Abstract
Adolescent growth and social development shape the early development of offspring from preconception through to the post-partum period through distinct processes in males and females. At a time of great change in the forces shaping adolescence, including the timing of parenthood, investments in today’s adolescents, the largest cohort in human history, will yield great dividends for future generations.
Similar content being viewed by others
Main
Global megatrends are reshaping health and human development almost everywhere1,2. Rapid economic, technological, social and demographic changes have brought reductions in infectious diseases, infant and maternal mortality and refocused attention on the non-communicable diseases of later life3. These forces are also reshaping health and development across the second and third decades. In preindustrial societies, the time between the end of childhood, which is signalled in girls by the late pubertal event of menarche (onset of menstruation) and spermarche (first ejaculation) or breaking of the voice in boys, and transition to adulthood, typically marked by parenthood, was generally around two years in girls and four in boys4,5. Improved nutrition and fewer infectious diseases in childhood, have been accompanied by a fall of around four years in the age at puberty to between 12 and 13 years6, a fall that has been rapid in current middle- and lower-income countries7,8. Over the same period, an even bigger upward shift has occurred in the timing of parenthood, the result of extended education, changing social norms around marriage and parenthood, and the availability of effective contraception.
Puberty initiates a phase of growth and maturation of the reproductive, musculoskeletal, neurodevelopmental, endocrine, metabolic, immune and cardio-metabolic systems, that extends into the third decade9,10. For this reason, adolescence can be considered a sensitive phase, during which the quality of the physical, nutritional and social environments may change trajectories of health and development into later life11. Given the concept that growth continues into the twenties, together with the delays in adopting adult roles, the idea has been proposed that adolescence might best be considered as ranging from 10 to 24 years12. From this perspective, adolescence occupies a greater proportion of the life course with greater relevance for human development than ever before9. An extended adolescence creates an opportunity for this generation to acquire greater assets and capabilities. Equally, adolescence has been accompanied by shifts in the social milieu of development, with the emergence of distinct youth cultures, greater media and peer engagement, and marketing to future consumers, in turn shifting patterns of health and health risk13. For example, the risk of sexually transmitted infections increases with multiple sexual partners before marriage; earlier initiation of substance use is associated with greater risk of later substance-use disorders; and a reduction in physical activity, alongside changes in diet, is associated with higher rates of obesity11,14.
In contrast to the recognition of the significance of adolescence for later adult health, its relevance for the next generation has received less attention15. This is surprising, given that adolescents are the next generation to become a parent and we have known for decades that preconception maternal nutrition (for example, folate deficiency)16 and infectious diseases17,18 affect the early life health and development of offspring. Indeed, a failure to consider influences on growth during early life that emerge in adolescence before conception may explain why antenatal interventions have too often only led to small gains10,19.
Here we explore the range of adolescent processes—molecular, physiological, behavioural and sociocultural—that may affect the early growth, health and development of the next generation19,20,21 (Fig. 1). Firstly, we consider time trends in the age of first parenthood and overall fertility across different country groups classified by level of economic development. Secondly, we explore the range of potentially modifiable processes that start during adolescence that may affect the early growth of offspring. Finally, we consider the shifting social determinants of health to illustrate the benefits for the next generation by investing in adolescents as the parents of tomorrow.
Puberty marks a transition to adolescence and a life phase during which girls and boys acquire resources that are essential for becoming parents of the next generation. It also marks the beginning of reproductive life with a transition to functional gamete production. The preconceptional phase (that is, adolescence) varies markedly in length carrying implications for the acquisition of the social, financial and educational assets and nutritional, health and interpersonal risks that underlie intergenerational processes. The three months before conception is a time of male and female gamete maturation when parental exposures, including nutrition, obesity, substance use, stress, endocrine disruptors and physical activity may influence gamete structure and function. Periconception includes fertilization of the maternal and paternal gametes as well as the zygote and embryonic phases that are sensitive to the maternal nutritional and hormonal environment. There continue to be direct maternal effects antenatally mediated through the in utero environment and postnatally through nutrition (for example, breastfeeding) and the maternal–infant relationship. Direct paternal influences grow in the postnatal phase through the paternal–infant relationship and potentially through risk exposures, such as paternal tobacco use. Maternal and paternal health, behaviour as well as social and economic circumstances continue to have an indirect effect on offspring development in both antenatal and postnatal phases.
The changing age of parenthood
Lower rates of giving birth during adolescence have led to a later transition to parenthood in most places. In all country income groups, birth rates in 15–19-year-old girls continue to fall with the most marked shifts in today’s lower middle-income countries where rates in 2030 are anticipated to be a third of those in 1970 (Extended Data Fig. 1a). Marked falls are also taking place across all country groups for young women aged 20–24, with 2030 birth rates in today’s high-income countries also predicted to be a third of the rates in 1970. As a result, adolescent parenthood is increasingly concentrated in specific geographic regions (South Asia, Latin-America and sub-Saharan Africa) and disadvantaged groups within countries22.
Decreases in birth rates during adolescence have led to parallel shifts in the duration of both adolescence and the preconception phase of reproductive life, defined as the time from reproductive maturity to first parenthood (Extended Data Fig. 1b). In high-income countries, only a quarter of girls now have a child by 25 years of age. As a result the gap between reproductive maturity, marked by menarche (on average between 12 and 13 years), and first parenthood is generally over a decade and often extends up to two. By contrast, over 80% of girls growing up in low-income countries become a parent by the age of 25, and 30% by the age of 18 years (Table 1). These differences have major implications for the acquisition of both assets and risks during the preconception window (Fig. 1).
Data on the timing of parenthood for males are scarcer and generally of poorer quality. France and Norway are among the few countries with data23. French men typically have children at around the age of 33 years, three years later than women. Males are also coming to parenthood later in life; 40% of Norwegian men born in the 1950s had become a parent by the age of 25 compared to less than 20% for those born in the 1970s, and just over 10% of those born in the 1990s. Therefore, the gap between reproductive maturity and parenthood has also lengthened for boys, a result of effective contraception, extended education, higher costs to establish a family and changing social norms around family formation24.
Early parenthood and its consequences
A longer adolescence leads to healthier growth, particularly for girls without the competing nutritional demands of early pregnancy, and greater opportunities for education and entry into the workforce25. For these reasons, age at first birth is a powerful determinant of long-term parental economic capacity, including income and housing26. Conversely adolescent parenthood predicts both poor maternal and infant health. In over 120,000 pregnancies in girls aged 10–24 in the Multicountry Survey of Maternal and Child Health of the World Health Organization (WHO), those giving birth before 15 years of age were at higher risk of eclampsia and puerperal infection27. Their babies had higher rates of low birth weight, preterm delivery and severe neonatal conditions27. Similarly, in pooled analyses of 19,403 offspring from birth cohorts in Brazil, Guatemala, India, the Philippines and South Africa, giving birth before the age of 19 predicted low birth weight, preterm birth and stunting of offspring and these associations were strongest in the youngest mothers28.
Nutritional needs increase markedly with rapid pubertal growth, making younger adolescents and their offspring vulnerable to undernutrition29. Studies of adolescents exposed to famine provide compelling evidence of the persisting effects on adult height of severe undernutrition during adolescence30. Equally, follow-up of the offspring of parents exposed to the Chinese (1959–1961) and Cambodian (1975–1979) famines suggest intergenerational risks, with rates of stunting greatest in those whose parents were exposed during adolescence31,32. Gestational undernutrition is particularly prominent in adolescence with maternal–fetal competition for energy and nutrients that remain essential for a girl’s own continued growth33. It is associated with increased risk of neonatal mortality, preterm birth, small for gestational age babies, and low birth weight34. The effects extend to the postnatal period with compromised antenatal breast development reducing breast milk quality and quantity35 and the establishment of attachment bonds36,37.
Iron and other micronutrient requirements increase sharply at puberty, particularly for girls with the onset of menstruation, so that in younger adolescents anaemia is the leading cause of global disease burden14. Adolescent anaemia is commonly a result of iron and other micronutrient deficiencies and is therefore a useful indicator of nutritional status38,39. Figure 2a and Extended Data Figure 2 show rates of anaemia across the years of transition to first parenthood. Since 1990, rates of anaemia in low- and lower middle-income countries have fallen but only modestly. Consistent with rapid growth and the onset of menstruation, anaemia rates rise for young women from adolescence into the early twenties and then stabilize through the remaining reproductive years. It indicates that nutritional deficiencies remain common in young women in the transition to parenthood and policies to date have failed to address these major, modifiable determinants of early growth in the next generation.
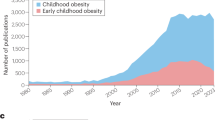
a, b, Prevalence of anaemia in females (a) and males (b). Prevalence of obesity in females (c) and males (d).
In high-income countries, maternal and offspring outcomes are also poorer in those giving birth before 15 years of age with greater infant death, stillbirth, intrauterine growth restriction and preterm birth40. Teenage childbearing is often unplanned, and is associated with partnership instability, a greater likelihood of single parenthood, greater poverty and less parental education contributing to poorer child outcomes41,42. Even small delays of 6–18 months in the transition to motherhood independently predict offspring test scores for reading and mathematics that are in turn predictive of educational attainment and eventual earnings43.
Antenatal actions to promote maternal and fetal health generally occur after pregnancy recognition or a first antenatal visit. In high-income countries, such as the United States, women are generally unaware of pregnancy until six weeks of gestation or longer if the pregnancy was unintended44. Initiation of antenatal care is typically around three weeks later45. In resource poor settings, pregnancy confirmation and a first antenatal visit are generally much later. Less than half of pregnant women in sub-Saharan Africa have an antenatal visit in the first trimester, and rates are lower in adolescents46. Although undernutrition has been a major policy focus in maternal health47, antenatal interventions with maternal protein-energy or micronutrient supplements have generally brought minimal changes to birth weight10. One probable reason is that interventions are taking place too late in pregnancy48.
Intergenerational risk processes
A range of parental adaptations have the potential to influence the growth and development of the next generation. These biological, interpersonal and social processes are outlined in the following sections.
Mechanisms involving parental gametes
A possibility that the male germline captures information from a changing environment to pass on to subsequent generations has generated attention more recently49. It challenges an assumption that the sole function of gametes is to deliver half each of the maternal and paternal genomes to a common zygote. It was believed that this process did not include the transfer of environmental information. However, alternative theories, starting with Lamarck, and including Darwin in his theory of pangenesis, have suggested that some adaptations may be transmitted to the next generation. Recent studies have begun to describe these processes, revealing an interplay between environmental exposures and the parental reproductive milieu (Fig. 1). Potential mechanisms involve not only the protein and RNA cargo contained within gametes, but also factors, which are external to gametes, that are capable of influencing fertilization and early embryonic development. Gamete DNA also has a distinct, and modifiable, epigenetic profile, that is sensitive to environmental exposures, with some changes that are maintained during embryonic development, thus carrying information from one generation to the next50.
For both males and females, puberty initiates functional gamete production, a process that continues throughout adult reproductive life. There are likely to be sex differences in the timing and duration of sensitive exposure windows, given differences in gamete maturation. Gametogenesis begins early in utero with the specification of primordial germ cells. In males, this process is halted before meiosis, but in females, the process proceeds to the first meiotic division, where it then arrests until puberty. Thus, all primary oocytes produced throughout a female’s lifetime exist before birth, or shortly thereafter. By contrast, the process of spermatogenesis commences at puberty. Sperm maturation takes between 70 and 100 days in humans, predominantly in the seminiferous tubules that are in constant contact with supporting Sertoli cells. This is followed by a 1–2 week transitional period in the epididymis, during which time proteins and a small amount of RNA are selectively shuttled into the developing sperm51,52.
The paternal preconception environment modulates the RNA content of the developing sperm, with possible effects on post-fertilization development and offspring phenotypes53. In animal studies, paternal exposures to high-fat and high-sugar diets produce metabolic disturbances in offspring54, and both stress and exercise affect stress responses of the offspring55,56,57. Animal and some human studies have found effects of preconceptional tobacco, alcohol and illicit drug use on gamete epigenomes, with diverse effects on offspring development58,59. Although there are fewer human studies, alcohol consumption of more than two standard drinks per day is linked to morphological changes in sperm60. One report of a very large study has found effects of heavy (more than five standard drinks per day) paternal but not maternal preconception drinking on offspring head circumference and risk of microcephaly61. Paternal obesity generates risks of metabolic disturbance and obesity in offspring through the gamete epigenome, but diet and exercise appear to modify these risks62,63. In humans, bariatric surgery reverses obesity-induced epigenetic changes in spermatozoa64. Whether these paternal processes are ‘anticipatory adaptive responses’ to a likely postnatal environment or have other functions is currently under debate65,66,67.
Maternal gametes (oocytes) also have a unique epigenetic profile, as well as a cargo of RNA species and proteins that are mostly acquired over the four months of maturation before ovulation68. Both animal and human studies have shown that the preconception environment may alter oocyte maturation69 with maternal obesity affecting the metabolism of the developing ova and early offspring growth70,71. Because mitochondrial DNA is only passed on through the maternal line, oocyte mitochondrial DNA may provide a further sex-specific intergenerational mechanism. In a mouse study, a high-fat and high-sugar diet beginning before conception altered insulin signalling in the skeletal muscle of the offspring due to mitochondrial dysfunction, an effect that passed through the maternal germ line to the third generation72.
Periconceptional mechanisms
The time between fertilization and embryo implantation into the uterine decidua is marked by the emergence of distinct cell lineages, beginning with the specification of embryonic and extra-embryonic cells. There is extensive remodelling of parental gametic epigenetic profiles, a process that differs depending on the parent of origin. This re-organization initiates a shift from two distinct gametic epigenomes to a single embryonic epigenome with a capacity to form any cell type (see Fig. 1). This embryonic phase consists of two major epigenetic remodelling events: the first occurs immediately after fertilization; and the second induces the reestablishment of totipotency in primordial germ cells. These cells are the precursors of all offspring gametes, which is one of the reasons why periconceptional processes have implications for more than one generation73.
The epigenomic reorganization of early embryogenesis is sensitive to the maternal environment, with effects of protein-energy and micronutrient deficiencies as well as over-nutrition74,75. Observational studies, such as the Dutch Hunger Winter study, have implicated periconception as a sensitive time for epigenetic programming76. Of note are studies of metastable epialleles, epigenetically labile regions of the genome that are subject to large changes in response to environmental influences during very early embryogenesis. These regions were first described in mice, but subsequent human studies in Gambia have demonstrated epigenetic variation at metastable epialleles that are linked to periconceptional maternal nutrition77, findings that have later been replicated in a rural Bangladeshi cohort78. The methylation status of metastable epialleles has been linked to later obesity and metabolic function79.
Implantation is associated with further sensitivity to environmental influence. It initiates a functional interaction between the blastocyst (early embryo) and endometrium. The uterine microenvironment allows embryo–maternal crosstalk both pre- and post-implantation. Extracellular vesicles produced by the endometrium have been shown to be mediators of maternal–embryo communication through their protein and RNA cargoes80. Secreted proteins from both the embryo (for example, human chorionic gonadotrophin from the trophectoderm) and endometrium (for example, cytokines) guide successful implantation81. These processes are sensitive to maternal hormonal status and environmental influences, including stress and nutrition82.
Persistence of adolescent assets and risks
Assets derived from education, financial resources, family, social and cultural capital that are acquired during adolescence are essential for effective parenting and ultimately the growth and development of the next generation83 (see Fig. 1). Similarly, risks related to undernutrition, obesity, substance abuse and mental disorders become prominent following puberty and tend to persist through the transition to parenthood even when this occurs decades later84.
Stress and mental disorders
Around one in four mothers experience symptoms of depression and anxiety in the perinatal period85. In contrast to earlier views that perinatal depression is a discrete disorder limited to the post-partum period, perinatal maternal depression more commonly seems to be a continuation of pre-pregnancy mental health problems into pregnancy and the post-partum period. A recent Australian study found that 86% of mothers with high perinatal depressive symptoms had a similar history before conception, predominantly dating back to adolescence86. Antenatal and postnatal exposures independently affect child cognitive and emotional development85,87. In low-resource settings, the effects extend to childhood stunting and physical illness with antenatal depressive symptoms predicting higher rates of pre-term birth, failure to thrive in utero and low birth weight88,89. Animal studies of maternal antenatal stress have shown effects on various hormonal and chemical mediators (glucocorticoids, oxygen and glucose) that are associated with reduced fetal weight, gender-specific metabolic changes in the offspring and long-term adverse metabolic and renal effects90,91. Persistence of preconception mental health risks into the postpartum affects mother–infant bonding with a greater likelihood of maternal over-intrusiveness, emotional withdrawal and failure to sensitively engage92.
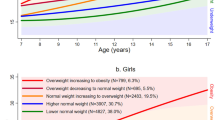
Given recent secular trends to earlier onset, adolescent mental disorders have become more important as an intergenerational risk process93. In high-income settings, over half of young women have an episode of a common mental disorder before becoming a parent94. Figure 3a and Extended Data Figure 3 show prevalence estimates for DSM (Diagnostic and Statistical Manual of Mental Disorders) depressive disorders (major depression and dysthymia) in females and males aged 10–35 years, drawn from the Global Burden of Disease (2016) study95. Rates increase through to the mid-twenties and then plateau so that in high-income countries, women typically become parents at a time of high risk.
a, Prevalence of major depression and dysthymia in females and males. b, Prevalence of daily tobacco use in females and males. c, Prevalence of alcohol-use disorders in females and males.
Substance use
Experimentation with tobacco, alcohol and other drugs typically begins in adolescence, with escalation to higher risk use and dependence in early adulthood96. Recent trends have generally been to earlier and heavier use with growing similarities in use in females and males97. Figure 3b, c and Extended Data Figures 4, 5 show patterns of daily smoking and alcohol-use disorders in females and males across the years of transition to parenthood. Daily smoking rates rise steeply during the period of adolescence and young adulthood for males in all country groupings. Rates of alcohol-use disorders are higher in males in all country strata, although in high-income countries, the gender gap is less. In high-income countries, the highest rates of substance use generally coincide with the peak in first parenthood for both sexes.
There is consistent and clear evidence that persisting maternal tobacco, alcohol, cannabis and other illicit drug use during pregnancy adversely affects growth and development of the offspring58. Maternal smoking has consistently been linked to adverse birth and child outcomes ranging from poor fetal growth, low birth weight, stillbirth, sudden unexpected death in infancy and a broad range of birth defects to later childhood behavioural problems, obesity and impaired lung function98,99. Heavier antenatal drinking (that is, more than three standard drinks per day) is also independently predictive of poor birth outcomes. What the risks of lower levels of consumption are remains debated100. Animal models indicate that alterations in fetal growth occur even with brief periconceptional alcohol exposure101 and even low levels of alcohol consumption during the first trimester affect craniofacial development in humans102.
Women commonly modify their substance use during later pregnancy with modest benefits for fetal growth and development103. Heavy and dependent users, more common in countries with delayed parenthood, are less likely to cease use during pregnancy104. However, given that around 40% of pregnancies are unintended and recognition typically occurs around 6–8 weeks of gestation, pre- and periconceptional exposure is likely to be very high in countries in which substance use in adolescents is common105,106.
Obesity and metabolic disruption
Figure 2b and Extended Data Figure 2 illustrate the rapid increase in obesity during adolescence and young adulthood in females across all country income strata and for males in high-income and upper middle-income countries. The increase with age reflects obesity’s strong tendency to persist once established107,108. Substantial increases in rates have occurred since 1990 across all country income groups. In high-income countries, prevalence rates of obesity for both females and males in the peak years for first parenthood are around one in five. Although rates are lower elsewhere, one in ten 25–29-year-old women in upper middle-income countries are obese.
Antenatal maternal obesity predicts macrosomic birth109, later childhood obesity and metabolic disturbance110,111, poorer cognitive skills and greater risk of behavioural problems during childhood112. Antenatal interventions to prevent these consequences appear to have limited benefits. Exercise has the potential to promote greater maternal insulin sensitivity, but its benefits during pregnancy are debated113,114. A recent Cochrane review failed to demonstrate that dietary and lifestyle (including exercise) interventions for women with gestational diabetes mellitus restored glycaemic control or prevented adverse effects for women or their babies113,115. Although two reports have suggested some modest benefits of antenatal exercise in obese women, its late timing in those with no regular pattern of physical activity before pregnancy seems likely to bring limited benefits116,117. By contrast, exercise and diet before pregnancy may bring greater offspring benefits. Exercise initiated before and continued during pregnancy in female rats at risk of gestational diabetes prevents the development of glucose intolerance (gestational diabetes) by increasing β-cell mass and function118. Given rapidly rising rates of obesity in nearly all countries, primary prevention that starts in late childhood and continues during adolescence will be essential to avoid wide-ranging adverse intergenerational effects. Sharp drops in physical activity across the second decade, with only around 20% of adolescents globally achieving recommended levels, suggest that promoting physical activity should be a priority119,120.
Adolescence and the next generation
Growth in the first thousand days predicts later-life health, human capability and resilience to adversity, which is why policies have focused on the promotion of optimal growth and human capital during the first thousand days. Increasingly it has also become a focus for the prevention of non-communicable diseases121. However, many of the processes that shape growth during early life originate well before conception or the first antenatal visit. Whether associated with early and high fertility, or with later and lower fertility, growth and development during adolescence provide a foundation for the start to life of the next generation.
The transition through education to employment typically occurs in adolescence, allowing the acquisition of assets that will be essential for being an effective parent, including financial resources and property, and extending to physical, cognitive, social and emotional capabilities (see Fig. 1). However, there are obstacles for many adolescents in achieving a secure foundation for parenthood. Early marriage is particularly noteworthy. Although rates are generally falling, more than half of girls continue to be married before the age of 18 years across many countries in sub-Saharan Africa122. Early marriage predicts early parenthood, overall fertility and poor maternal and child nutrition123,124,125. Its effects on the next generation are further mediated through curtailed education and exclusion of women from the formal workforce126. The annual benefits in 2030 from ending child marriage from reduced population growth and reductions in early childhood mortality and stunting have recently been estimated at US$664 billion126. For proven interventions targeting social norms to delay early marriage, we estimated their benefit–cost ratios to be 8.9 in terms of improving education in the next generation (see Box 1).
Adolescent investments for the next generation will differ in different places. The education of girls is essential in countries with high and early fertility, and early marriage127. The education of boys also appears to be important, in that males without education are more likely to marry girls before the legal age and educated fathers have daughters who marry later125. Figure 4 illustrates progress in secondary school completion across country income groups in 1990 and 2010. Over 20 years, rates of secondary school completion for girls and boys have increased in all income groups, although much less so in low-income countries, in which only a small minority of girls complete secondary education. Despite gains in lower middle-income countries, rates of secondary school completion for both boys and girls remain under 50%, underlining the importance of continuing investments throughout the Sustainable Development Goal period. Ultimately, success in promoting education will also depend on tackling adolescent undernutrition, social norms favouring early marriage, exposure to hazardous social and physical environments, and adolescents’ poor access to health services, including modern contraception.
a, b, Secondary school completion for females (a) and males (b) in 1990 and 2010.
In higher-income countries that have made a transition to low and late fertility, shifting the policy focus to health risks that emerge in adolescence and persist through to parenthood will be essential. Rates of adolescent mental disorders appear to be reaching historic highs and have a strong tendency to persist into the child-bearing years with consequences for maternal and child health, and family wellbeing. Similarly, adolescent and young adult alcohol use and other substance use continue to rise in many countries. Even more marked is the rise in obesity, particularly given that available antenatal interventions to reduce the metabolic consequences for both mothers and offspring are limited128.
Intergenerational epidemiological studies remain uncommon, and few have addressed risks during sensitive time periods129. However, it is becoming clear that different approaches to pregnancy and parenthood will be needed. Preparation for pregnancy and preconception care has been one recent focus48,75,130. Previously, the main preconception focus of health services has been on the prevention of unintended pregnancy through provision of contraception131. Nevertheless, in countries with high levels of primary care coverage, in which a majority of women make contact with health services at least annually, there would be scope to screen and intervene around intergenerational health risks132. The major barriers are the low current demand from future parents and a limited provision of more comprehensive healthcare, particularly for women at the greatest risk131. There is little doubt that a reorientation of service systems towards preconception would be of value133. However, given continuing high rates of unintended pregnancy134,135 and the difficulty of modifying chronic health risks, addressing obesity, mental disorders and substance dependence earlier in adolescence will be essential. It requires a broadening of adolescent health beyond a traditional emphasis on sexual and reproductive health, extending the engagement of health service systems with adolescents and creating health-promoting environments in the families, schools, workplaces and communities in which adolescents are growing up11. Given the extent to which adolescents shape their own social and nutritional environments, this will require an active engagement with adolescents themselves.
The rapid rise in obesity in middle-income countries, even where undernutrition and food insecurity persist, will require multicomponent approaches with elements addressing healthy diets, physical activity and sedentary behaviour, as well as creating the opportunities for adolescents and their families to make healthy choices136. Similarly, high rates of mental disorders are likely to require not only early clinical intervention, but also the targeting of risk factors and the acquisition of protective social and emotional skills. For poor and socially marginalized adolescents in higher-income countries, who often have high and early fertility, responses may need to be similar to those for adolescents growing up in low-income countries19. Creating health-promoting environments for adolescents will ultimately require engagement well beyond the health sector, with education, local government, industry, religious leaders, civil society and young people themselves all essential actors.
Girls and young women should undoubtedly remain a priority. However boys and young men should also be brought into focus. They have important roles in parenting that are affected by health problems that commonly emerge before conception137. Their values and behaviours affect the capacities of young women to become effective mothers138. Increasingly we also understand that their influence on the next generation extends to distinct biological processes that directly affect the early development of the next generation.
Relative to other ages, the current generation of 10–24-year-olds is the largest cohort seen139. The potential demographic dividend from a large healthy and educated adolescent cohort entering the workforce has already captured policy attention25. We have largely overlooked the fact that this will also be the largest generation to parent, promising an additional dividend in the health, growth and capabilities of the next generation43. In a world of competing policy priorities, there is no doubt that providing the resources for healthy adolescent growth, education and emotional development will yield large benefits for current and future generations.
Methods
The analysis of risks included the 195 countries represented in the Institute for Health Metrics and Evaluation (IHME) Global Health Data Exchange database. The IHME provide population data for each country by year, sex and age group. We grouped countries according to World Bank income groups on gross national income per capita in US dollars: high income, upper middle income, lower middle income, and low income145. Estimates of prevalence are included as the percentage of people affected (for example, daily smokers) within each World Bank stratum. Estimates were generated for males and females; for the age groups (years): 10–14, 15–19, 20–24, 25–29 and 30–34; for the years: 1990, 1995, 2000, 2005, 2010 and 2016. The modelling of the data, including simulation of uncertainty bounds, is described elsewhere146,147,148.
The secondary school completion data were sourced from the database of ref. 149. Data are available for 146 countries. Completion of secondary education was defined as the sum of adolescents who had completed high school together with those currently in tertiary education.
Data in Extended Data Fig. 1 derive from the United Nations Population Division (UNPD) beginning in 1970 and projecting through to 2030 for countries that are stratified by their World Bank income status in 2015. In Fig. 2b, the estimates for 2030 are based on the level of education achieved in 2015 by girls in the respective country strata.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Change history
02 May 2018
Please see accompanying Publisher correction (https://doi.org/10.1038/s41586-018-0069-3). In Fig. 4a of this Analysis, owing to an error during the production process, the year in the header of the right column was '2016' rather than '2010'. In addition, in the HTML version of the Analysis, Table 1 was formatted incorrectly. These errors have been corrected online.
References
Lamy, P. Now for the Long Term: The Report of the Oxford Martin Commission for Future Generations (Oxford Univ. Press, 2013)
Jamison, D. T. et al. Global health 2035: a world converging within a generation. Lancet 382, 1898–1955 (2013)
GBD 2015 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388, 1603–1658 (2016)
Schlegel, A & Barry, H. Adolescence: An Anthropological Enquiry (Free Press, 1991)
Gluckman, P. D. & Hanson, M. A. Evolution, development and timing of puberty. Trends Endocrinol. Metab. 17, 7–12 (2006)
Ljung, B.-O., Bergsten-Brucefors, A. & Lindgren, G. The secular trend in physical growth in Sweden. Ann. Hum. Biol. 1, 245–256 (1974)
Meng, X., Li, S., Duan, W., Sun, Y. & Jia, C. Secular trend of age at menarche in Chinese adolescents born from 1973 to 2004. Pediatrics 140, e20170085 (2017)
Kac, G ., Auxiliadora De Santa Cruz Coelho, M. & Velasquez-Melendez, G. Secular trend in age at menarche for women born between 1920 and 1979 in Rio de Janeiro, Brazil. Ann. Hum. Biol. 27, 423–428 (2000)
Patton, G. C. & Viner, R. Pubertal transitions in health. Lancet 369, 1130–1139 (2007)
Prentice, A. M. et al. Critical windows for nutritional interventions against stunting. Am. J. Clin. Nutr. 97, 911–918 (2013)
Patton, G. C. et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet 387, 2423–2478 (2016)
Sawyer, S. M., Azzopardi, P. S., Wickremarathne, D. & Patton, G. C. The age of adolescence. Lancet Child Adolesc. Health https://doi.org/10.1016/S2352-4642(18)30022-1 (2018)
Viner, R. M. et al. Adolescence and the social determinants of health. Lancet 379, 1641–1652 (2012)
Mokdad, A. H. et al. Global burden of diseases, injuries, and risk factors for young people’s health during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 387, 2383–2401 (2016)
Sheehan, P. et al. Building the foundations for sustainable development: a case for global investment in the capabilities of adolescents. Lancet 390, 1792–1806 (2017)
Pitkin, R. M. Folate and neural tube defects. Am. J. Clin. Nutr. 85, 285S–288S (2007)
Peckham, C. & Gibb, D. Mother-to-child transmission of the human immunodeficiency virus. N. Engl. J. Med. 333, 298–303 (1995)
Lee, M.-J., Hallmark, R. J., Frenkel, L. M. & Del Priore, G. Maternal syphilis and vertical perinatal transmission of human immunodeficiency virus type-1 infection. Int. J. Gynaecol. Obstet. 63, 247–252 (1998)
Aizer, A. & Currie, J. The intergenerational transmission of inequality: maternal disadvantage and health at birth. Science 344, 856–861 (2014)
Thompson, O. Genetic mechanisms in the intergenerational transmission of health. J. Health Econ. 35, 132–146 (2014)
Godfrey, K. M., Gluckman, P. D. & Hanson, M. A. Developmental origins of metabolic disease: life course and intergenerational perspectives. Trends Endocrinol. Metab. 21, 199–205 (2010)
Mollborn, S. Teenage mothers today: what we know and how it matters. Child Dev. Perspect. 11, 63–69 (2017)
Rostgaard, T. & Møberg, R. J. in Fatherhood in the Nordic Welfare states: Comparing Care Policies and Practice (eds Eydal, G. B . & Rostgaard, T. ) Ch. 2, 23–52 (Policy Press, 2014)
Tanturri, M. L. in Contemporary Issues in Family Studies (eds Abela, A . & Walker, J. ) 136–150 (John Wiley & Sons, 2013)
World Bank. World Development Report 2007: Development and the Next Generation (World Bank, 2007)
Hoffman, S. D. & Maynard, R. A. Kids having Kids: Economic Costs & Social Consequences of Teen Pregnancy (The Urban Insitute, 2008)
Ganchimeg, T. et al. Pregnancy and childbirth outcomes among adolescent mothers: a World Health Organization multicountry study. Br. J. Obstet. Gynaecol. 121, 40–48 (2014)
Fall, C. H. et al. Association between maternal age at childbirth and child and adult outcomes in the offspring: a prospective study in five low-income and middle-income countries (COHORTS collaboration). Lancet Glob. Health 3, e366–e377 (2015)
Das, J. K. et al. Nutrition in adolescents: physiology, metabolism, and nutritional needs. Ann. NY Acad. Sci. 1393, 21–33 (2017)
Akresh, R., Bhalotra, S., Leone, M. & Osili, U. O. War and stature: growing up during the Nigerian Civil War. Am. Econ. Rev. 102, 273–277 (2012)
Li, Q. & An, L. Intergenerational health consequences of the 1959–1961 Great Famine on children in rural China. Econ. Hum. Biol. 18, 27–40 (2015)
Holmqvist, G. & Pereira. A. Famines and stunting: Are adolescents the hardest hit? https://blogs.unicef.org/evidence-for-action/famines-and-stunting-are-adolescents-the-hardest-hit/ (Unicef, 2017)
King, J. C. The risk of maternal nutritional depletion and poor outcomes increases in early or closely spaced pregnancies. J. Nutr. 133, 1732S–1736S (2003)
Wu, L. et al. Paternal psychological stress reprograms hepatic gluconeogenesis in offspring. Cell Metab. 23, 735–743 (2016)
Black, R. E. et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371, 243–260 (2008)
O’Dowd, R., Kent, J. C., Moseley, J. M. & Wlodek, M. E. Effects of uteroplacental insufficiency and reducing litter size on maternal mammary function and postnatal offspring growth. Am. J. Physiol. Regul. Integr. Comp. Physiol. 294, R539–R548 (2008)
Tharner, A. et al. Breastfeeding and its relation to maternal sensitivity and infant attachment. J. Dev. Behav. Pediatr. 33, 396–404 (2012)
Bhalotra, S. & Rawlings, S. Gradients of the intergenerational transmission of health in developing countries. Rev. Econ. Stat. 95, 660–672 (2013)
Ahmed, F., Khan, M. R., Banu, C. P., Qazi, M. R. & Akhtaruzzaman, M. The coexistence of other micronutrient deficiencies in anaemic adolescent schoolgirls in rural Bangladesh. Eur. J. Clin. Nutr. 62, 365–372 (2008)
Malabarey, O. T., Balayla, J., Klam, S. L., Shrim, A. & Abenhaim, H. A. Pregnancies in young adolescent mothers: a population-based study on 37 million births. J. Pediatr. Adolesc. Gynecol. 25, 98–102 (2012)
Mortimer, J. T. Adolescent Mothers in Later Life. Frank F. Furstenberg, Jr., J. Brooks-Gunn, and S. Philip Morgan. Cambridge University Press, New York, 1987. xiv, 204 pp., illus. $27.95. Human Development in Cultural and Historical Contexts. Science 240, 1060–1061 (1988)
McLanahan, S., Tach, L. & Schneider, D. The causal effects of father absence. Annu. Rev. Sociol. 39, 399–427 (2013)
Miller, A. R. Motherhood delay and the human capital of the next generation. Am. Econ. Rev. 99, 154–158 (2008)
Branum, A. M. & Ahrens, K. A. Trends in timing of pregnancy awareness among US women. Matern. Child Health J. 21, 715–726 (2017)
Ayoola, A. B., Nettleman, M. D. & Stommel, M. Time from pregnancy recognition to prenatal care and associated newborn outcomes. J. Obstet. Gynecol. Neonatal Nurs. 39, 550–556 (2010)
Owolabi, O. O. et al. Comparing the use and content of antenatal care in adolescent and older first-time mothers in 13 countries of west Africa: a cross-sectional analysis of Demographic and Health Surveys. Lancet Child Adolesc. Health 1, 203–212 (2017)
Victora, C. G., de Onis, M., Hallal, P. C., Blössner, M. & Shrimpton, R. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics 125, e473–e480 (2010)
Hanson, M. A ., Godfrey, K ., Poston, L ., Bustreo, F. & Stephenson, J. The Health of the 51%: Women Annual Report of the Chief Medical Officer (2014) Preconception health https://www.gov.uk/government/publications/chief-medical-officer-annual-report-2014-womens-health (Department of Health and Social Care, 2015)
Soubry, A. Epigenetic inheritance and evolution: a paternal perspective on dietary influences. Prog. Biophys. Mol. Biol. 118, 79–85 (2015)
Lane, M., Robker, R. L. & Robertson, S. A. Parenting from before conception. Science 345, 756–760 (2014)
Dacheux, J. L. & Dacheux, F. New insights into epididymal function in relation to sperm maturation. Reproduction 147, R27–R42 (2013)
Johnson, G. D., Mackie, P., Jodar, M., Moskovtsev, S. & Krawetz, S. A. Chromatin and extracellular vesicle associated sperm RNAs. Nucleic Acids Res. 43, 6847–6859 (2015)
Eaton, S. A. et al. Roll over Weismann: extracellular vesicles in the transgenerational transmission of environmental effects. Epigenomics 7, 1165–1171 (2015)
Chen, Q. et al. Sperm tsRNAs contribute to intergenerational inheritance of an acquired metabolic disorder. Science 351, 397–400 (2016)
Rodgers, A. B., Morgan, C. P., Leu, N. A. & Bale, T. L. Transgenerational epigenetic programming via sperm microRNA recapitulates effects of paternal stress. Proc. Natl Acad. Sci. USA 112, 13699–13704 (2015)
Short, A. K. et al. Elevated paternal glucocorticoid exposure alters the small noncoding RNA profile in sperm and modifies anxiety and depressive phenotypes in the offspring. Transl. Psychiatry 6, e837 (2016)
Short, A. K. et al. Exercise alters mouse sperm small noncoding RNAs and induces a transgenerational modification of male offspring conditioned fear and anxiety. Transl. Psychiatry 7, e1114 (2017)
Vassoler, F. M., Byrnes, E. M. & Pierce, R. C. The impact of exposure to addictive drugs on future generations: physiological and behavioral effects. Neuropharmacology 76, 269–275 (2014)
Laubenthal, J. et al. Cigarette smoke-induced transgenerational alterations in genome stability in cord blood of human F1 offspring. FASEB J. 26, 3946–3956 (2012)
Lwow, F., Me˛dras´, M., Słowin´ska-Lisowska, M., Józ´ków, P. & Szmigiero, L. The effect of occasional alcohol drinking on semen quality and sperm morphology among young and healthy Polish men. J. Mens Health 13, e16–e24 (2017)
Zuccolo, L. et al. Pre-conception and prenatal alcohol exposure from mothers and fathers drinking and head circumference: results from the Norwegian Mother–Child Study (MoBa). Sci. Rep. 7, 39535 (2016)
Huypens, P. et al. Epigenetic germline inheritance of diet-induced obesity and insulin resistance. Nat. Genet. 48, 497–499 (2016)
McPherson, N. O., Owens, J. A., Fullston, T. & Lane, M. Preconception diet or exercise intervention in obese fathers normalizes sperm microRNA profile and metabolic syndrome in female offspring. Am. J. Physiol. Endocrinol. Metab. 308, E805–E821 (2015)
Donkin, I. et al. Obesity and bariatric surgery drive epigenetic variation of spermatozoa in humans. Cell Metab. 23, 369–378 (2016)
Hosken, D. J. & Hodgson, D. J. Why do sperm carry RNA? Relatedness, conflict, and control. Trends Ecol. Evol. 29, 451–455 (2014)
Holman, L. & Price, T. A. Even more functions of sperm RNA: a response to Hosken and Hodgson. Trends Ecol. Evol. 29, 648–649 (2014)
Gluckman, P. D., Hanson, M. A. & Spencer, H. G. Predictive adaptive responses and human evolution. Trends Ecol. Evol. 20, 527–533 (2005)
Clarke, H. J. & Vieux, K.-F. Epigenetic inheritance through the female germ-line: the known, the unknown, and the possible. Semin. Cell Dev. Biol. 43, 106–116 (2015)
Rando, O. J. & Simmons, R. A. I’m eating for two: parental dietary effects on offspring metabolism. Cell 161, 93–105 (2015)
Jungheim, E. S. et al. Diet-induced obesity model: abnormal oocytes and persistent growth abnormalities in the offspring. Endocrinology 151, 4039–4046 (2010)
Ashworth, C. J., Toma, L. M. & Hunter, M. G. Nutritional effects on oocyte and embryo development in mammals: implications for reproductive efficiency and environmental sustainability. Phil. Trans. R. Soc. B 364, 3351–3361 (2009)
Saben, J. L. et al. Excess maternal fructose consumption increases fetal loss and impairs endometrial decidualization in mice. Endocrinology 157, 956–968 (2016)
Stringer, J. M., Barrand, S. & Western, P. Fine-tuning evolution: germ-line epigenetics and inheritance. Reproduction 146, R37–R48 (2013)
Fleming, T. P. et al. Do little embryos make big decisions? How maternal dietary protein restriction can permanently change an embryo’s potential, affecting adult health. Reprod. Fertil. Dev. 27, 684–692 (2015)
Hanson, M. A. et al. The International Federation of Gynecology and Obstetrics (FIGO) recommendations on adolescent, preconception, and maternal nutrition: “Think Nutrition First”. Int J. Gynaecol. Obstet. 131, S213–S253 (2015)
Tobi, E. W. et al. DNA methylation signatures link prenatal famine exposure to growth and metabolism. Nat. Commun. 5, 5592 (2014)
Dominguez-Salas, P. et al. Maternal nutrition at conception modulates DNA methylation of human metastable epialleles. Nat. Commun. 5, 3746 (2014)
Finer, S. et al. Is famine exposure during developmental life in rural Bangladesh associated with a metabolic and epigenetic signature in young adulthood? A historical cohort study. BMJ Open 6, e011768 (2016)
Kühnen, P. et al. Interindividual variation in DNA methylation at a putative POMC metastable epiallele is associated with obesity. Cell Metab. 24, 502–509 (2016)
Ng, M . et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384, 766–781 (2014)
Salamonsen, L. A., Evans, J., Nguyen, H. P. & Edgell, T. A. The microenvironment of human implantation: determinant of reproductive success. Am. J. Reprod. Immunol. 75, 218–225 (2016)
Greening, D. W., Nguyen, H. P., Elgass, K., Simpson, R. J. & Salamonsen, L. A. Human endometrial exosomes contain hormone-specific cargo modulating trophoblast adhesive capacity: insights into endometrial–embryo interactions. Biol. Reprod. 94, 1–15 (2016)
Currie, J. & Moretti, E. Mother’s Education and the Intergenerational Transmission of human Capital: Evidence from College Openings and Longitudinal Data. Working Paper No. 9360 (National Bureau of Economic Research, 2002)
Roth, T. L., Lubin, F. D., Funk, A. J. & Sweatt, J. D. Lasting epigenetic influence of early-life adversity on the BDNF gene. Biol. Psychiatry 65, 760–769 (2009)
Stein, A. et al. Effects of perinatal mental disorders on the fetus and child. Lancet 384, 1800–1819 (2014)
Patton, G. C. et al. Prediction of perinatal depression from adolescence and before conception (VIHCS): 20-year prospective cohort study. Lancet 386, 875–883 (2015)
Pearson, R. M. et al. Maternal depression during pregnancy and the postnatal period: risks and possible mechanisms for offspring depression at age 18 years. JAMA Psychiatry 70, 1312–1319 (2013)
Parsons, C. E., Young, K. S., Rochat, T. J., Kringelbach, M. L. & Stein, A. Postnatal depression and its effects on child development: a review of evidence from low- and middle-income countries. Br. Med. Bull. 101, 57–79 (2012)
Surkan, P. J., Kennedy, C. E., Hurley, K. M. & Black, M. M. Maternal depression and early childhood growth in developing countries: systematic review and meta-analysis. Bull. World Health Organ. 89, 608–615 (2011)
Cheong, J. N. et al. Sex-specific metabolic outcomes in offspring of female rats born small or exposed to stress during pregnancy. Endocrinology 157, 4104–4120 (2016)
Gallo, L. A., Tran, M., Moritz, K. M., Jefferies, A. J. & Wlodek, M. E. Pregnancy in aged rats that were born small: cardiorenal and metabolic adaptations and second-generation fetal growth. FASEB J. 26, 4337–4347 (2012)
Murray, L., Hipwell, A., Hooper, R., Stein, A. & Cooper, P. The cognitive development of 5-year-old children of postnatally depressed mothers. J. Child Psychol. Psychiatry 37, 927–935 (1996)
Collishaw, S. Annual research review: secular trends in child and adolescent mental health. J. Child Psychol. Psychiatry 56, 370–393 (2015)
Patton, G. C. et al. The prognosis of common mental disorders in adolescents: a 14-year prospective cohort study. Lancet 383, 1404–1411 (2014)
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1211–1259 (2017)
Olsson, C. A. et al. Drinking patterns of adolescents who develop alcohol use disorders: results from the Victorian Adolescent Health Cohort Study. BMJ Open 6, e010455 (2016)
Michaud, P. A., Berchtold, A., Jeannin, A., Chossis, I. & Suris, J. C. Secular trends in legal and illegal substance use among 16 to 20 year old adolescents in Switzerland. Swiss Med. Wkly 136, 318–326 (2006)
Banderali, G. et al. Short and long term health effects of parental tobacco smoking during pregnancy and lactation: a descriptive review. J. Transl. Med. 13, 327 (2015)
Hackshaw, A., Rodeck, C. & Boniface, S. Maternal smoking in pregnancy and birth defects: a systematic review based on 173 687 malformed cases and 11.7 million controls. Hum. Reprod. Update 17, 589–604 (2011)
Patra, J. et al. Dose–response relationship between alcohol consumption before and during pregnancy and the risks of low birthweight, preterm birth and small for gestational age (SGA)—a systematic review and meta-analyses. Br. J. Obstet. Gynaecol. 118, 1411–1421 (2011)
Gårdebjer, E. M., Cuffe, J. S., Pantaleon, M., Wlodek, M. E. & Moritz, K. M. Periconceptional alcohol consumption causes fetal growth restriction and increases glycogen accumulation in the late gestation rat placenta. Placenta 35, 50–57 (2014)
Muggli, E. et al. Association between prenatal alcohol exposure and craniofacial shape of children at 12 months of age. JAMA Pediatr. 171, 771–780 (2017)
Lumley, J. et al. Interventions for promoting smoking cessation during pregnancy. Cochrane Database Syst. Rev. 3, CD001055 (2009)
Schneider, S., Huy, C., Schütz, J. & Diehl, K. Smoking cessation during pregnancy: a systematic literature review. Drug Alcohol Rev. 29, 81–90 (2010)
Singh, S., Sedgh, G. & Hussain, R. Unintended pregnancy: worldwide levels, trends, and outcomes. Stud. Fam. Plann. 41, 241–250 (2010)
Nykjaer, C. et al. Maternal alcohol intake prior to and during pregnancy and risk of adverse birth outcomes: evidence from a British cohort. J. Epidemiol. Community Health 68, 542–549 (2014)
Patton, G. C. et al. Overweight and obesity between adolescence and young adulthood: a 10-year prospective cohort study. J. Adolesc. Health 48, 275–280 (2011)
Venn, A. J. et al. Overweight and obesity from childhood to adulthood: a follow-up of participants in the 1985 Australian Schools Health and Fitness Survey. Med. J. Aust. 186, 458–460 (2007)
Strutz, K. L., Richardson, L. J. & Hussey, J. M. Preconception health trajectories and birth weight in a national prospective cohort. J. Adolesc. Health 51, 629–636 (2012)
Wahlqvist, M. L. et al. Early-life influences on obesity: from preconception to adolescence. Ann. NY Acad. Sci. 1347, 1–28 (2015)
Yu, Z. et al. Pre-pregnancy body mass index in relation to infant birth weight and offspring overweight/obesity: a systematic review and meta-analysis. PLoS ONE 8, e61627 (2013)
Van Lieshout, R. J., Taylor, V. H. & Boyle, M. H. Pre-pregnancy and pregnancy obesity and neurodevelopmental outcomes in offspring: a systematic review. Obes. Rev. 12, e548–e559 (2011)
Agha-Jaffar, R., Oliver, N., Johnston, D. & Robinson, S. Gestational diabetes mellitus: does an effective prevention strategy exist? Nat. Rev. Endocrinol. 12, 533–546 (2016)
Hopkins, S. A. & Cutfield, W. S. Exercise in pregnancy: weighing up the long-term impact on the next generation. Exerc. Sport Sci. Rev. 39, 120–127 (2011)
Bain, E. et al. Diet and exercise interventions for preventing gestational diabetes mellitus. Cochrane Database Syst. Rev. 4, CD010443 (2015)
Russo, L. M., Nobles, C., Ertel, K. A., Chasan-Taber, L. & Whitcomb, B. W. Physical activity interventions in pregnancy and risk of gestational diabetes mellitus: a systematic review and meta-analysis. Obstet. Gynecol. 125, 576–582 (2015)
Wang, C. et al. A randomized clinical trial of exercise during pregnancy to prevent gestational diabetes mellitus and improve pregnancy outcome in overweight and obese pregnant women. Am. J. Obstet. Gynecol. 216, 340–351 (2017)
Mahizir, D. et al. Exercise before and during pregnancy is more effective in preventing metabolic disease in females born small fed a high fat diet than exercise during pregnancy only. Clin. Endocrinol. 86, 28 (2017)
Olds, T. et al. How do school-day activity patterns differ with age and gender across adolescence? J. Adolesc. Health 44, 64–72 (2009)
Hallal, P. C. et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 380, 247–257 (2012)
Bundy, D. A. P . et al. Investment in child and adolescent health and development: key messages from Disease Control Priorities, 3rd Edition. Lancet https://doi.org/10.1016/S0140-6736(17)32417-0 (2017)
Koski, A., Clark, S. & Nandi, A. Has child marriage declined in sub-Saharan Africa? An analysis of trends in 31 countries. Popul. Dev. Rev. 43, 7–29 (2017)
Adebowale, S. A., Fagbamigbe, F. A., Okareh, T. O. & Lawal, G. O. Survival analysis of timing of first marriage among women of reproductive age in Nigeria: regional differences. Afr. J. Reprod. Health 16, 95–107 (2012)
Fagbamigbe, A. F. & Idemudia, E. S. Survival analysis and prognostic factors of timing of first childbirth among women in Nigeria. BMC Pregnancy Childbirth 16, 102 (2016)
Hossain, M. G., Mahumud, R. A. & Saw, A. Prevalence of child marriage among Bangladeshi women and trend of change over time. J. Biosoc. Sci. 48, 530–538 (2016)
Wodon, Q . et al. Economic Impacts of Child Marriage: Global Synthesis Report (World Bank, 2017)
Kalamar, A. M., Lee-Rife, S. & Hindin, M. J. Interventions to prevent child marriage among young people in low- and middle-income countries: a systematic review of the published and gray literature. J. Adolesc. Health 59, S16–S21 (2016)
Hanson, M. et al. Interventions to prevent maternal obesity before conception, during pregnancy, and post partum. Lancet Diabetes Endocrinol. 5, 65–76 (2017)
Rando, O. J. Intergenerational transfer of epigenetic information in sperm. Cold Spring Harb. Perspect. Med. 6, a022988 (2016)
Mason, E. et al. From evidence to action to deliver a healthy start for the next generation. Lancet 384, 455–467 (2014)
M’hamdi, H. I., van Voorst, S. F., Pinxten, W., Hilhorst, M. T. & Steegers, E. A. Barriers in the uptake and delivery of preconception care: exploring the views of care providers. Matern. Child Health J. 21, 21–28 (2017)
Shannon, G. D., Alberg, C., Nacul, L. & Pashayan, N. Preconception healthcare delivery at a population level: construction of public health models of preconception care. Matern. Child Health J. 18, 1512–1531 (2014)
van Voorst, S. F. et al. Effectiveness of general preconception care accompanied by a recruitment approach: protocol of a community-based cohort study (the Healthy Pregnancy 4 All study). BMJ Open 5, e006284 (2015)
Finer, L. B. & Zolna, M. R. Shifts in intended and unintended pregnancies in the United States, 2001–2008. Am. J. Public Health 104, S43–S48 (2014)
Sedgh, G., Singh, S. & Hussain, R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud. Fam. Plann. 45, 301–314 (2014)
Draper, C. E. et al. Application of Intervention Mapping to develop a community-based health promotion pre-pregnancy intervention for adolescent girls in rural South Africa: Project Ntshembo (Hope). BMC Public Health 14, S5 (2014)
Wilson, S. & Durbin, C. E. Effects of paternal depression on fathers’ parenting behaviors: a meta-analytic review. Clin. Psychol. Rev. 30, 167–180 (2010)
Abramsky, T. et al. What factors are associated with recent intimate partner violence? Findings from the WHO multi-country study on women’s health and domestic violence. BMC Public Health 11, 109 (2011)
Gupta, M. D. The Power of 1.8 Billion: Adolescents, Youth and the transformation of the future (United Nations Population Fund, 2014)
United Nations. World Population Prospects The 2017 Revision. Key Findings and Advance Tables. Report No. ESA/P/WP/248 (United Nations, 2017)
Günes¸, P. M. The role of maternal education in child health: evidence from a compulsory schooling law. Econ. Educ. Rev. 47, 1–16 (2015)
Delprato, M., Akyeampong, K. & Dunne, M. Intergenerational education effects of early marriage in sub-Saharan Africa. World Dev. 91, 173–192 (2017)
Pande, R., Kurz, K., Walia, S., MacQuarrie, K. & Jain, S. Improving the reproductive health of married and unmarried youth in India: evidence of effectiveness and costs from community-based interventions. Final Report of the Adolescent Reproductive Health Program in India. (ICRW, 2006)
Montenegro, C. E. & Patrinos, H. A. Comparable Estimates of Returns to Schooling around the World. Policy Research Working Paper WPS7020 (World Bank, 2014)
World Bank. How does the World Bank classify countries?https://datahelpdesk.worldbank.org/knowledgebase/articles/378834-how-does-the-world-bank-classify-countries (accessed 6 January 2018)
GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1260–1344 (2017)
GBD 2016 SDG Collaborators. Measuring progress and projecting attainment on the basis of past trends of the health-related Sustainable Development Goals in 188 countries: an analysis from the Global Burden of Disease Study 2016. Lancet 390, 1423–1459 (2017)
GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 377, 13–27 (2017)
Barro, R. J. & Lee, J. W. A new data set of educational attainment in the world, 1950–2010. J. Dev. Econ. 104, 184–198 (2013)
Acknowledgements
We thank B. Reid for his assistance with the design of Fig. 1. G.C.P., P.S.A. and N.R. are supported by NH and MRC research fellowships. We acknowledge the support of the Victorian Government’s Operational Infrastructure Support Program. The views expressed in this paper are those of the authors and do not necessarily reflect the views of the European Commission.
Author information
Authors and Affiliations
Contributions
G.C.P. conceptualized the paper in conjunction with other authors. G.C.P. compiled the first draft with written contributions from S.M.S., C.A.O., V.S., R.S., M.E.W. and E.S. G.C.P., P.S.A., V.S., M.S., B.R., K.F. and K.S. contributed to the presented analyses. C.J.L.M., A.H.M. and N.J.K. provided estimates from Global Burden of Disease Study 2016. All authors reviewed first and subsequent versions of the paper and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended Data Figure 1 Birth rates and age of transition to parenthood in females across World Bank income groups.
a, Trends in birth rates in 15–24 year olds for 1970–2030. b, Transition to parenthood in 2015 and 2030. *Projections to 2030 are based on educational attainment of girls in 2015.
Extended Data Figure 2 Prevalence of anaemia and obesity in 10–34-year-old females and males in 1990 and 2016 for the four World Bank Country groupings in 2016.
Data are mean prevalence (line) and 95% uncertainty bounds (shading). Data were obtained from the Global Health Data Exchange (Global Burden of Disease Study 2016; http://ghdx.healthdata.org/gbd-results-tool).
Extended Data Figure 3 Prevalence of depressive disorders in 10–34-year-old females and males in 2016 for the four World Bank Country groupings.
Data are mean prevalence (line) and 95% uncertainty bounds (shading). Data were obtained from the Global Health Data Exchange (Global Burden of Disease Study 2016; http://ghdx.healthdata.org/gbd-results-tool).
Extended Data Figure 4 Prevalence of daily smoking in 10–34-year-old females and males in 2016 for the four World Bank Country groupings.
Data are mean prevalence (line) and 95% uncertainty bounds (shading). Data were obtained from the Global Health Data Exchange (Global Burden of Disease Study 2016; http://ghdx.healthdata.org/gbd-results-tool).
Extended Data Figure 5 Prevalence of alcohol-use disorders in 10–34-year-old females and males in 2016 for the four World Bank Country groupings.
Data are mean prevalence (line) and 95% uncertainty bounds (shading). Data were obtained from the Global Health Data Exchange (Global Burden of Disease Study 2016; http://ghdx.healthdata.org/gbd-results-tool).
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International (CC BY 4.0) licence. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons licence, users will need to obtain permission from the licence holder to reproduce the material. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Patton, G., Olsson, C., Skirbekk, V. et al. Adolescence and the next generation. Nature 554, 458–466 (2018). https://doi.org/10.1038/nature25759
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nature25759
This article is cited by
-
Using group model building to frame the commercial determinants of dietary behaviour in adolescence – findings from online system mapping workshops with adolescents, policymakers and public health practitioners in the Southwest of England
BMC Public Health (2025)
-
Sexual and reproductive health information needs; an inquiry from the lens of in-school adolescents in Ebonyi State, Southeast Nigeria
BMC Public Health (2024)
-
The relationship between non-communicable disease risk and mental wellbeing in adolescence: a cross-sectional study utilising objective measures in Indonesia
BMC Public Health (2024)
-
How much do adverse childhood experiences contribute to adolescent anxiety and depression symptoms? Evidence from the longitudinal study of Australian children
BMC Psychiatry (2024)
-
Familial confounding of internalising symptoms and obesity in adolescents and young adults; a co-twin analysis
International Journal of Obesity (2024)