Abstract
Purpose
To evaluate and compare the diagnostic accuracy of the Humphrey Field Analyzer (HFA), Octopus perimetry, and Cirrus OCT for glaucomatous optic neuropathy.
Methods
Eighty-eight healthy individuals and 150 open-angle glaucoma patients were consecutive and prospectively selected. Eligibility criteria for the glaucoma group were intraocular pressure ≥21 mm Hg and glaucomatous optic nerve head morphology. All subjects underwent a reliable standard automated perimetry with the HFA and Octopus perimeter, and were imaged with the Cirrus OCT. Receiver-operating characteristic (ROC) curves were plotted for the threshold values and main indices of the HFA and Octopus, the peripapillary retinal nerve fiber layer thicknesses, and the optic nerve head parameters. Sensitivities at 85 and 95% fixed-specificities were also calculated. The best areas under the ROC curves (AUCs) were compared using the DeLong method.
Results
In the glaucoma group, mean deviation (MD) was −5.42±4.6 dB for HFA and 3.90±3.6 dB for Octopus. The MD of the HFA (0.966; P<0.001), mean sensitivity of the Octopus (0.941; P<0.001), and average cup-to-disc (C/D) ratio measured by the Cirrus OCT (0.958; P<0.001) had the largest AUCs for each test studied. There were no significant differences among them. Sensitivities at 95% fixed-specificity were 82% for pattern standard deviation of the HFA, 81.3% for average C/D ratio of OCT, and 80% for the MD of the Octopus.
Conclusions
HFA, Octopus, and Cirrus OCT demonstrated similar diagnostic accuracies for glaucomatous optic neuropathy. Visual field and OCT provide supplementary information and thus these tests are not interchangeable.
Similar content being viewed by others
Introduction
Primary open-angle glaucoma is generally considered a progressive optic neuropathy, including damage at the optic nerve head (ONH) and/or retinal nerve fiber layer (RNFL), and reduced visual function.1 Randomized clinical trials indicate that the first detectable glaucomatous change at early stages of the disease can be either functional or structural.2, 3 The agreement among RNFL, neuroretinal rim, and visual field (VF) measurements for detecting progression, however, is poor,4, 5, 6 and a combination of structural and functional tests is therefore used to increase the diagnostic sensitivity and detection of progression.7, 8
Standard automated perimetry (SAP) has become the functional clinical standard for diagnosing and monitoring patients with glaucoma. Particularly, the 24-2 Swedish Interactive Threshold Algorithm (SITA) of the Humphrey Field Analyzer (HFA)9 and the G1 Tendency-Oriented Perimetry strategy (TOP) of the Octopus10 are among the most commonly used VF algorithms worldwide. Objective structural imaging instruments have also been standardized for the diagnosis and follow-up of patients with, or at risk for, glaucoma. One of these tools is optical coherence tomography (OCT), which provides quantitative and reproducible measurements of the ONH parameters and peripapillary RNFL thickness.11, 12, 13, 14, 15 Understanding their comparative roles and performance in clinical practice is key to the management of glaucoma.
Current knowledge of the relative diagnostic performance of both SAPs (HFA and Octopus) and OCT comes from studies in which the data were analyzed independently for each test or where only one kind of SAP was compared with a structural test.11, 12, 13, 14, 15, 16, 17, 18, 19, 20 Some studies compared tests for evaluating the VF based on other stimuli than white-on-white perimetry,21, 22, 23, 24, 25, 26, 27 or evaluated the structure–function relationship.28, 29, 30, 31, 32, 33 The objective of the present study was to evaluate and compare the glaucoma diagnostic accuracy of the most widely used VF testing algorithms in clinical practice (24-2 SITA Standard strategy of HFA and G1 TOP strategy of Octopus) with one of the most advanced structural imagining tests (OCT). To the best of our knowledge, this is the first study aimed at comparing the diagnostic accuracy of these tests.
Materials and methods
Participants
The Institutional Review Board approved the prospective study protocol. All participants provided informed consent prior to enrollment and the study methodology adhered to the tenets of the Helsinki Declaration for biomedical research.
A sample of 249 consecutive subjects was prospectively preselected. Glaucoma patients were recruited from the Department of Ophthalmology of the Gregorio Maranon University Hospital and the Glaucoma Clinic of the Moncloa Hospital (Madrid, Spain). Controls were enrolled from patients referred for refraction without abnormal ocular findings, relatives of patients, and friends and family of the hospital staff.
Inclusion criteria for the glaucoma group were a glaucomatous optic disc morphology and intraocular pressure (IOP) ≥21 mm Hg, regardless of the SAP or OCT outcomes. The control group had normal optic disc morphology and IOP <21 mm Hg.
The morphology of the ONH was evaluated by slit-lamp indirect ophthalmoscopy with a 90-diopter lens. The optic discs were evaluated by two glaucoma specialists masked to patient identity and clinical history, and any disagreement was resolved by consensus. Glaucomatous optic disc appearance was defined as focal (localized notching) or diffuse neuroretinal rim narrowing with concentric enlargement of the optic cup or both.
All participants met the following inclusion criteria: best-corrected visual acuity >20/40, refractive error <5 D sphere and 2 cylinder, transparent ocular media (nuclear color/opalescence, cortical or posterior subcapsular lens opacity <1) according to the Lens Opacities Classification System III system,34 and open anterior chamber angle. Subjects with previous intraocular surgery, diabetes or other systemic diseases, history of ocular or neurologic disease, or current use of a medication that could affect VF sensitivity were excluded.
Participants underwent full ophthalmologic examination: clinical history, visual acuity, biomicroscopy of the anterior segment using a slit lamp, gonioscopy, Goldmann applanation tonometry, central corneal ultrasonic pachymetry, and ophthalmoscopy of the posterior segment.
Visual field measurements
All participants underwent at least two white-on-white SAPs with the HFA (Humphrey Zeiss Systems, Dublin, CA, USA; 24-2 SITA Standard strategy) and at least two SAPs with the Octopus (Haag-Streit International, Koeniz, Switzerland; G1 TOP test strategy) to minimize the learning effect. If the perimetry was not reliable (fixation losses <20% and false positive and negative rates <15%), the test was repeated. The last reliable perimetry was included in the statistical analysis. The subjects completed the perimetry tests before undergoing clinical examination or structural testing. Each perimetry examination was performed on different days to avoid a fatigue effect.
HFA and Octopus perimeters use the same background lighting of 31.5 apostilbs (asb). Retinal sensitivity measured by both perimetry types is indicated in decibels (dB), which are tenths of a log unit. Nonetheless, the maximal luminance varied between the instruments. A 0 dB value was the maximum brightness, which corresponds to a 10 000 asb stimulus intensity for HFA, and 4000 asb for Octopus perimetry.
OCT measurements
Peripapillary RNFL thickness and optic disc morphometric parameters were measured using the Optic Disc Cube 200 × 200 scanning protocol of the Cirrus OCT (Carl Zeiss Meditec). For image acquisition, scanning laser images were focused after subjects were seated and properly positioned. The left eye data were converted to a right eye format (Figure 1). All images were artifact-free and acquired with a quality greater than >6/10. The same trained operator performed all scans.
Statistical analyses
All statistical analyses were calculated using SPSS for Mac (version 22.0, IBM corporation, Somers, NY, USA) and Windows MedCal statistical software (version 15; Mariakerke, Belgium). Minimum sample size should be eight individuals per group considering a difference of 25.1 μm for the average thickness as significant,14 with a type 1 error rate of 0.01, and a power of 90%. All variables studied were normally distributed, as verified by the Kolmogorov–Smirnov test. Demographics, HFA, Octopus, and OCT parameters were compared between groups with independent t-tests.
Each of the mean threshold values at each point of the VF was numbered (Figure 1). To evaluate the diagnostic ability for glaucoma, the receiver-operating characteristic (ROC) curves were plotted for the RNFL and ONH parameters acquired with OCT, and for all the HFA and Octopus study points and main parameters. Sensitivities at 85 and 95% fixed-specificities were also calculated. The best areas under the ROC curves (AUCs) were compared using the DeLong method, which is an algorithm for the calculation of the standard error of the AUC and of the difference between two AUCs.35 Using Bonferroni's correction for multiple comparisons, a P-value ≤0.001 was considered significant.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Results
Of the 249 enrolled participants, 11 did not complete all required tests and were excluded from further analysis. In total, 150 eyes of 150 glaucoma patients and 88 eyes of 88 healthy subjects were enrolled. Their clinical characteristics are summarized in Table 1. Comparison of the clinical characteristics revealed significant differences (P<0.001) in all the parameters except age, sex, and laterality of eye included.
Among the 150 glaucoma participants, 24 had normal HFA results according to pattern standard deviation (PSD) or the glaucoma hemifield test. Three participants of the control group presented with PSD beyond 5% probability level. This finding can be explained as part of the VF learning process. Among the 150 glaucoma participants, 32 had normal Octopus results based on mean deviation (MD <2 dB). All the controls had normal Octopus results.
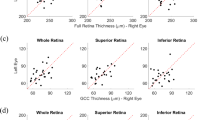
Figure 2 represents the mean sensitivity (MS) at each study point of the VF evaluated with the HFA and Octopus in the two study groups. There was a clear depression of the sensitivity at all points of the VF in the glaucoma group, which was especially significant in the area corresponding to the upper arcuate defects and nasal step (orange-red color in HFA and yellow-orange in Octopus). All threshold values of both the HFA and Octopus were significantly different (P<0.001) between normal subjects and the glaucoma group (Student’s t-test).
All peripapillary RNFL thickness and ONH parameters measured with OCT were significantly different between healthy and glaucoma patients, except for at the 3 (nasal sector; P=0.306) and 9 clock-hour positions (temporal sector; P=0.035), and the disc area (P=0.536).
Diagnostic ability of the RNFL thickness and ONH parameters measured by OCT
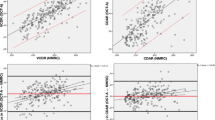
To evaluate the diagnostic ability for glaucoma of the three studied tests, the AUCs were calculated with their 95% confidence intervals. AUCs of the RNFL thickness measurements and ONH parameters measured by OCT are presented in Figure 3 (bottom). Among these parameters, Mean cup-to-disc (C/D) ratio had the largest AUC (0.958; 95% CI: 0.937–0.980; P<0.001), followed by the Vertical C/D ratio (0.957; 95% CI: 0.935–0.978; P<0.001), and Rim area (0.952; 95% CI: 0.927–0.977; P<0.001). Except for the Disc area (0.513; 95% CI: 0.437–0.587; P=0.74), all parameters had AUCs >0.90 (P<0.001).
The RNFL thicknesses showed good diagnostic ability in the superior and inferior quadrants and 5–7 and 11–2 clock-hour positions (AUCs >0.774; P<0.001). The AUCs of the RNFL thickness in the nasal and temporal quadrants, and at the 3, 4, and 8 to 10 clock-hour positions, however, ranged from 0.599 to 0.710 (Figure 3). The inferior quadrant thickness (0.926; 95% CI: 0.894–0.958; P<0.001), Mean thickness (0.918; 95% CI: 0.885–0.952; P<0.001), and RNFL thickness at the 7 clock-hour position (0.905; 95% CI: 0.869–0.940; P<0,001) had the largest AUCs.
Diagnostic ability of HFA
Figure 3 (top and right) represents the AUCs of the main HFA indices. The largest AUCs were observed for the MD (0.966; 95% CI: 0.945–0.987; P<0.001) and VF index (VFI) (0.961; 95% CI: 0.934–0.987; P<0.001). The largest AUCs were found for the threshold values at point 7 (0.901; 95% CI: 0.857–0.944; P<0.001), point 19 (0.911; 95% CI: 0.867–0.954; P<0.001), point 20 (0.923; 95% CI: 0.886–00.961; P<0.001), and point 21 (0.914; 95% CI: 0.875–0.954; P<0.001).
Diagnostic ability of Octopus Perimetry
Figure 3 (top and left) represents the AUCs of the main Octopus indices. The largest AUCs were observed for MS (0.941; 95% CI: 0.913–0.969; P<0.001). The largest AUCs were observed for the threshold values at point 3 (0.907; 95% CI: 0.870–0.944; P<0.001), point 5 (0.900; 95% CI: 0.861–0.940; P<0.001) and point 21 (0.911; 95% CI: 0.877–0.946; P<0.001).
Comparison of the diagnostic ability between the HFA, Octopus, and OCT
Overall, the best sensitivity/specificity balance was observed for the VFI of HFA (91.3–89.8%; cutoff point ≤98) and the PSD of HFA (87.3–93.2%; cutoff point >1.88). The Octopus parameter with the best sensitivity-specificity balance was MD (84.6–94.3%; cutoff point >0.75). Table 2 represents sensitivities at 85 and 95% fixed-specificities. At 85% fixed-specificity, the best parameter for discriminating between control and glaucoma patients was the VFI of HFA (93.3%), and at 95% fixed-specificity the best parameter to discriminate between control and glaucoma eyes was the PSD of HFA (82.0%).
The comparison of the best AUCs (DeLong method) of the three-study test did not show significant differences between them. No differences were detected (significant differences were considered when P≤0.001) between the MD of the HFA and the MS of the Octopus (P=0.042), or between the MD of the HFA and RNFL thickness at the inferior quadrant (P=0.027).
Discussion
Our study was designed to assess and compare the diagnostic accuracy of the 24-2 SITA-Standard algorithm of HFA, the G1 TOP strategy of the Octopus, and OCT to discriminate between normal and glaucoma patients. The best parameter to discriminate between healthy and glaucoma eyes at 95% fixed specificity was the PSD of the HFA (sensitivity 82.0%). Additionally, HFA parameters presented better numerical AUCs than the Octopus and OCT parameters, but comparison of the ROC curves revealed no significant differences in the diagnostic ability of the three tests. Nevertheless, the P<0.001 condition for statistical significance was set high due to multiple comparisons, and this fact is actually limiting the ability to compare the tests. Although the DeLong method did not show significant differences, we should take into account that the low P-values are suggestive of a difference, even if they do not reach the fixed level to be considered as significant in this study.
The main parameters of the HFA and Octopus (Figure 3, top) had good accuracy for discriminating between normal and glaucoma eyes (all AUCs >0.929; P<0.001). The VF parameters with the best AUCs were MD of the HFA (0.966; 95% CI: 0.945–0.987; P<0.001) and MS of the Octopus (0.941; 95% CI: 0.913–0.969; P<0.001). Our inclusion criteria were very strict and only included participants with transparent ocular media. This fact may have led to these results, where the MD of the HFA and the MS of the Octopus had larger AUCs than PSD of the HFA and square root of loss of variance (sLV) of the Octopus, which are usually more sensitive for detecting focal losses instead of diffuse vision loss. The study population was selected to avoid any other ocular pathologies than glaucoma in the glaucoma group. Participants presented with very good visual acuities, no cataracts, and no previous intraocular surgeries.
We found similar sensitivities at fixed specificities for the main indices of the Octopus. In a study published in 2006 by De la Rosa et al18 analyzing the diagnostic accuracy and reproducibility of TOP in glaucoma, the Octopus MD and Octopus LV had similar diagnostic precision for moderate and advanced glaucoma, but the LV was the best diagnostic index when the MD was <6 dB.
The largest AUCs were for the MD of the HFA (0.966; 95% CI: 0.945–0.987; P<0,001) and the VFI of the HFA (0.961; 95% CI: 0.934–0.987; P<0.001). Although the VFI presented the best sensitivity/specificity balance and the best sensitivity (93%) at 85% fixed specificity, clinicians should take into account the ceiling effect that occurs in VFI with MDs better than −5 dB.36
Study points with the largest AUCs were located in the superior hemifield: points 7, 19, 20, and 21 of the HFA, and points 3 and 21 of the Octopus. These study points represent a superior arcuate defect and a nasal step, locations of very typical glaucomatous VF defects.37, 38, 39 Paracentral points (19 and 10) have also been documented as very typical of glaucoma, especially when regionally enhanced spatial resolution is used,40 but points close to the fovea did not present with good AUCs in our sample (mild glaucoma). We used non-equivalent strategies from both perimetry types, SITA Standard and TOP, because they are the default strategies used in clinical practice. Our objective was to analyze the strategies that are normally used in clinical practice.
In this study, optic disc parameters presented with numerically better AUCs than RNFL thickness measurements. Three of the optic disc parameters measured by the OCT had the largest AUCs: average C/D ratio (0.958; 95% CI: 0.937–0.98; P<0.001), vertical C/D ratio (0.957; 95% CI: 0.935–0.978; P<0.001), and rim area (0.952; 95% CI: 0.927–0.977; P<0.001). Our results are among the best in the literature, especially considering that our glaucoma group basically comprised early glaucomatous eyes according to the Hodapp–Parrish–Anderson score (MD of HFA was −5.42±4.6 dB).41 It is important to note, however, that patients were selected because of the optic disc appearance regardless of the VF or the OCT results, which may have biased the ONH parameters to be more accurate for differentiating between normal and eyes with glaucomatous optic neuropathy. Mwanza et al13 found similar OCT diagnostic ability. They studied 73 glaucomatous eyes and 146 control eyes, and observed the largest AUCs for the rim area (0.912) and the vertical C/D ratio (0.890). This last parameter, vertical C/D ratio, had the best AUC (0.962) in a very similar study published by the same group that included 58 glaucomatous eyes and 99 controls.42 A recent similar study43 that included a large sample (209 glaucomatous eyes, 405 pre-perimetric glaucomatous eyes, and 109 controls) had worse results compared with our study and that of Mwanza et al13 Only rim area presented a relatively good AUC and it was worse than that of the average RNFL thickness. One potential reason for this is that they included glaucomatous eyes at an earlier stage of the disease. Indeed, the diagnostic ability improved when advance glaucoma cases were selected. Pollet-Villard et al32 reported similar results.
Many studies have confirmed the good diagnostic ability of peripapillary RNFL thickness measured by OCT.11, 12, 13 In our study, the best AUC was for the RNFL thickness at the inferior quadrant (0.926; 95% CI: 0.894–0.958; P<0.001), followed by the average RNFL thickness (0.918; 95% CI: 0.885–0.952; P<0.001) and the RNFL thickness at the 7 clock-hour position (0.905; 95% CI: 0.869–0.940; P<0.001). These three parameters also had the best AUCs in the Mwanza et al study.13
Comparison of measurements obtained by the Cirrus and Stratus OCT indicates that both tests have the same diagnostic ability despite the better reproducibility of the Cirrus OCT.26, 44, 45 Most of the studies show consistency in the parameters with the best AUCs: RNFL thickness at the inferior quadrant, RNFL thickness at the 7 and 6 clock-hour positions, and average RNFL thickness.40, 46 These results support the idea that early glaucoma damage usually starts at the superior and inferior optic disc poles.14, 30, 47, 48
In conclusion, the HFA, Octopus, and Cirrus OCT did not significantly differ in their ability to discriminate glaucomatous optic neuropathy. The three tests demonstrated very good diagnostic ability for discriminating between healthy and glaucomatous eyes.

References
Foster JP, Buhrman R, Quigley HA . The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol 2002; 86: 238–242.
Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP et al. The ocular hyper- tension treatment study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120: 701–713.
European Glaucoma Prevention Study (EGPS) Group. Results of the European glaucoma prevention study. Ophthalmology 2005; 112: 366–375.
Leung CK, Liu S, Weinreb RN, Lai G, Ye C, Cheung CY et al. Evaluation of retinal nerve fiber layer progression in glaucoma a prospective analysis with neuroretinal rim and visual field progression. Ophthalmology 2011; 118: 1551–1557.
Gonzalez-Hernandez M, Pablo L, Armas-Dominguez K, Rodriguez de la Vega R, Ferreras A, Gonzalez et al. Structure-function relationship depends on glaucoma severity. Br J Ophthalmol 2009; 93: 1195–1199.
López-Peña MJ, Ferreras A, Larrosa JM, Polo V, Pablo LE . Relationship between standard automated perimetry and retinal nerve fiber layer parameters obtained with optical coherence tomography. J Glaucoma 2011; 20: 422–432.
Shah NN, Bowd C, Medeiros FA, Weinreb RN, Sample PA, Hoffmann EM et al. Combining structural and functional testing for detection of glaucoma. Ophthalmology 2006; 113: 1593–1602.
Garway-Heath DF, Friedman DS . How should results from clinical tests be integrated into the diagnostic process? Ophthalmology 2006; 113: 1479–1480.
Bengtsson B, Olsson J, Heijl A, Rootzén H . A new generation of algorithms for computerized threshold perimetry, SITA. Acta Ophthalmol Scand 1997; 75: 368–375.
Morales J, Weitzman ML, González de la Rosa M . Comparison between tendency-oriented perimetry (TOP) and octopus threshold perimetry. Ophthalmology 2000; 107: 134–142.
Leung CK, Choi N, Weireb RN, Liu S, Ye C, Liu L et al. Retinal nerve fiber layer imaging with spectral-domain optical coherence tomography pattern of RNFL defects in glaucoma. Ophthalmology 2010; 117: 2337–2344.
Hwang YH, Kim YY . Glaucoma diagnostic ability of quadrant and clock-hour neuroretinal rim assessment using Cirrus HD optical coherence tomography. Invest Ophthalmol Vis Sci 2012; 53: 2226–2234.
Mwanza JC, Oakley JD, Budenz DL, Anderson DR Cirrus Optical Coherence Tomography Normative Database Study Group. Ability of Cirrus HD-OCT optic nerve head parameters to discriminate normal from glaucomatous eyes. Ophthalmology 2011; 118: 241–248.
Ferreras A, Pablo LE, Pajarín AB, Larrosa JM, Polo V, Honrubia FM . Logistic regression analysis for early glaucoma diagnosis using optical coherence tomography. Arch Ophthalmol 2008; 126: 465–470.
Bowd C, Hao J, Tavares IM, Medeiros FA, Zangwill LM, Lee TW et al. Bayesian machine learning classifiers for combining structural and functional measurements to classify healthy and glaucomatous eyes. Invest Ophthalmol Vis Sci 2008; 49: 945–953.
Pablo LE, Ferreras A, Pajarin AB, Fogagnolo P . Diagnostic ability of a linear discriminant function for optic nerve head parameters measured with optical coherence tomography for perimetric glaucoma. Eye 2010; 24: 1051–1057.
Leung CK, Cheung CY, Weinreb RN, Qiu Q, Liu S, Li H et al. Retinal nerve fiber layer imaging with spectral-domain optical coherence tomography: a variability and diagnostic performance study. Ophthalmology 2009; 116: 1257–1263.
Gonzalez de la Rosa M, Gonzalez-Hernandez M, Garcia Feijoo J, Morales J, Azuara-Blanco A . Diagnostic accuracy and reproducibility of tendency oriented perimetry in glaucoma. Eur J Ophthalmol 2006; 16: 259–267.
Birt CM, Shin DH, Samudrala V, Hughes BA, Kim C, Lee D . Analysis of reliability indices from Humphrey visual field tests in an urban glaucoma population. Ophthalmology 1997; 104: 1126–1130.
Chang RT, Knight OJ, Feuer WJ, Budenz DL . Sensitivity and specificity of time-domain versus spectral-domain optical coherence tomography in diagnosing early to moderate glaucoma. Ophthalmology 2009; 116: 2294–2299.
Pierre-Filho Pde T, Schimiti RB, de Vasconcellos JP, Costa VP . Sensitivity and specificity of frequency-doubling technology, tendency-oriented perimetry, SITA standard and SITA Fast perimetry in perimetrically inexperienced individuals. Acta Ophthalmol Scand 2006; 84: 345–350.
Papp A, Kis K, Németh J . Conversion formulas between automated-perimetry indexes as measured by two different types of instrument. Ophthalmologica 2001; 215: 87–90.
Wadood AC, Azuara-Blanco A, Aspinall P, Taguri A, King AJ . Sensitivity and specificity of frequency-doubling technology, tendency-oriented perimetry, and Humphrey Swedish interactive threshold algorithm-fast perimetry in a glaucoma practice. Am J Ophthalmol 2002; 133: 327–332.
Ferreras A, Polo V, Larrosa JM, Pablo LE, Pajarín AB, Pueyo V et al. Can frequency-doubling technology and short-wavelength automated perimetries detect visual field defects before standard automated perimetry in patients with pre-perimetric glaucoma? J Glaucoma 2007; 16: 372–383.
Fogagnolo P, Rossetti L, Ranno S, Ferreras A, Orzalesi N . Short-wavelength automated perimetry and frequency-doubling technology perimetry in glaucoma. Prog Brain Res 2008; 173: 101–124.
Racette L, Chiou CY, Hao J, Bowd C, Goldbaum MH, Zangwill LM et al. Combining functional and structural tests improves the diagnostic accuracy of relevance vector machine classifiers. J Glaucoma 2010; 19: 167–175.
Horn FK, Mardin CY, Bendchneider D, Jünemann AG, Adler W, Tornow RP . Frequency doubling technique perimetry and spectral domain optical coherence tomography in patients with early glaucoma. Eye 2011; 25: 17–29.
Garway-Heath DF, Poinoosawmy D, Fitzke FW, Hitchings RA . Mapping the visual field to the optic disc in normal tension glaucoma eyes. Ophthalmology 2000; 107: 1809–1815.
Gardiner SK, Johnson CA, Cioffi GA . Evaluation of the structure-function relationship in glaucoma. Invest Ophthalmol Vis Sci 2005; 46: 3712–3717.
Bowd C, Zangwill LM, Medeiros FA, Tavares IM, Hoffmann EM, Bourne RR et al. Structure-function relationships using confocal scanning laser ophthalmoscopy, optical coherence tomography, and scanning laser polarimetry. Invest Ophthalmol Vis Sci 2006; 47: 2889–2895.
Ferreras A, Pablo LE, Garway-Heath DF, Fogagnolo P, García-Feijoo J . Mapping standard automated perimetry to the peripapillary retinal nerve fiber layer in glaucoma. Invest Ophthalmol Vis Sci 2008; 49: 3018–3025.
Pollet-Villard F, Chiquet C, Romanet JP, Noel C, Aptel F . Structure-function relationships with spectral-domain optical coherence tomography retinal nerve fiber layer and optic nerve head measurements. Invest Ophthalmol Vis Sci 2014; 55: 2953–2962.
Monsalve B, Ferreras A, Khawaja AP, Calvo P, Ara M, Fogagnolo P et al. The relationship between structure and function as measured by OCT and Octopus perimetry. Br J Ophthalmol 2015; 99: 1230–1235.
Chylack LT Jr, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL et al. The lens opacities classification system III. the longitudinal study of cataract study group. Arch Ophthalmol 1993; 111: 831–836.
DeLong ER, DeLong DM, Clarke-Pearson DL . Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988; 44: 837–845.
Artes PH, O'Leary N, Hutchison DM, Heckler L, Sharpe GP, Nicolela MT et al. Properties of the statpac visual field index. Invest Ophthalmol Vis Sci 2011; 52: 4030–4038.
Nascimento VC, Kasahara N, Cohen R, Almeida GV, Mandia C Jr, Paolera MD et al. Location and frequency of visual field defects as measured by SITA (Swedish Interactive Threshold Algorithm) strategy in primary open angle glaucoma. Arq Bras Oftalmol 2005; 68: 661–665.
Lau LI, Liu CJ, Chou JC, Hsu WM, Liu JH . Patterns of visual field defects in chronic angle-closure glaucoma with different disease severity. Ophthalmology 2003; 110: 1890–1894.
Schiefer U, Papageorgiou E, Sample PA, Pascual JP, Selig B, Krapp E et al. Spatial pattern of glaucomatous visual field loss obtained with regionally condensed stimulus arrangements. Invest Ophthalmol Vis Sci 2010; 51: 5685–5689.
Sihota R, Gupta V, Tuli D, Sharma A, Sony P, Srinivasan G . Classifying patterns of localized glaucomatous visual field defects on automated perimetry. J Glaucoma 2007; 16: 146–152.
Hodapp E, Parrish RK II, Anderson DR . Clinical Decisions in Glaucoma. Mosby: St Louis, MO, USA, 1993; 52–61.
Mwanza JC, Durbin MK, Budenz DL, Sayyad FE, Chang RT, Neelakantan A et al. Glaucoma diagnostic accuracy of ganglion cell-inner plexiform layer thickness: comparison with nerve fiber layer and optic nerve head. Ophthalmology 2012; 119: 1151–1158.
Sung KR, Na JH, Lee Y . Glaucoma diagnostic capabilities of optic nerve head parameters as determined by Cirrus HD optical coherence tomography. J Glaucoma 2012; 21: 498–504.
Chen HY, Chang YC, Wang IJ, Chen WC . Comparison of glaucoma diagnoses using stratus and Cirrus optical coherence tomography in different glaucoma types in a Chinese population. J Glaucoma 2013; 22 (8): 638–646.
Moreno-Montañés J, Olmo N, Alvarez A, García N, Zarranz-Ventura J . Cirrus high-definition optical coherence tomography compared with stratus optical coherence tomography in glaucoma diagnosis. Invest Ophthalmol Vis Sci 2010; 51: 335–343.
Chen HY, Chang YC . Meta-analysis of stratus OCT glaucoma diagnostic accuracy. Optom Vis Sci 2014; 91: 1129–1139.
Uchida H, Brigatti L, Caprioli J . Detection of structural damage from glaucoma with confocal laser image analysis. Invest Ophthalmol Vis Sci 1996; 37: 2393–2401.
Pablo LE, Ferreras A, Fogagnolo P, Figus M, Pajarín AB . Optic nerve head changes in early glaucoma: a comparison between stereophotography and Heidelberg retina tomography. Eye 2010; 24: 123–130.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Monsalve, B., Ferreras, A., Calvo, P. et al. Diagnostic ability of Humphrey perimetry, Octopus perimetry, and optical coherence tomography for glaucomatous optic neuropathy. Eye 31, 443–451 (2017). https://doi.org/10.1038/eye.2016.251
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2016.251
This article is cited by
-
Influence of implantation of diffractive trifocal intraocular lenses on standard automated perimetry
BMC Ophthalmology (2022)
-
Infrared- and white-light retinal sensitivity in glaucomatous neuropathy
Scientific Reports (2022)
-
Comparison of the visual field test of Glaufield Lite with Humphrey Field Analyser
International Ophthalmology (2022)