Abstract
Objective:
To investigate the association between thrombocytopenia and placental lesions.
Study Design:
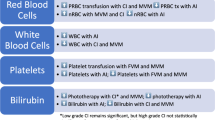
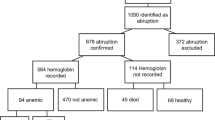
Cases included singleton infants admitted to the intensive care unit (2005 to 2010) with platelet counts <100 000 μl−1. We selected a contemporaneous control group matched for gestational age: 49 cases and 63 controls. The frequency of thrombosis in fetal vessels, fetal thrombotic vasculopathy, acute chorioamnionitis, chronic villitis, infarcts, hematomas, cord insertion and increased circulating nucleated red blood cells were identified on retrospective review of placental histology. Logistic regression models were used to test for associations.
Result:
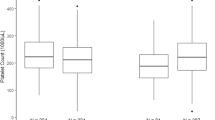
Placental lesions associated with poor maternal perfusion (odds ratio (OR) 3.36, 95% confidence interval (CI) 1.38, 8.15) or affecting fetal vasculature (OR 2.75, 95% CI 1.05, 7.23), but not inflammation, were associated with thrombocytopenia. A Pearson Chi-Square Test for Independence for fetal and maternal lesions indicated that the two are independent factors.
Conclusion:
Poor maternal perfusion and fetal vascular lesions are independently associated with thrombocytopenia in the newborn.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Christensen RD, Henry E, Wiedmeier SE, Stoddard RA, Sola-Visner MC, Lambert DK et al. Thrombocytopenia among extremely low birth weight neonates: data from a multihospital healthcare system. J Perinatol 2006; 26 (6): 348–353.
Ulusoy E, Tufekci O, Duman N, Kumral A, Irken G, Oren H . Thrombocytopenia in neonates: causes and outcomes. Ann Hematol 2013; 92 (7): 961–967.
Roberts I, Murray NA . Neonatal thrombocytopenia: causes and management. Arch Dis Child Fetal Neonatal Ed 2003; 88 (5): F359–F364.
Chakravorty S, Roberts I . How I manage neonatal thrombocytopenia. Br J Haematol 2012; 156 (2): 155–162.
Baer VL, Lambert DK, Henry E, Christensen RD . Severe thrombocytopenia in the NICU. Pediatrics 2009; 124 (6): e1095–e1100.
Venkatesh V, Curley A, Clarke P, Watts T, Stanworth S . Do we know when to treat neonatal thrombocytopaenia? Arch Dis Child Fetal Neonatal Ed 2013; 98 (5): F380–F382.
Salafia CM, Yampolsky M, Misra DP, Shlakhter O, Haas D, Eucker B et al. Placental surface shape, function, and effects of maternal and fetal vascular pathology. Placenta 2010; 31 (11): 958–962.
Murray NA, Roberts IA . Circulating megakaryocytes and their progenitors in early thrombocytopenia in preterm neonates. Pediatr Res 1996; 40 (1): 112–119.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Litt, J., Hecht, J. Placental pathology and neonatal thrombocytopenia: lesion type is associated with increased risk. J Perinatol 34, 914–916 (2014). https://doi.org/10.1038/jp.2014.117
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.117
This article is cited by
-
Association of placental histology and neonatal hematologic outcomes
Journal of Perinatology (2023)