stained positive for NP(366–374) tetramer. (c) Absolute numbers of NP(366–374)-specific CD8+ T cells in the lungs of CD137 mAb–treated (n = 16), untreated (n = 16) or isotype control mAb–treated (n = 6) mice. (b,c) Pooled data from five independent experiments are shown.
We also analyzed the NP(366–374)-specific CD8+ T cell response by measuring interferon-γ (IFN-γ)–producing CD8+ T cells after in vitro stimulation of lung mononuclear cells with the NP(366–374) peptide. Similar to the tetramer results, CD137 stimulation increased the absolute number of lung NP(366–374)-specific CD8+ T cells (3.53 × 105 ± 1.48 × 105 CD137 mAb–treated versus 1.20 × 105 ± 0.43 × 105 untreated, n = 8) and decreased the frequency of NP(366–374)-specific CD8+ T cells as a frequency of total CD8+ T cells (5.73 ± 1.25% CD137 mAb–treated versus 11.10 ± 1.48% untreated, n = 8, P<0.01). Isotype control mAb–treated animals did not show a difference in either frequency (10.84 ± 2.00%, n = 6) or absolute numbers (1.35 × 105 ± 0.50 × 105, n = 6) of NP(366–374)-specific CD8+ T cells.
In the above experiments, we also analyzed the total number of CD8+ T cells in the lungs of treated and untreated mice after influenza virus infection. Although the frequency of NP(366–374)-specific CD8+ T cells had decreased, we observed a significant increase in frequency (40.9 ± 4.07% CD137 mAb–treated versus 25.2 ± 2.74% untreated, n = 16, P<0.001) (Fig. 2a,b) and absolute numbers (5.75 × 106 ± 1.63 × 106 CD137 mAb–treated versus 2.27 × 106 ± 0.58 × 106 untreated, n = 16, P<0.002) (Fig. 2c) of CD8+ T cells in the lung parenchyma. Also, CD137 stimulation had no significant effect on the expression of cell-surface activation markers on NP(366–374)-specific CD8+ T cells. Expression of the early activation marker CD69 and the interleukin 2 receptor α chain (IL-2Rα, also known as CD25) did not differ, and NP(366–374)-specific CD8+ T cells showed the characteristic CD44hiCD62Llo phenotype of effector-memory CD8+ T cells (data not shown). Stimulation of CD137 had no effect on the kinetics of CD8+ T cell migration to the lungs on days 5 and 7 after infection (data not shown). Thus, we observed an increase in the absolute numbers of NP(366–374)-specific CD8+ T cells in the lungs of CD137 mAb–treated mice, but a decrease in frequency of CD8+ T cells specific for the immunodominant NP(366–374) epitope. Because most responding CD8+ T cells in the lung are virus-specific rather than bystanders20, we hypothesized that CD137 costimulation may enhance the CD8+ T cell response to other influenza-specific epitopes.
Pulmonary lymphocytes were collected 10 days after intranasal infection with influenza virus and were stained with CD8 mAb. (a) Representative histogram plots showing CD8+ T cell staining of pulmonary lymphocytes. Numbers indicate the percentages of lymphocytes that stained positive for CD8. (b) The percentages of lymphocytes that stained positive for CD8 in five independent experiments are shown; *P<0.001. (c) The absolute numbers of CD8+ T cells in the lungs of CD137 mAb–treated (n = 16), untreated (n = 16) or isotype control mAb–treated (n = 6) mice; *P<0.002. Pooled data from five independent experiments are shown; significant differences were determined with paired Student's t-tests,.
CD137 stimulation and nondominant epitopes
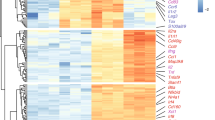
We investigated the possibility that CD137 stimulation may be enhancing the response to other influenza-specific epitopes. After in vitro peptide stimulation we examined the CD8+ T cell response to the H-2Kb–restricted M1(128–135) and NS2(114–121) epitopes and the H-2Db–restricted PA(224–233) epitope21,22 by intracellular IFN-γ staining (Fig. 3a). The “dominance” of CD8+ T cells specific for various epitopes was revealed by enumerating the epitope-specific CTLs as a percentage of the total number of CD8+ T cells. This method of analysis showed that stimulation of CD137 increased the frequency of CD8+ T cells specific for the M1(128–135), NS2(114–121) and PA(224–233) epitopes within the CD8+ T cell population as a measure of total CD8+ T cells (Fig. 3b). Stimulation of CD137 altered the dominance hierarchy so that the NP(366–374) epitope became the least dominant, as measured by IFN-γ production.
Pulmonary lymphocytes were collected 10 days after intranasal infection with influenza virus and intracytoplasmic IFN-γ was determined by flow cytometry after peptide stimulation. (a) Representative FACS plots show intracytoplasmic IFN-γ staining after M1(128–135) peptide stimulation. Numbers indicate the percentages of lymphocytes that stained positive for both IFN-γ and CD8. Pooled data from three independent experiments (n = 8 in each group) show the frequency of virus-specific IFN-γ–producing CD8+ T cells as a measure of (b) total CD8+ T cells (*P<0.01) (c) total pulmonary lymphocytes (*P<0.05; **P<0.02) and (d) the absolute numbers of virus-specific cells per lung (*P<0.05; **P<0.01). Significant differences were determined with paired Student's t-tests. (e) Representative experiment showing the direct ex vivo cytotoxic activity of pulmonary lymphocytes against target cells loaded with the indicated peptides.
We also evaluated the data as the percentage of total lymphocytes. When enumerated in this manner, CD137 stimulation significantly increased the percentage of M1(128–135)-specific (3.64 ± 0.66% CD137 mAb–treated versus 2.03 ± 0.63% untreated, n = 8, P<0.05), NS2(114–121)-specific (4.91 ± 0.90% CD137 mAb–treated versus 2.29 ± 0.74% untreated, n = 8, P<0.02) and PA(224–233)-specific CD8+ T cells (4.87 ± 0.89% CD137 mAb–treated versus 2.82 ± 1.01% untreated, n = 4) while having no effect on the percentage of NP(366–374)-specific CD8+ T cells as a measure of total lymphocytes (2.91 ± 0.82% CD137 mAb–treated versus 2.84 ± 0.61% untreated) (Fig. 3c). Isotype control mAb treatment had no effect on these epitope-specific responses (Fig. 3c). In addition, CD137 stimulation also significantly increased the absolute number of CD8+ T cells specific for the M1(128–135) (4.06 × 105 ± 1.35 × 105 CD137 mAb–treated versus 1.00 × 105 ± 0.41 × 105 untreated, n = 8, P<0.05), NS2(114–121) (5.48 × 105 ± 1.85 × 105 CD137 mAb–treated versus 1.09 × 105 ± 0.49 × 105 untreated, n = 8, P<0.01) and PA(224–233) (4.85 × 105 ± 1.80 × 105 CD137 mAb–treated versus 1.36 × 105 ± 0.72 × 105 untreated, n = 4) (Fig. 3d). Absolute numbers of epitope-specific CD8+ T cells did not differ between untreated and isotype control mAb–treated groups (Fig. 3d).
CD137 stimulation and ex vivo cytotoxicity
To determine whether the CD137 stimulation–induced increase in epitope-specific CD8+ T cells also resulted in increased cytotoxicity to cells presenting influenza virus peptides, we examined major histocompatibility complex (MHC) class I peptide–specific cytoxicity to peptide-loaded EL-4 cells in a 51Cr-release assay. In vivo CD137 stimulation did not enhance NP(366–374)-specific cytotoxicity of lung lymphocytes. However, CD137 stimulation augmented cytotoxicity to M1(128–135), NS2(114–121) and the PA(224–233) peptide-loaded target cells (Fig. 3e).
CD137 stimulation and the humoral response
Stimulation of CD137 abrogates T cell–dependent humoral responses23, possibly through the induction of T cell anergy24. Thus, we examined whether in vivo treatment with the agonistic CD137 mAb affected the immunoglobulin M (IgM) and IgG antibody responses to influenza virus. CD137 stimulation slightly, but not significantly, increased anti–influenza IgM compared to untreated controls (4.7 ± 0.9 antibody units for CD137 mAb–treated versus 4.2 ± 1.0 antibody units for untreated, n = 6) while decreasing anti–influenza IgG (2.6 ± 0.6 antibody units for CD137 mAb–treated versus 3.8 ± 0.8 antibody units for untreated, n = 6).
CD137 stimulation of CD28−/− mice
To examine whether CD137 stimulation could substitute CD28 costimulation and act in its absence, we treated influenza-infected CD28−/− mice with CD137 mAb. We found that CD28−/− mice did not mount a significant CD8+ T cell response to influenza virus, which confirmed published data that examined CD8+ T cell responses to influenza virus under costimulation-deficient conditions25 (Fig. 4a). The immunodominant NP(366–374)-specific CD8+ T cell response to influenza virus infection was almost completely abrogated in terms of absolute numbers (2.63 × 105 ± 1.0 × 105 in wild-type versus 0.37 × 105 ± 0.2 × 105 in CD28−/− mice, n = 12, P<0.05) and frequency (8.01 ± 1.4% in wild-type versus 1.41 ± 0.22% in CD28−/− mice, n = 12, P<0.002) of CD8+ T cells in the lungs. Stimulation of CD137 restored both the absolute number (2.6 × 105 ± 1.2 × 105) and frequency (7.1 ± 1.2%) of NP(366–374)-specific CD8+ T cells, as a measure of total CD8+ T cells, to wild-type amounts (Fig. 4a–d). Direct ex vivo NP(366–374)-specific cytotoxicity was greatly reduced in lung lymphocytes of CD28−/− mice infected with influenza virus, and this was also restored by CD137 stimulation to wild-type amounts (Fig. 4e). Thus, CD137 stimulation can substitute CD28 costimulation in the generation of a primary CD8+ T cell response to influenza type A viral infection.
Pulmonary lymphocytes were collected 10 days after intranasal infection with influenza virus and were stained with CD8 mAb and Db–NP(366–374) tetramers. (a) Representative flow cytometry plots are shown. Numbers indicate the percentages of CD8+ T cells that stained positive for the NP(366–374) tetramer. Pooled data from five independent experiments (n = 12 in each group) show cells that stained positive for CD8 and NP(366–374) tetramer as a measure of (b) total CD8+ T cells (c) total lymphocytes and (d) the absolute numbers of NP(366–374)-specific CD8+ T cells. (e) Representative experiment showing cytotoxicity of pulmonary lymphocytes against NP(366–374) peptide–loaded target cells.
Discussion
We show here that CD137 mAb increased the total number of virus-specific T cells in the lungs. However, the frequency of CD8+ T cells directed against the immunodominant epitope decreased, whereas the frequency of CD8+ T cells that responded to minor epitopes was enhanced. The biological significance of such increases is not known at present because CD8+ T cells are not protective during a primary influenza infection26. However, because CD8+ T cell memory is dependent upon the primary clonal burst size27, CD137 stimulation—by enhancing the primary response—may prove advantageous in increasing and broadening CD8+ T cell memory. It remains to be seen what effect stimulation of CD137 has on the generation and maintenance of CD8+ T cell memory.
The mechanisms that control immunodominance in MHC class I–restricted T cell responses are complex and largely unresolved. Both the quantities of peptide–MHC class I complexes expressed on antigen-presenting cells (APCs), which are governed by efficient processing and adequate binding of MHC class I, and the CD8+ T cell repertoire that binds to these complexes appear to be critical21,28,29. A number of studies have indicated that costimulation may influence the peptide hierarchy of the T cell response. In the absence of CD28 costimulation for example, in CD8+ T cells, responses are exclusively directed against immunodominant tumor peptides, whereas CD8+ T cell responses against subdominant epitopes occur only when CD28 costimulation is present30. Increasing responses against subdominant epitopes by costimulating with mAb in vivo, however, has yet to be shown. The increase in CD8+ T cell responses to epitopes other than the immunodominant epitope that we observed with CD137 mAb treatment may be biologically important because responses to subdominant peptides provide protection against lethal challenge with influenza virus31.
A number of mechanisms may be responsible for the enhancing and broadening effect of CD137 stimulation on the CD8+ T cell response. Stimulation of CD137 may act directly on naïve CD8+ T cells and lower their activation threshold for T cell receptor (TCR)-induced T cell activation, as is the case for CD2832. In CD4+ T cells, weak agonist MHC class II peptides can be converted into strong agonists by CD28 costimulation of CD4+ T cells and this is most likely due to lowering of the activation threshold33. CD137 signaling may synergize with the TCR signal at the level of the Jnk (c-Jun NH2-terminal kinase) and such synergy could potentially amplify a weak TCR signal generated by subdominant peptides, which results in full activation of the CD8+ T cell34,35. This was in agreement with published studies showing that CD137 is required for optimal activation, expansion and differentiation of CD8+ T cells36. It is possible, however, that the enhancement of CD8+ T cell responses by CD137 mAb treatment is due to the costimulation and activation of CD4+ T cells, thereby increasing T helper cell activity. This is an unlikely mechanism, however, as primary cytotoxic CD8+ T cell responses to viral infections are unaffected when CD4 is absent37,38,39, and we have found that the NP(366–374)-specific CD8+ T cell response to influenza type A infection is CD4+ T cell independent (E. S. Halstead and P. D. Katsikis, unpublished data). Whether CD8+ T cell responses to other influenza-specific epitopes also exhibit such CD4+ T cell–independence is unknown at present.
Although CD137 has not been reported to be expressed on APCs, we cannot exclude the possibility that the CD137 mAb acts directly or indirectly on the APCs rather than CD8+ T cells. Cytokines can have multiple effects on peptide presentation by APCs, one of which is modifying the proteosome and thus affecting peptide generation29, thereby increasing the presentation of subdominant peptides by MHC class I. However, the M1(128–135) epitope is processed efficiently, binds strongly to MHC class I and yet does not elicit a strong CTL response, apparently due to the low avidity of M1(128–135)-specific TCRs for the cognate peptide-MHC class I complex21. Therefore, these data suggest that CD137 stimulation acts directly on CD8+ T cells and decreases the threshold of activation governed by TCR-peptide–MHC class I avidity rather than CD4+ T cells or antigen presentation by APCs.
In influenza-infected mice, responding effector CD8+ CTLs have been divided into type 1 (TC1) and type 2 (TC2) cells, based on cytokine secretion and migration subpopulations. TC1 cells produce IFN-γ and tend to migrate to the site of infection, whereas TC2 cells produce IL-4 and IL-10 and tend to stay in the draining lymph node40. An alternative explanation for our findings is that CD137 stimulation causes a redistribution of CD8+ T cells via type-switching, with TC2 cells switching to TC1 cells with consequential enhanced homing to the infected pulmonary parenchyma. This is unlikely because the response to influenza in C57BL/6J mice is dominated by a TH1 response41, an environment that does not favor TC2 cell development. In addition, with intracellular staining, we did not detect any IL-4– or IL-10–producing CD8+ T cells in either the lungs or mediastinal lymph nodes of infected C57BL/6 mice in either untreated or CD137 mAb–treated mice (data not shown).
CD137 stimulation in vivo inhibits humoral responses to various antigens23,24. In our model, agonistic CD137 mAb treatment slightly increased anti–influenza IgM and decreased anti–influenza IgG amounts. Whether this is the result of CD137 stimulation inhibiting B cells or deleting them is not clear. CD137L-transgenic mice suffer from a progressive loss of B cells42. The mechanism behind the progressive B cell depletion and reduced antibody production may be Fas-induced apoptosis of B cells because CD137 stimulation increases the expression of FasL on CD4+ T cells43.
Our results may explain the mechanism by which poorly immunogenic tumors were made immunogenic and were, in fact, rejected by mice treated with an agonistic CD137 mAb16. Our data indicate that CD137 stimulation may overcome the lack of CD28 costimulation by tumor cells and that the antitumor response may be broadened to subdominant epitopes. Such CD8+ T cells generated against subdominant epitopes can eliminate tumors in mice, indicating that responses to subdominant peptides can be functional and biologically significant in vivo30.
Our findings show that in vivo CD137 costimulation enhances the primary CD8+ T cell response to influenza virus. CD137 costimulation broadens the virus-specific CD8+ T cell response by increasing the numbers and frequency of CD8+ T cells directed against nondominant peptides and, most importantly, cytotoxic activity against these peptides. Finally, in vivo CD137 stimulation restores the primary CD8+ T cell responses to the immunodominant NP(366–374) epitope when CD28 costimulation is absent. The above suggest that in vivo CD137 stimulation may prove useful as a strategy for enhancing the CD8+ T cell response to viruses.
Methods
Animals and reagents.
Specific pathogen–free 6- to 8-week-old female C57BL/6J (wild-type) and B6.129S2-CD28tm1Mak (CD28−/−) mice were from The Jackson Laboratory (Bar Harbor, ME) and were maintained in an AAALAC-certified barrier facility at MCP Hahnemann University. All animal work was done with IACUC approval. The A/Puerto Rico/8/34 (PR8, H1N1) influenza virus strain was a gift of W. Gerhard (The Wistar Institute, Philadelphia, PA). The M6 agonistic rat IgG2a mAb to CD137 was a gift of B. Gliniak (Immunex, Seattle, WA). Monoclonal rat anti–KLH was used as an IgG2a isotype–control mAb and was from eBioscience (San Diego, CA). All antibodies were endotoxin-negative and contained no azide. The influenza virus–specific MHC class I H-2Db–NP(366–374) and Sendai virus–specific MHC class I H-2Db–NP(324–332) tetramers were prepared as described44. The H-2Db–binding NP(366–374), ASNENMETM, and PA(224–233), SSLENFRAYV, influenza peptides and the H-2Kb–binding M1(128–135), MGLIYNRM, and NS2(114–121), RTFSFQLI, influenza peptides were from Genosys (The Woodlands, TX).
Influenza virus infections.
Mice were anesthetized by intraperitoneal (i.p.) injection with 2,2,2 tribromoethanol (240 mg/kg, Acros, Belgium) and intranasally infected with 4 hemagglutinin units (HAU) of PR8 influenza virus in 20 μl of PBS (Mediatech, Herndon, VA) on day 0. The M6 CD137 mAb and the isotype control antibodies were administered by i.p. injection (100 μg per injection) on days 0, 3 and 7 after infection. All cells were collected on day 10 after infection. All mice were age- and cage-matched and all statistical analyses were performed with a paired Student's t-test.
Pulmonary lymphocyte isolation.
Single cell suspensions of lung parenchymal cells were prepared by digesting lungs from individual mice with Collagenase A and DNAse I (3.0 mg/ml and 0.15 mg/ml respectively, Roche Molecular Biochemicals, Indianapolis, IN) in sterile RPMI 1640 (Mediatech) with 10% heat-inactivated fetal bovine serum (FBS, Mediatech) for 2 h at 37 °C on a rocker. The lung digest was passed through a 40-μm sterile nylon cell strainer (Becton Dickinson, San Jose, CA). Single cell suspensions were washed (all washes done with sterile RPMI 1640 with 5% heat-inactivated FBS) and mononuclear cells were isolated by density gradient centrifugation with Lympholyte-M (Cedarlane Laboratories Limited, Ontario, Canada) at 1300g at room temperature for 20 min. Lung mononuclear cells were resuspended in RPMI complete media (with 10% heat-inactivated FBS, 10 μg/ml of penicillin and streptomycin, 0.2 mM l-glutamine and 5.5 μM 2-mercaptoethanol). Cells were counted with acridine orange (3 μg/ml) and ethidium bromide (5 μg/ml) stains (Sigma-Aldrich, St. Louis, MO) to visualize live and dead cells under ultraviolet light.
Flow cytometry.
CD8+ T cells specific for NP(366–374) were quantified and phenotyped with MHC class I H-2Db–NP(366–374) tetramers. The Sendai virus–specific H-2Db-NP(324–332) tetramer was used as a control. The tetramers were formed by complexing the peptide-loaded MHC monomers to allophycocyanin-strepavidin (Molecular Probes, Eugene, OR). The following four-color combinations of fluorochrome-conjugated mAbs were used for immunofluorescent staining: FITC–anti-CD44 (IM7) and PE–anti-CD62L (Mel-14), FITC–anti-CD69 (H1.2F3) and PE–anti-CD25 (PC61) and FITC–anti-CD4 (RM4-5) and PE–anti-NK1.1 (PK136) all in combination with Cy5PE–anti-CD8α (53–6.7) and allophycocyanin-tetramer. All fluorochrome-conjugated mAbs were from eBioscience. Cells were stained and washed in Hank's buffered salt solution (HBSS, Mediatech) with 2% heat inactivated FBS and 0.02% sodium azide. Cell staining was done at 4 °C for 30 min. Cells were washed twice and fixed with 1% paraformaldehyde. Events were acquired with a FACSCalibur flow cytometer with Cell Quest (Becton Dickinson) software and data were analyzed with FlowJo software (TreeStar, Mountain View, CA).
Cytotoxicity assay.
Pulmonary CTL activity was analyzed directly ex vivo against EL-4 target cells that were pulsed with 1 μg/ml of MHC class I viral peptide for 6 h. Five-million peptide-loaded EL-4 target cells were labeled with 100 μCi of 51Cr for 90 min at 37 °C. Cells were washed twice and resuspended in RPMI complete media. Target cells (1 × 104 targets/well) were incubated with different numbers of effector cells in 96-well V-bottomed Costar cell culture plates (Corning, NY), centrifuged for 1 min at 200g, then incubated for 6 h at 37 °C in a 5% CO2 incubator. After incubation, cells were centrifuged for 5 min at 500g. Culture supernatants (30 μl) were transferred to 96-well Lumaplates (Packard Instrument Company, Downers Grove, IL), dried overnight and counted with a Top Count-NXT luminescence scintillation counter (Packard Instrument Company). The percentage lysis calculation was done as follows: 100 × (cpm experimental − cpm spontaneous)/(cpm maximum − cpm spontaneous). Maximum 51Cr release was assessed via lysis with 5% Triton-X100 solution. Spontaneous 51Cr release was typically 10–15% of the maximum release.
Intracellular IFN-γ staining.
Lung mononuclear cells (1.0 × 106) were cultured in 100 μl of RPMI complete media with 10 μg/ml of brefeldin A in 5-ml sterile polystyrene round-bottomed tubes in the presence or absence of 10 μg/ml of virus-specific peptides. Cells were incubated for 6 h at 37 °C in a 5% CO2 incubator. After culture, the cells were first surface-stained with mAb as detailed above then fixed and permeabilized with Cytofix-Cytoperm (Pharmingen, La Jolla, CA) for 20 min at 4 °C. Cells were stained for the intracellular accumulation of IFN-γ with an allophycocyanin-conjugated IFN-γ mAb (eBioscience) for 15 min at 4 °C. Cells were washed with Perm/Wash buffer (Pharmingen) and fixed with 1% paraformaldehyde. Events were acquired using a FACSCalibur flow cytometer with CellQuest software (Becton Dickinson) and data were analyzed with FlowJo software (TreeStar).
Serum antibody titers.
Serum IgM and IgG influenza antibodies were measured in serum by ELISA. Blood from individual infected mice was coagulated and centrifuged for 20 min at 10,000g at 4 °C and serum was isolated and stored at −80 °C. Maxisorb ELISA plates (Nalge Nunc International, Rochester, NY) were coated with 200 HAU/ml of influenza PR8 virus in carbonate buffer (pH 9.5) overnight at 4 °C. Plates were washed three times with PBS, 0.05% Tween 20 (Fisher Scientific, Fair Lawn, NJ) in-between each step. Nonspecific binding was blocked with 2% BSA (Sigma-Aldrich) in PBS for 2 h at 37 °C. The plates were then incubated with serial dilutions of serum in PBS, 2% BSA for 2 h at room temperature. Anti–influenza IgG and IgM were detected with horseradish peroxidase-conjugated goat anti–mouse IgG (Cedarlane Laboratories) and goat anti–mouse IgM (Pierce, Rockland, IL). Plates were washed five times and enzyme activity was detected with TMB (3,3′,5,5′- tetramethyl-benzidine) substrate (KPL, Gaithersburg, MD) and absorbance measured at 450 nm with a Spectramax Plus 384 microplate reader (Molecular Devices, Sunnyvale, CA). Serum from influenza-hyperimmune mice was used to generate a standard curve. One antibody unit was arbitrarily designated as the absorbance generated from a 1/30,000 dilution of the influenza hyperimmune serum. Antibody units of individual mouse sera were calculated based on the standard curve.
References
Pollok, K.E. et al. Inducible T cell antigen 4-1BB. Analysis of expression and function. J. Immunol. 150, 771–781 (1993).
Pollok, K.E., Kim, S.H. & Kwon, B.S. Regulation of 4-1BB expression by cell-cell interactions and the cytokines, interleukin-2 and interleukin-4. Eur. J. Immunol. 25, 488–494 (1995).
Melero, I., Johnston, J.V., Shufford, W.W., Mittler, R.S. & Chen, L. NK1.1 cells express 4-1BB (CDw137) costimulatory molecule and are required for tumor immunity elicited by anti-4-1BB monoclonal antibodies. Cell. Immunol. 190, 167–172 (1998).
DeBenedette, M.A. et al. Role of 4-1BB ligand in costimulation of T lymphocyte growth and its upregulation on M12 B lymphomas by cAMP. J. Exp. Med. 181, 985–992 (1995).
Hurtado, J.C., Kim, Y.J. & Kwon, B.S. Signals through 4-1BB are costimulatory to previously activated splenic T cells and inhibit activation-induced cell death. J. Immunol. 158, 2600–2609 (1997).
Pollok, K.E. et al. 4-1BB T-cell antigen binds to mature B cells and macrophages, and costimulates anti-μ-primed splenic B cells. Eur. J. Immunol. 24, 367–374 (1994).
Hurtado, J.C., Kim, S.H., Pollok, K.E., Lee, Z.H. & Kwon, B.S. Potential role of 4-1BB in T cell activation. Comparison with the costimulatory molecule CD28. J. Immunol. 155, 3360–3367 (1995).
Goodwin, R.G. et al. Molecular cloning of a ligand for the inducible T cell gene 4-1BB: a member of an emerging family of cytokines with homology to tumor necrosis factor. Eur. J. Immunol. 23, 2631–2641 (1993).
Takahashi, C., Mittler, R.S. & Vella, A.T. Cutting edge: 4-1BB is a bona fide CD8 T cell survival signal. J. Immunol. 162, 5037–5040 (1999).
Kim, Y.J., Kim, S.H., Mantel, P. & Kwon, B.S. Human 4-1BB regulates CD28 co-stimulation to promote Th1 cell responses. Eur. J. Immunol. 28, 881–890 (1998).
Shuford, W.W. et al. 4-1BB costimulatory signals preferentially induce CD8+ T cell proliferation and lead to the amplification in vivo of cytotoxic T cell responses. J. Exp. Med. 186, 47–55 (1997).
Tan, J.T., Whitmire, J.K., Ahmed, R., Pearson, T.C. & Larsen, C.P. 4-1BB ligand, a member of the TNF family, is important for the generation of antiviral CD8 T cell responses. J. Immunol. 163, 4859–4868 (1999).
Saoulli, K. et al. CD28-independent, TRAF2-dependent costimulation of resting T cells by 4-1BB ligand. J. Exp. Med. 187, 1849–1862 (1998).
DeBenedette, M.A., Shahinian, A., Mak, T.W. & Watts, T.H. Costimulation of CD28− T lymphocytes by 4-1BB ligand. J. Immunol. 158, 551–559 (1997).
DeBenedette, M.A. et al. Analysis of 4-1BB ligand (4-1BBL)-deficient mice and of mice lacking both 4-1BBL and CD28 reveals a role for 4-1BBL in skin allograft rejection and in the cytotoxic T cell response to influenza virus. J. Immunol. 163, 4833–4841 (1999).
Melero, I. et al. Monoclonal antibodies against the 4-1BB T-cell activation molecule eradicate established tumors. Nature Med. 3, 682–685 (1997).
Tan, J.T. et al. 4-1BB costimulation is required for protective anti-viral immunity after peptide vaccination. J. Immunol. 164, 2320–2325 (2000).
Baumgarth, N., Egerton, M. & Kelso, A. Activated T cells from draining lymph nodes and an effector site differ in their responses to TCR stimulation. J. Immunol. 159, 1182–1191 (1997).
Doyle, A.G., Buttigieg, K., Groves, P., Johnson, B.J. & Kelso, A. The activated type 1-polarized CD8+ T cell population isolated from an effector site contains cells with flexible cytokine profiles. J. Exp. Med. 190, 1081–1092 (1999).
Murali-Krishna, K. et al. Counting antigen-specific CD8 T cells: a reevaluation of bystander activation during viral infection. Immunity 8, 177–187 (1998).
Vitiello, A. et al. Immunodominance analysis of CTL responses to influenza PR8 virus reveals two new dominant and subdominant Kb-restricted epitopes. J. Immunol. 157, 5555–5562 (1996).
Belz, G.T., Xie, W., Altman, J.D. & Doherty, P.C. A previously unrecognized H-2D(b)-restricted peptide prominent in the primary influenza A virus-specific CD8+ T-cell response is much less apparent following secondary challenge. J. Virol. 74, 3486–3493 (2000).
Hong, H.J. et al. A humanized anti–4-1BB monoclonal antibody suppresses antigen-induced humoral immune response in nonhuman primates. J. Immunother. 23, 613–621 (2000).
Mittler, R.S., Bailey, T.S., Klussman, K., Trailsmith, M.D. & Hoffmann, M.K. Anti-4-1BB monoclonal antibodies abrogate T cell-dependent humoral immune responses in vivo through the induction of helper T cell anergy. J. Exp. Med. 190, 1535–1540 (1999).
Lumsden, J.M., Roberts, J.M., Harris, N.L., Peach, R.J. & Ronchese, F. Differential requirement for CD80 and CD80/CD86-dependent costimulation in the lung immune response to an influenza virus infection. J. Immunol. 164, 79–85 (2000).
Moskophidis, D. & Kioussis, D. Contribution of virus-specific CD8+ cytotoxic T cells to virus clearance or pathologic manifestations of influenza virus infection in a T cell receptor transgenic mouse model. J. Exp. Med. 188, 223–232 (1998).
Hou, S., Hyland, L., Ryan, K.W., Portner, A. & Doherty, P.C. Virus-specific CD8+ T-cell memory determined by clonal burst size. Nature 369, 652–654 (1994).
Daly, K., Nguyen, P., Woodland, D.L. & Blackman, M.A. Immunodominance of major histocompatibility complex class I-restricted influenza virus epitopes can be influenced by the T-cell receptor repertoire. J. Virol. 69, 7416–7422 (1995).
Yewdell, J.W. & Bennink, J.R. Immunodominance in major histocompatibility complex class I-restricted T lymphocyte responses. Annu. Rev. Immunol. 17, 51–88 (1999).
Johnston, J.V. et al. B7-CD28 costimulation unveils the hierarchy of tumor epitopes recognized by major histocompatibility complex class I-restricted CD8+ cytolytic T lymphocytes. J. Exp. Med. 183, 791–800 (1996).
Oukka, M. et al. Protection against lethal viral infection by vaccination with nonimmunodominant peptides. J. Immunol. 157, 3039–3045 (1996).
Pardigon, N. et al. Role of co-stimulation in CD8+ T cell activation. Int. Immunol. 10, 619–630 (1998).
Murtaza, A., Kuchroo, V.K. & Freeman, G.J. Changes in the strength of co-stimulation through the B7/CD28 pathway alter functional T cell responses to altered peptide ligands. Int. Immunol. 11, 407–416 (1999).
Zhang, J. et al. p38 mitogen-activated protein kinase mediates signal integration of TCR/CD28 costimulation in primary murine T cells. J. Immunol. 162, 3819–3829 (1999).
Cannons, J.L., Choi, Y. & Watts, T.H. Role of TNF receptor-associated factor 2 and p38 mitogen-activated protein kinase activation during 4-1BB-dependent immune response. J. Immunol. 165, 6193–6204 (2000).
Cooper, D., Bansal-Pakala, P. & Croft, M. 4-1BB (CD137) controls the clonal expansion and survival of CD8 T cells in vivo but does not contribute to the development of cytotoxicity. Eur. J. Immunol. 32, 521–529 (2002).
Matloubian, M., Concepcion, R.J. & Ahmed, R. CD4+ T cells are required to sustain CD8+ cytotoxic T-cell responses during chronic viral infection. J. Virol. 68, 8056–8063 (1994).
Battegay, M. et al. Enhanced establishment of a virus carrier state in adult CD4+ T-cell- deficient mice. J. Virol. 68, 4700–4704 (1994).
Rahemtulla, A. et al. Normal development and function of CD8+ cells but markedly decreased helper cell activity in mice lacking CD4. Nature 353, 180–184 (1991).
Cerwenka, A., Morgan, T.M., Harmsen, A.G. & Dutton, R.W. Migration kinetics and final destination of type 1 and type 2 CD8 effector cells predict protection against pulmonary virus infection. J. Exp. Med. 189, 423–434 (1999).
Graham, M.B. et al. Response to influenza infection in mice with a targeted disruption in the interferon γ gene. J. Exp. Med. 178, 1725–1732 (1993).
Zhu, G. et al. Progressive depletion of peripheral B lymphocytes in 4-1BB (CD137) ligand/I-Eα)-transgenic mice. J. Immunol. 167, 2671–2676 (2001).
Ebata, T. et al. Rapid induction of CD95 ligand and CD4+ T cell-mediated apoptosis by CD137 (4-1BB) costimulation. Eur. J. Immunol. 31, 1410–1416 (2001).
Altman, J.D. et al. Phenotypic analysis of antigen-specific T lymphocytes. Science 274, 94–96 (1996).
Acknowledgements
We thank J. L. Po for helpful suggestions. Supported in part by NIH grant AI46719 (to P. D. K.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Halstead, E., Mueller, Y., Altman, J. et al. In vivo stimulation of CD137 broadens primary antiviral CD8+ T cell responses. Nat Immunol 3, 536–541 (2002). https://doi.org/10.1038/ni798
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ni798
This article is cited by
-
CD137 costimulation enhances the antiviral activity of Vγ9Vδ2-T cells against influenza virus
Signal Transduction and Targeted Therapy (2020)
-
Amelioration of Japanese encephalitis by blockage of 4-1BB signaling is coupled to divergent enhancement of type I/II IFN responses and Ly-6Chi monocyte differentiation
Journal of Neuroinflammation (2015)