Abstract
Aortic stiffness is strongly related to age and mean arterial pressure (MAP). In the present analysis, we investigated whether antihypertensive treatment modulates the association of the aortic pulse wave velocity (PWV) with age and with MAP in the general population. In the Czech post-MONICA cross-sectional study, we measured the PWV in 735 subjects (mean age 61.2±7.8 years, 54.1% women, 44.3% on antihypertensive medication). We used a linear regression model to assess the effect of treatment on the PWV. The independent covariates in our analysis included sex, age, MAP, heart rate, body mass index, plasma glucose, low-density lipoprotein cholesterol, smoking and observer. The patients receiving treatment were older (64.1±6.7 vs. 58.9±7.8 years), had higher systolic blood pressure (135.9±16.2 vs. 130.1±16.5 mm Hg) and had higher pulse wave velocity (9.1±2.2 vs. 8.2±2.1 m s−1; P for all <0.0001) than untreated subjects. After adjustment for MAP, the use of treatment modified the association between age and the PWV (regression equations, treated patients 9.68–0.009 × age vs. untreated subjects 6.98+0.020 × age, difference of regression slopes, F=11.2; P=0.0009). In analyses adjusted for age, treatment was associated with a smaller increase of the PWV with MAP (treated patients 9.63–0.006 × MAP vs. untreated subjects 7.18+0.010 × MAP, F=10.70; P=0.0001). These results were driven primarily by subjects whose blood pressure was below 140/90 mm Hg. In the cross-sectional analysis from a random sample of the general population, antihypertensive treatment was associated with a less steep increase in the PWV with age and the mean arterial pressure. Further longitudinal studies are needed to confirm this finding.
Similar content being viewed by others
Introduction
The aortic pulse wave velocity (PWV) is a surrogate measurement of aortic stiffness. Clinical interpretation of the aortic PWV is straightforward in that higher values are directly attributable to excessive aortic wall stiffness and are associated with an increasing risk for cardiovascular morbidity and mortality both in the general population1, 2 and in patients with several pathological conditions.3, 4 The 2007 European Guidelines for the Management of Hypertension5 listed aortic stiffness, measured through the carotid-femoral PWV, among the parameters that should be evaluated to assess target organ damage. Many studies have reported the beneficial effects of different antihypertensive drugs on arterial compliance.6, 7, 8 Whether the reduction in arterial stiffness after antihypertensive treatment is caused only by a reduction in blood pressure (BP) or also by additional effects independent of the BP is subject to debate.9 Few studies have reported data in favor of a BP-independent decrease in aortic stiffness.10, 11, 12, 13 The aim of the present study was to investigate whether antihypertensive treatment modifies the association of aortic stiffness with age and mean arterial pressure (MAP) in a random sample of the general population.
Methods
Study population
The Czech post-MONICA (MONItoring trends and determinants in CArdiovascular disease) study is a population survey studying trends and determinants of cardiovascular risk factors in a 1% random sample of the Czech population in nine districts of the country. The methods of the Czech post-MONICA study are described elsewhere.14 The present analysis included individuals examined in the city of Pilsen. The overall response rate in this district was 68.0%. Because the proportion of subjects using antihypertensive medication in the 25–45 year-old age group was small (5.1%), only subjects older than 45 years were included in the present analysis. The PWV measurement was available from 754 of the 930 participants. We excluded 19 subjects because biochemical variables were missing or the quality of the PWV measurement was insufficient. The total number of analyzed subjects was 735.
The research protocol included the administration of a standardized questionnaire to obtain information on each subject’s medical history, smoking and drinking habits, and medication use. Blood pressure was measured in triplicate in the right arm with the subject in the sitting position after at least 5 min at rest. Standard mercury sphygmomanometers and correctly sized cuffs were used. The participant’s right arm was supported at the heart level and the maximum inflation level was determined before the actual measurement. The blood pressure values were recorded to the nearest 2 mm Hg. The mean value of the last two readings was used for further analysis. The MAP derived from the office blood pressure measurement was calculated as the diastolic pressure plus one-third of the pulse pressure. Blood samples were obtained for biochemical analyses. Diabetes was defined as fasting plasma glucose ⩾7.0 mmol l−1 or the use of oral antidiabetic drugs and/or insulin. Height and body weight were determined for all of the participants, and body mass index was calculated as body weight/height2 (kg m−2).
Four observers obtained a PWV measurement using a SphygmoCor device (AtCor Medical, West Ryde, NSW, Australia). The PWV was computed from recordings of the arterial pressure wave at the carotid and femoral arteries.15 The distances between the site of the carotid recordings and the suprasternal notch, and between the suprasternal notch and the site of the femoral recordings were measured. The two values were subtracted to obtain the travel distance. The aortic PWV was calculated as the ratio of the travel distance in meters to the transit time in seconds. PWV was shown to have good reproducibility.15 Wilkinson et al.15 found that within-observer and between-observer variability amounted to 0.07±1.17 m s−1 and −0.30±1.25 m s−1, respectively.
Statistical methods
For the database management and statistical analyses, we used SAS software, version 9.2 (SAS Institute, Cary, NC, USA). The data are presented as the mean±s.d. or proportions. Student's t-test and the Fisher test were used to compare the differences between the untreated and treated subjects.
The effect of antihypertensive treatment on the PWV was evaluated using multivariate linear regressions. The differences between the slopes and intercepts of regression lines were tested using the F-test. The selection of covariates was based on known associations from the literature and from the significant univariate relationship. The basic model was adjusted for the observer and age or MAP. In the fully adjusted model, we added the following independent variables to the regression model: gender, body mass index, heart rate, plasma glucose, low-density lipoprotein cholesterol and smoking.
Results
Characteristics of participants
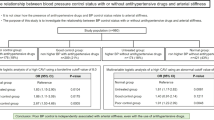
The general characteristics of the subjects are listed in Table 1. The proportions of women and men did not differ in the untreated and treated group. The subjects using antihypertensive drugs were older 64.1±6.7 vs. 58.9±7.8 years, had higher systolic blood pressure 135.9±16.2 vs. 130.1±16.5 mm Hg and were more obese than the untreated subjects (body mass index 29.7±4.6 vs. 27.2±4.6 kg m−2, P for all <0.0001). As expected, the aortic PWV was also higher in the treated patients compared with the untreated subjects (9.1±2.2 vs. 8.2±2.1 m s−1; P<0.0001). The proportions of diabetic patients (21.8% vs. 7.1%;) and the use of lipid-lowering medication (42.3% vs. 11.0%; P for both <0.0001) were higher in the treated group than in the untreated subjects. The prevalence of smokers was lower in the treated group than in the untreated subjects (18.7% vs. 30.8%; P=0.0002).
In the treated group, 40% of the patients were on monotherapy, 36% were taking a double-combination, 10% were taking a triple-combination and 14% were taking four or more antihypertensive drugs. Table 2 gives the numbers and proportions of the different classes of antihypertensive drugs. The most commonly used medications were drugs interfering with the renin–angiotensin system. Among the 326 treated patients, 184 (56.4%) had well-controlled BP. In the untreated group, 283 (69.2%) participants were normotensive.
Effect of antihypertensive treatment
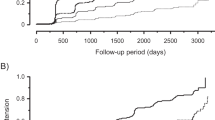
Figure 1 shows the relationships between age and PWV. In this model, as well as in fully adjusted regression models, the treated subjects had higher intercepts of the regression lines than the untreated subjects. In a model adjusted for the MAP, the PWV increase with age was smaller in the treated patients compared with the untreated subjects (P for difference of regression slopes =0.0009; Figure 1a). This finding was consistent with the fully adjusted model (P=0.019, Figure 1b). Similarly, the PWV increase with the MAP was significantly lesser in the treated patients than in the untreated subjects in the basically (P=0.0001; Figure 2a) and fully adjusted (P⩽0.0011; Figure 2b) analysis. Moreover, adjustment for age resulted in a slightly inverse relation between the PWV and MAP (Figures 2a and b).
Effect of antihypertensive treatment on aortic PWV in relation to age. Effects of antihypertensive treatment on PWV in relation to age. Panel a shows results of analysis after basic adjustments (for observer and MAP); panel b analysis adjusted for sex, MAP, heart rate, body mass index, plasma glucose, low-density lipoprotein cholesterol, smoking and observer. Gray squares indicate untreated subjects, black triangles indicate treated patients. The number of subjects, regression equations and 95% confidence limits for mean predicted values are given for each group. The differences of regression line slopes are given.
These associations between the PWV and age remained consistent in 467 subjects who had BP below 140/90 mm Hg (Figure 3a). On the other hand, in 268 subjects with BP above 140/90 mm Hg, no difference was found in the slopes of the regression lines between the treated and untreated subjects (Figure 3b).
Effect of antihypertensive treatment on PWV in relation to age in subjects with blood pressure <140/90 mm Hg and in those with blood pressure ⩾140/90 mm Hg. Effects of antihypertensive treatment on PWV in relation to age in subjects whose blood pressure was below 140/90 mm Hg (panel a) and in those with blood pressure ⩾140/90 mm Hg (panel b). The figures show results of analyses after basic adjustments for observer and MAP, respectively. The differences of intercepts (if appropriate) and regression line slopes are given. For further explanation, see Figure 1.
The above-mentioned findings remained consistent after exclusion of the outlying values from the analysis (data not shown).
Discussion
The key finding of our study is that the use of antihypertensive medication was associated with a less steep increase in aortic stiffness with age in the general population. This protective effect of BP-lowering drugs on aortic stiffness was driven by well-controlled subjects, for example, subjects whose BP was lower than 140/90 mm Hg. Another important finding was that the untreated subjects showed a steeper rise in the PWV with MAP compared with the treated patients.
The aim of the present analysis was to investigate whether the use of antihypertensive treatment modulates the association between aortic stiffness and age or MAP. To the best of our knowledge, no previous observational study has addressed this research question. Several reports have shown that antihypertensive treatment is associated with a reduction in aortic stiffness.6, 7, 16, 17 Ait-Oufella et al.16 showed that in routine clinical practice, treatment with antihypertensive drugs was associated with a large and sustained decrease in the carotid-femoral PWV over a follow-up of 5.3 years. In the multivariate analysis, the decrease in the PWV was only partly explained by the reduction in the mean BP. The authors concluded that the reduction in the PWV likely represented a delayed response to the long-term normalization of the BP, through arterial remodeling.16 Similarly, after a 12-month treatment period, the PWV was significantly smaller in the intensively treated hypertensive patients with a target BP of <130/85 mm Hg than in their moderately treated counterparts with a target BP of <140/90 mm Hg.12 These findings are in agreement with our study results. Indeed, the smaller increase in the PWV with age was driven by patients with well-controlled BP. It is possible that in some patients, irreversible structural damage may have occurred at the large artery level because of advanced stage and long-term hypertension. In our study, the median duration of hypertension (data obtained from a questionnaire) was 9.0 years (range, 1–49 years).
Several studies have demonstrated a beneficial effect of different classes of antihypertensive drugs on a reduction in the PWV.6, 7, 17, 18 Karalliede et al.7 compared the effect of the angiotensin receptor blocker valsartan/hydrochlorothiazide and amlodipine (a calcium-channel blocker) on the aortic PWV in 131 hypertensive type 2 diabetic patients. After a 24-week treatment period, the PWV decreased significantly in both treatment groups. Valsartan improved arterial stiffness by 0.9 m s−1 more than amlodipine, despite a similar decrease in the central and peripheral pulse pressure.7 After a 12-month follow-up in patients with essential hypertension, a combination of low-dose perindopril with indapamide reduced the aortic PWV significantly and to a similar extent as did treatment with atenolol.6 The decrease in the carotid and aortic BP was significantly more pronounced with the perindopril/indapamide combination than with atenolol, primarily because of the attenuation of wave reflection.6
The combination of amlodipine/valsartan compared with amlodipine/atenolol led to a similar decrease in the carotid-femoral PWV, despite a greater reduction in the central systolic BP in the former treatment group.18 In elderly subjects with essential hypertension, Kithas and Supiano17 showed a comparable beneficial effect of spironolactone and hydrochlorothiazide on arterial stiffness. The above-mentioned reports demonstrated the beneficial effect on the aortic pulse velocity by different classes of antihypertensive drugs alone or in combination, although the effect on the wave reflection parameters varied. In our study, 60% of the treated patients were on combination therapy, and the most commonly used drugs interfered with the renin–angiotensin system.
A lower PWV,1 but not augmentation index, central pulse pressure or pulse pressure amplification2 was associated with a lower overall cardiovascular risk even after adjustment for BP and other classical risk factors. In the untreated normotensive participants in the ACCT trial, the age-related change in the PWV was estimated to increase by 1.36 m s−1 per decade.19 A smaller age-associated increase of the PWV in our treated group compared with the untreated subjects is likely to be clinically relevant.
The present study must be interpreted within the context of its limitations and strengths. First, our study had a cross-sectional design. We can only speculate on whether the effects of antihypertensive drugs on the PWV were BP-dependent. Second, we did not have data regarding previously used antihypertensive treatments or the overall duration of these treatments. Thus, we are unable to distinguish the possible effect of these factors on our results. Similarly, because of the use of combination therapy in 60% of the subjects, we were unable to evaluate the effect of different drug classes on aortic stiffness. Third, the measurement of the hypertension control was based on the episodic blood pressure measured at rest and was not confirmed by a 24 -h ambulatory BP measurement.
In conclusion, we observed that the use of antihypertensive treatment lessened the PWV increase with age and with MAP in the general population, and this effect was driven predominantly by well-controlled patients. These findings might suggest that the reduction of aortic stiffening induced by antihypertensive treatment extends beyond its effect on clinical BP. The importance of our study is underscored by the epidemiological evidence that aortic PWV per se is an independent risk factor for cardiovascular morbidity and mortality.1, 2, 20 Further longitudinal studies should confirm the present observation.
References
Willum Hansen T, Staessen JA, Torp-Pedersen C, Rasmussen S, Thijs L, Ibsen H, Jeppesen J . Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation 2006; 113: 664–670.
Mitchell GF, Hwang SJ, Vasan RS, Larson MG, Pencina MJ, Hamburg NM, Vita JA, Levy D, Benjamin EJ . Arterial stiffness and cardiovascular events: the Framingham Heart Study. Circulation 2010; 121: 505–511.
Boutouyrie P, Tropeano AI, Asmar R, Gautier I, Benetos A, Lacolley P, Laurent S . Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: a longitudinal study. Hypertension 2002; 39: 10–15.
Blacher J, Safar ME, Guerin AP, Pannier B, Marchais SJ, London GM . Aortic pulse wave velocity index and mortality in end-stage renal disease. Kidney Int 2003; 63: 1852–1860.
Mancia G, De Backer G, Dominiczak A, Cífková R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Struijker Boudier HAJ, Zanchetti A . 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25: 1105–1187.
Asmar RG, London GM, O'Rourke ME, Safar ME . Improvement in blood pressure, arterial stiffness and wave reflections with a very-low-dose perindopril/indapamide combination in hypertensive patient: a comparison with atenolol. Hypertension 2001; 38: 922–926.
Karalliedde J, Smith A, DeAngelis L, Mirenda V, Kandra A, Botha J, Ferber P, Viberti G . Valsartan improves arterial stiffness in type 2 diabetes independently of blood pressure lowering. Hypertension 2008; 51: 1617–1623.
Matsui Y, Eguchi K, Shibasaki S, Ishikawa J, Hoshide S, Shimada K, Kario K, on behalf of the JMS-1 study group. Impact of arterial stiffness reduction on urinary albumin excretion during antihypertensive treatment: the Japan morning Surge-1 study. J Hypertens 2010; 28: 1752–1760.
Van Bortel LM, Struijker-Boudier HA, Safar ME . Pulse pressure, arterial stiffness, and drug treatment of hypertension. Hypertension 2001; 38: 914–921.
Mitchell GF, Izzo JL Jr, Lacourcière Y, Ouellet JP, Neutel J, Qian C, Kerwin LJ, Block AJ, Pfeffer MA . Omapatrilat reduces pulse pressure and proximal aortic stiffness in patients with systolic hypertension: results of the conduit hemodynamics of omapatrilat international research study. Circulation 2002; 105: 2955–2961.
Mitchell GF, Dunlap ME, Warnica W, Ducharme A, Arnold JMO, Tardif JC, Solomon SD, Domanski MJ, Jablonski KA, Rice MM, Pfeffer MA, for the Prevention of Events With Angiotensin-Converting Enzyme Inhibition Investigators. Long-term trandolapril treatment is associated with reduced aortic stiffness: the prevention of events with angiotensin-converting enzyme inhibition hemodynamic substudy. Hypertension 2007; 49: 1271–1277.
Ichihara A, Hayashi M, Koura Y, Tada Y, Hirota N, Saruta T . Long-term effects of intensive blood-pressure lowering on arterial wall stiffness in hypertensive patients. Am J Hypertens 2003; 16: 959–965.
Nakamura T, Fujii S, Hoshino J, Saito Y, Mizuno H, Saito Y, Kurabazashi M . Selective angiotensin receptor antagonism with valsartan decreases arterial stiffness independently of blood pressure lowering in hypertensive patients. Hypertens Res 2005; 28: 937–943.
Cífková R, Škodová Z, Lánská V, Adámková V, Novozámská E, Jozífová M, Plášková M, Hejl Z, Petržílková Z, Galovcová M, Palouš D . Prevalence, awareness, treatment, and control of hypertension in the Czech Republic. Results of two nationwide cross-sectional surveys in 1997/1998 and 2000/2001 Czech Post-MONICA Study. J Hum Hypertens 2004; 18: 571–579.
Wilkinson IB, Fuchs SA, Jansen IM, Spratt JC, Murray GD, Cockcroft JR, Webb DJ . Reproducibility of pulse wave velocity and augmentation index measured by pulse wave analysis. J Hypertens 1998; 16: 2079–2084.
Ait-Oufella H, Collin C, Bozec E, Laloux B, Ong KT, Dufouil C, Boutouyrie P, Laurent S . Long-term reduction in aortic stiffness: a 5.3-year follow-up in routine clinical practice. J Hypertens 2010; 28: 2336–2341.
Kithas PA, Supiano MA . Spironolactone and hydrochlorothiazide decrease vascular stiffness and blood pressure in geriatric hypertension. J Am Geriatr Soc 2010; 58: 1327–1332.
Boutouyrie P, Achouba A, Trunet P, Laurent S, for the EXPLOR Trialist Group. Amlodipine-valsartan combination decreases central systolic blood pressure more effectively than the amlodipine-atenolol combination: the EXPLOR study. Hypertension 2010; 55: 1314–1322.
McEniery CM, Yasmin, Hall IR, Qasem A, Wilkinson IB, Cockcroft JR, on behalf of the ACCT Investigators. Normal vascular aging: differential effects on wave reflection and aortic pulse wave velocity: the Anglo-Cardiff Collaborative Trial (ACCT). J Am Coll Cardiol 2005; 46: 1753–1760.
Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, Ducimetiere P, Benetos A . Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 2001; 37: 1236–1241.
Acknowledgements
This study would not have been possible without the voluntary collaboration of the participants. We acknowledge the expert technical assistance of Ms Alena Maříková. This study was supported by the Charles University Research Fund (project number P36), by project ED2.1.00/03.0076 from the European Regional Development Fund and by unrestricted research grants from the Krka Czech Republic s.r.o. and Servier Czech Republic s.r.o. The manuscript has not been published and is not being considered for publication elsewhere, in whole or in part, in any language, except as an Abstract.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Seidlerová, J., Filipovský, J., Mayer, O. et al. Positive effects of antihypertensive treatment on aortic stiffness in the general population. Hypertens Res 37, 64–68 (2014). https://doi.org/10.1038/hr.2013.113
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2013.113
Keywords
This article is cited by
-
Use of Antihypertensive Drugs and Arterial Stiffness in the Longitudinal Study of Adult Health (ELSA-Brasil)
Cardiovascular Drugs and Therapy (2023)
-
Second derivative of the finger photoplethysmogram and cardiovascular mortality in middle-aged and elderly Japanese women
Hypertension Research (2017)
-
Measurement of pulse wave velocity in normal ageing: comparison of Vicorder and magnetic resonance phase contrast imaging
BMC Cardiovascular Disorders (2016)
-
Plasma PCSK9 level is unrelated to blood pressure and not associated independently with carotid intima–media thickness in hypertensives
Hypertension Research (2016)
-
Influence of the central-to-peripheral arterial stiffness gradient on the timing and amplitude of wave reflections
Hypertension Research (2016)