Abstract
Purpose
To describe prognostic factors and survival outcomes in patients who underwent orbital exenteration for periocular non-melanoma cutaneous malignancies.
Methods
The authors performed an institutional review board-approved retrospective review of all patients who underwent orbital exenteration for non-melanoma periocular cutaneous malignancies at a tertiary care hospital system over a 10-year period. Patient demographics, tumor, and treatment data were recorded. Survival outcomes included disease-free survival (DFS) and overall survival (OS). Log-rank tests were used to test for difference in survival curves among various potential prognostic indicators, and multivariate analysis was performed using Cox’s proportional hazards model.
Results
Forty-nine patients with an average age of 70.3 years were followed with a median follow-up of 17.5 months. At 2 years the OS was 78% while the DFS was 61%. The mean DFS for basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and sebaceous gland carcinoma (SGC) were 52.6, 39.2 and 28.1 months, respectively. Multivariate analysis demonstrated that only positive final surgical margin was predictive of worse outcome (P=0.002). Recurrences were most frequent in the first 2 years.
Conclusions
Despite the relatively more aggressive nature of periocular malignancies that have invaded the orbit, orbital exenteration offers an overall 2-year DFS of ~60%. BCC had the greatest mean survival time, however this was not statistically significant. We found worse prognosis with positive final surgical margins and recommend a multidisciplinary surgical approach to achieve complete resection when indicated.
Similar content being viewed by others
Introduction
Non-melanoma skin malignancies of the eyelids and periocular region are common, and comprise between 5 and 10 percent of all skin cancers.1, 2 Often these tumors are diagnosed early and treated definitively with surgical excision (most commonly Mohs micrographic surgery).3 Early detection is important, as these tumors can invade the orbit in 2–4% of cases.1, 4 The most common non-melanoma cutaneous malignancies affecting the periocular region are basal cell carcinoma (BCC), squamous cell carcinoma (SCC) and sebaceous gland carcinoma (SGC), all of which can invade the orbit.
BCC is the most common malignant periorbital skin tumor, and while orbital invasion is considered rare, it may occur in recurrent disease, incompletely excised medial canthal tumors, or less common, more aggressive histological subtypes.5 When orbital invasion of BCC occurs, it has a similarly poor prognosis as other periorbital malignancies, such as SCC.6 While SCC is a less common periocular malignancy, 20–30% of periocular SCC is multifocal at the time of diagnosis1, 7 with regional involvement in between 1 and 24.3% of cases.7, 8 Perineural invasion occurs in 3–14% of squamous cell carcinomas and is associated with a worse prognosis.1, 8 SGC is a rare, aggressive cancer that not only spreads locally but also demonstrates significant metastatic potential with lymph node involvement present in 30% of cases.9, 10 Reported overall mortality from SGC ranges from 18 to 30% and tumors that involve the upper and lower eyelids, are greater than 10mm in diameter, demonstrate pagetoid spread, or invade the orbit have a worse prognosis.10, 11 Risk factors for orbital invasion for all three tumor types include tumor size, medial canthal location, aggressive histological subtype, multiply recurrent tumors, perineural spread, pagetoid spread (in cases of SGC)1 and age.4, 12, 13 Although clinical signs including a palpable mass with bony fixation, impaired ocular motility, and globe displacement are all highly suggestive of orbital involvement, more than one third of patients with orbital invasion are initially asymptomatic.5, 14
Orbital exenteration refers to complete excision of periorbital tissues, orbital contents, and orbital fat, extraocular muscles, bulbar conjunctiva, and sclera.1, 15 It is indicated for tumors of the orbit, periorbita, conjunctiva, globe, and paranasal sinuses that have invaded the orbital apex, retrobulbar fat, extraocular muscles, bulbar conjunctiva, or sclera and which are potentially fatal, progressive, and cannot be effectively treated by other modalities.1, 16 Although total exenteration refers to the removal of all orbital tissue (including the periorbita) posterior to the orbital rim, in some cases the eyelids may be preserved and used in reconstruction.1 When bone resection is required (which is typically anterior ethmoidectomy and total maxillectomy), the procedure is referred to as an extended orbital exenteration.9 Obtaining clear margins is an important goal of orbital exenteration. Clear margin status, however, has previously not been associated with improved prognosis in patients undergoing exenteration for malignancies with orbital invasion.6, 17, 18 However, these studies represent a significant mix of histologic subtype (including melanoma) and site of origin (including sinonasal and primary orbital). Due to the relative rarity of orbital invasion in periorbital skin cancers, there are few reported studies that specifically examine orbital exenteration for non-melanoma malignancies arising from periocular tissue, and none that address prognostic factors and survival in this group.
The goal of this study is to better characterize the prognostic factors, complications, and outcomes for patients undergoing orbital exenteration specifically for non-melanoma periorbital malignancies. We hypothesize that the following clinical factors will be predictive of a worse prognosis: recurrent disease, decreased visual acuity or diplopia, bone erosion on preoperative imaging, preoperative pain, and positive surgical margins. In addition, we hypothesize that BCC has better survival outcomes than both SCC and SGC, due to its relatively less aggressive clinical course.
Materials and methods
This retrospective single case series was conducted in accordance with the amended Declaration of Helsinki and approved by the Institutional Review Board at the University of Miami Miller School of Medicine, protocol number 20120608. All charts of the 99 total patients with a history of orbital exenteration as per billing codes between January 2002 and January 2012 at Bascom Palmer Eye Institute, University of Miami Hospital, and Jackson Memorial Hospital were reviewed. Patients undergoing orbital exenteration for melanoma or cancers of any histology that did not arise from periocular skin were excluded from the study. Forty-nine cases of periorbital non-melanoma skin cancer resulting in total and/or extended orbital exenteration were included in the study. Patient demographics, clinical presentation, operative reports, tumor histology, surgical report, reconstruction technique, follow up, disease-free survival (DFS), and overall survival (OS) data were collected. Descriptive statistics were first used to describe continuous and categorical patient characteristics. Survival outcomes including DFS and OS were described using Kaplan–Meier statistics along with survival curves. Log-rank tests were used to test for difference in survival curves among groups of potential prognostic indicators including: pain on presentation, decreased visual acuity, ulceration, history of radiation, history of prior treatment, history of other skin cancer, tumor location, bone erosion on preoperative imaging, frozen section margins, final margins, tumor histology, and need for additional resection beyond exenteration. Multivariate analysis was performed using Cox proportional hazards model. All statistical analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC, USA) assuming a type I error rate at 0.05 level.
Results
Patient characteristics
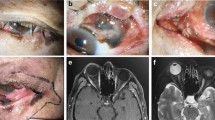
A total of 49 patients (38 male, 11 female) with a mean age of 70.3 years (range 39 to 85) who underwent orbital exenteration for periorbital non-melanoma skin cancer were included in the study (Table 1). The distribution of histological diagnoses in the group included 22 patients with BCC (45%), 17 with SCC (35%), and 10 with SGC (20%, Table 2). 40 patients (82%) had a history of previous cutaneous malignancy occurring at a site other than the periorbita and orbital cavity. The most common locations of the primary lesion were the lower lid (29%), upper lid (29%), medial canthus (18%), and supraorbital/brow skin (18%). Disturbed vision (78%), conjunctival injection (63%), discharge from the lesion (51%), and eye pain (55%) were the most commonly encountered preoperative signs and symptoms. Thirty-five patients (71%) presented with local disease recurrence after previous Mohs micrographic surgery and thirteen patients had received prior radiation treatment; most of the patients were referred from outside institutions so the details of both prior Mohs surgery and radiation therapy were not consistently available. Pre-operative imaging (either CT and/or MRI) was performed for 36 patients (73%), of which obvious orbital involvement was seen in 31 patients.
Surgical characteristics
Twenty-seven patients required additional resection beyond orbital exenteration including 12 parotidectomies, 10 neck dissections, 10 wide local excisions of facial skin, 8 craniofacial approaches, 8 maxillectomies, 6 ethmoidectomies, 5 frontal sinus resections, 4 dural resections with repair, and 2 sentinel lymphadenectomies. For SCC, 7 of the 17 cases required a parotidectomy and neck dissection to address regional lymphadenopathy. Six of the 10 cases of SGC required surgical attention to regional lymph nodes as follows: parotidectomy and neck dissection in 3 cases, sentinel lymph node biopsy in 2 cases (one of which was followed by selective neck dissection due to positive sentinel node), and delayed neck dissection due to recurrence in one case. The extensive nature of disease necessitated the use of a multidisciplinary team approach in 23 cases. This team approach included Oculoplastic Surgery, Head and Neck Surgery, and Neurosurgery when indicated. The remaining 26 surgeries, 15 of which were for basal cell carcinoma, did not require resection beyond the orbit/periorbital tissue and were performed by Oculoplastics alone.
Frozen sections were utilized on an as-needed basis (21 of 49 cases) in sinonasal mucosal sites, dural margins, as well as in extra-orbital facial skin. There were 5 cases in which frozen section margins were positive and in 2 of those cases further resection was performed to achieve a negative final margin status. Interestingly, 6 cases in which the initial frozen section margins were negative ended up with at least one positive final surgical margin.
Reconstruction was performed with split thickness skin grafts in 36 cases, free flap in 9 patients (5 anterolateral thigh, 3 rectus abdominis, 1 radial forearm), and local/regional flaps in 4 flaps (1 cervicofacial advancement flap, 1 temporalis muscle flap, 1 temporoparietal fascia flap, and 1 upper and lower eyelid flap).
Outcome
Median follow-up was 17.5 months (range 0.2–75.2 months). The 2-year OS was 78%, and the 5-year OS was 74%. Taking into account disease recurrence or death, the 2-year DFS was 61% while the 5-year DFS was 51%. The average age at last follow-up was 72.3 years. Of the 23 patients receiving radiation, the majority was preoperative. Ten patients were treated with adjuvant radiation therapy and three were treated with adjuvant chemotherapy.
Five patients (22%) with BCC had positive margins: one at the periorbital skin edge treated successfully with Mohs (patient 11), one at temporalis muscle treated successfully with further resection and radiation (patient 7), one in the infratemporal fossa treated only with radiation who died without clearing the disease (patient 5), and 2 with very advanced tumors with positive margins at the dura who died in the postoperative period (patients 1 and 4, Table 1). Only one patient with BCC developed recurrence which was local at the skin margin and which was treated successfully with Mohs surgery (patient 20, Table 1).
For SCC there were six cases (35%) with positive margins: one at the orbital apex treated with postoperative chemoradiation who died of disease (patient 26), three who did not receive any adjuvant treatment and who died of disease (patients 24, 25 and 29), three with a positive margin at the orbital apex treated with adjuvant chemoradiation who was alive without disease at 14 months (patient 28), and one at the resected skin margin treated with chemoradiation with initial response (patient 32). This last patient later recurred in the parotid and then underwent parotidectomy/lateral temporal bone resection with no evidence of disease at 26 months post-exenteration (Table 1). The recurrence rate for SCC was 30%, with one other case of regional recurrence to the scapula in patient 31, who subsequently did not receive further treatment and died of disease. There were also two other cases of SCC with local recurrence: one underwent clearance of disease through maxillectomy and radiation therapy (patient 36), and another received only radiation and was alive (DFS) at 26 months after exenteration (patient 33, Table 1). The mean time to recurrence overall was 19 months (ranging from 2 to 44 months).
No cases of SGC had positive final margins; however, two (20%) did develop recurrence: one locally who elected no further treatment and died of disease after almost 3 years (patient 48), and another who developed cervical lymph node disease 2 years after exenteration, was treated by neck dissection and radiation, and was alive without disease at 24-month follow-up (patient 47, Table 1).
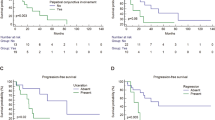
Univariate analysis of OS found the following clinical characteristics to significantly predict worse prognosis: bone erosion (P=0.010), positive permanent surgical margins (P=<0.0001), and additional resection beyond exenteration (P=0.014). The need for additional resection beyond exenteration was also specifically predictive of worse prognosis for the BCC subgroup (P=0.020). Univariate analysis of DFS found that tumor ulceration/drainage at patient presentation was also predictive of a worse prognosis (P=0.045). No other potential prognostic indicator including tumor location, pre-operative visual disturbance, prior radiation therapy, positive frozen section margin, pain at presentation, presence of other skin cancer, or histology was shown to predict a prognosis (Table 3). The survival curves of BCC, SCC, and SGC were not significantly different: 52.6 with SD of ±7.2 months, 39.2±8.5 months, and 28.1±5.6 months, respectively (P-value −0.642, Figure 1).
Multivariate analysis using the Cox’s proportional hazards model showed that only the presence of a positive final surgical margin appeared to confer a significantly worse prognosis (P=0.002, 95% confidence interval of 2.73–102.11; Figure 2).
Discussion
Herein, we examine the clinical characteristics and outcomes of patients with periorbital non-melanoma skin cancer requiring orbital exenteration. The primary objective of exenteration in this clinical context is to completely remove all tumor at the expense of functional and physical disfigurement. Therefore, negative surgical margins are generally considered an important part of the surgical goal when considering exenteration. It is contraindicated in cases of distant tumor metastasis, more than limited intracranial extension, or in cases in which clear margins would be otherwise unobtainable. Surprisingly, we did not find any significant difference between the survival curves of BCC and SCC. This may have been due to limited sample size, as a trend towards significance was seen with best survival outcomes in the BCC group, intermediate in the SCC group, and poorest in the sebaceous cell group. Another explanation for the lower than anticipated survival for the BCC group was the inclusion of highly advanced cases with questionable dural extension such as patient 1 (Table 1) who had a long-standing neglected BCC with initially questionable dural extension that was subsequently confirmed in the operating room. This patient died after exenteration on postoperative day 25 while still in the hospital. The two other basal cell carcinoma deaths also feature positive margins in highly advanced cases in which additional resection was required and in which relatively early postoperative deaths occurred at 3 and 5 months (patients 4 and 5, respectively, Table 1).
Twenty-two percent of cases in this series did have positive permanent surgical margins. This is lower than the rates of positive permanent margins between 28 and 47% reported in other series.6, 17, 19 One possible explanation for this is that the multidisciplinary approach to tumor resection typically used at this tertiary referral cancer center enabled additional surgical procedures to be performed at the same time as the exenteration in order to optimize tumor control. In our series, multivariate analysis showed that the presence of a positive final surgical margin was the only potential factor that was associated with a worse prognosis. Interestingly, positive final surgical margins have not been associated with a worse prognosis in other series.6, 17 It may be hard to compare numbers between different retrospective series because of the heterogeneity of inclusion criteria. This is possibly due to lower overall rates of positive margins in this series as mentioned above, as well as higher rate of micrometastasis of other tumor types such as melanoma, malignant sarcomas, adenoid cystic carcinoma, sinonasal tumors, primary orbital tumors, and lacrimal tumors, which were not included in our study.20 Since frozen section margins were not utilized in over half of the cases in this series a thorough analysis of frozen margin utility in this clinical context could not be performed. However, the fact that there were 6 cases in which all frozen section margins were negative but that at least one final margin was positive does warrant some caution regarding frozen margin reliability in this context.
The rates of overall and disease-free 2-year survival of 78% and 61%, respectively, are consistent with or better than those published in previous series.12, 18, 21, 22 This is likely because advanced cases of periorbital skin cancer are managed at our institution in a multidisciplinary fashion.
Although ulceration, bone erosion, and need for extended resection were not significant prognostic factors on multivariate analysis, they were identified as potentially prognostic on univariate analysis. Their potential as possible prognostic indicators is not surprising as these factors are often regarded as clinical markers of highly aggressive tumors. Those cases tend to have more extensive disease, thus increased likelihood of positive margins (whether recognized or not).9, 20, 23, 24 Contrary to other studies, perineural invasion did not confer a worse prognosis in this series.1, 5, 18 It is important to note, however, that there were not enough cases of confirmed perineural invasion in this series to render statistical analysis of this potential prognostic indicator possible. Our series also failed to show a prognostic difference among subsite origin (lower lid, upper lid, and medial canthus). This could be more relevant for early cancer as opposed to advanced periorbital skin cancers where multiple subsites become involved.
Of the 11 patients with positive final margins, only 4 were without evidence of disease at last follow-up, having been treated with: postoperative radiation only in 2 cases, both additional surgery and radiation in 1 case, and additional surgery only in 1 case whose positive margin was cutaneous. The remaining seven patients with positive margins all died of disease, despite treatment with postoperative radiation in three cases (Table 1). The use of adjuvant radiation was also not prognostic of improved survival on either univariate or multivariate analysis. This further highlights the importance of complete surgical excision with negative margins irrespective of tumor location, prior treatment failure, and adjuvant radiation.
Tumor recurrence was most common within the first 24 months following orbital exenteration and occurred most commonly in SCC. Local and regional recurrence occurred at the same frequency. Local recurrence occurred in 2 cases of SCC, 1 BCC, and 1 SGC. Regional recurrence occurred in 3 cases of SCC and 1 case of SGC. Of note, none of the cases of regional recurrence initially underwent a neck dissection at the time of their exenteration. Adjuvant radiation therapy was used in 6 of the 8 recurrences; however, 2 of these patients died of disease despite this. With the majority of recurrences occurring in the first 2 years following exenteration, we advocate for especially close follow-up during this time period. It is also important to take these findings into consideration when planning the surgical reconstruction of orbital exenteration cases.
There are a variety of reconstructive techniques that may be used after exenteration.25, 26, 27, 28, 29, 30, 31, 32, 33, 34 In this series the majority of reconstruction was done with split thickness skin grafting, as our institute typically uses this technique for exenteration when done alone.35 In cases of extended orbital exenteration involving bone removal, flaps are more commonly used at our institute and there were four cases of local/regional flaps, and nine free flaps done for cases of extended orbital exenteration. We advocate an individualized approach to reconstructive approach. We did not find a statistically significant difference in prognosis based on reconstructive approach. When clinically appropriate, selecting surgical reconstruction techniques, such as split thickness skin grafts, that do not impair the ability to detect recurrence may be advantageous.36
For patients with periorbital BCC and cutaneous SCC who are not surgical candidates due to unresectable disease, multifocal malignancies, multiple medical comorbities, or for whom orbital exenteration is not accepted, targeted systemic therapy is another treatment option which warrants consideration as well as further investigation. Vismodegib (Erivedge), a hedgehog pathway inhibitor approved by for the treatment of metastatic and locally advanced BCC, has been shown to produce either a complete or partial response in 30–60 percent of patients with metastatic or locally advanced BCC,37 and has also been used as neoadjuvant therapy for patients with orbital invasion to make globe-sparing surgical resection possible.38, 39 For patients with SCC with orbital invasion who are unable or unwilling to undergo exenteration, the prognosis is traditionally quite poor,40 but various epidermal growth factor receptor (cetuximab) and tyrosine kinase (gefitinib, erlotinib) inhibitors have been studied in small series and shown efficacy in either reducing or stabilizing cutaneous SCC,41 and may have a neoadjuvant application as well.
A limitation of this study is that while focusing on complete exenteration, we were unable to retrospectively capture and analyze cases of globe-sparing tumor resection in which negative margins were attempted without the need for exenteration. Although cases of globe-sparing and other more conservative orbital surgery were not included in this series, some data suggest that attempts to conserve the globe may be associated with lower rates of clear surgical margins in certain cases.5, 18, 20 In selected cases, globe-sparing surgery can offer the potential for low recurrence rates while maintaining the integrity and function of the globe, even with adjuvant radiation treatment.42, 43 Currently, the decision to proceed with conservation of the globe is individualized to the patient based on tumor location, tumor behavior, tumor subtype, reconstruction goals, and patient preference.18, 20, 42, 43, 44, 45 The roles of and interplay between ‘globe sparing’ surgery and targeted therapy in the treatment of periorbital skin cancer require further study. The inconsistent and in select cases short duration of follow-up is a significant limitation of the study, and therefore the long-term survival data must be interpreted with caution. Another limitation of this study is that many of the initial presenting symptoms of periorbital malignancies were non-specific in nature, thus rendering their retrospective collection and analysis difficult.
Despite the aggressive nature of advanced periocular malignancies, orbital exenteration offers an overall 2-year DFS of ~60% and 2-year OS of ~80%. In our review, worse prognosis was associated with positive final surgical margins. We recommend a multidisciplinary surgical approach to achieve complete resection with negative margins when this surgery is considered. Close follow-up especially in the first 24 months after orbital exenteration is important to detect disease recurrence.

References
Tyers AG . Orbital exenteration for invasive skin tumours. Eye 2006; 20 (10): 1165–1170.
Abraham JC, Jabaley ME, Hoopes JE . Basal cell carcinoma of the medial canthal region. Am J Surg 1973; 126 (4): 492–495.
Ceilley RI, Anderson RL . Microscopically controlled excision of malignant neoplasms on and around eyelids followed by immediate surgical reconstruction. J Dermatol Surg Oncol 1978; 4 (1): 55–62.
Howard GR, Nerad JA, Carter KD, Whitaker DC . Clinical characteristics associated with orbital invasion of cutaneous basal cell and squamous cell tumors of the eyelid. Am J Ophthalmol 1992; 113 (2): 123–133.
Leibovitch I, McNab A, Sullivan T, Davis G, Selva D . Orbital invasion by periocular basal cell carcinoma. Ophthalmology 2005; 112 (4): 717–723.
Rahman I, Maino A, Cook AE, Leatherbarrow B . Mortality following exenteration for malignant tumours of the orbit. Br J Ophthalmol 2005; 89 (11): 1445–1448.
Slutsky JB, Jones EC . Periocular cutaneous malignancies: a review of the literature. Dermatol Surg 2012; 38 (4): 552–569.
Limawararut V, Leibovitch I, Sullivan T, Selva D . Periocular squamous cell carcinoma. Clin Exp Ophthalmol 2007; 35 (2): 174–185.
Kovacevic PT, Visnjic MM, Kovacevic TT, Radojkovic MR, Stojanovic MR . Extended orbital exenteration in the treatment of advanced periocular skin cancer with primary reconstruction with a galeacutaneous flap. Scand J Plast Reconstr Surg Hand Surg 2009; 43 (6): 325–329.
Shields JA, Demirci H, Marr BP, Eagle Jr RC, Shields CL . Sebaceous carcinoma of the ocular region: a review. Surv Ophthalmol 2005; 50 (2): 103–122.
McNab AA, Francis IC, Benger R, Crompton JL . Perineural spread of cutaneous squamous cell carcinoma via the orbit. Clinical features and outcome in 21 cases. Ophthalmology 1997; 104 (9): 1457–1462.
Savage RC . Orbital exenteration and reconstruction for massive basal cell and squamous cell carcinoma of cutaneous origin. Ann Plast Surg 1983; 10 (6): 458–466.
Walling HW, Fosko SW, Geraminejad PA, Whitaker DC, Arpey CJ . Aggressive basal cell carcinoma: presentation, pathogenesis, and management. Cancer Metastasis Rev 2004; 23 (3-4): 389–402.
Roche P, Timon C . Orbital exenteration in periorbital malignancies. Surgeon 2012; 10 (4): 189–193.
Imola MJ, Schramm VL Jr . Orbital preservation in surgical management of sinonasal malignancy. Laryngoscope 2002; 112 (8 Pt 1): 1357–1365.
Ali MJ, Pujari A, Dave TV, Kaliki S, Naik MN . Clinicopathological profile of orbital exenteration: 14 years of experience from a tertiary eye care center in South India. Int Ophthalmol 2016; 36: 253–258.
Mouriaux F, Martinot V, Pellerin P, Patenotre P, Rouland JF, Constantinides G . Survival after malignant tumors of the orbit and periorbit treated by exenteration. Acta Ophthalmol Scand 1999; 77 (3): 326–330.
Hoffman GR, Jefferson ND, Reid CB, Eisenberg RL . Orbital exenteration to manage infiltrative sinonasal, orbital adnexal, and cutaneous malignancies provides acceptable survival outcomes: an institutional review, literature review, and meta-analysis. J Oral Maxillofac Surg 2016; 74 (3): 631–643.
Goldberg RA, Kim JW, Shorr N . Orbital exenteration: results of an individualized approach. Ophthal Plast Reconstr Surg 2003; 19 (3): 229–236.
Ben Simon GJ, Schwarcz RM, Douglas R, Fiaschetti D, McCann JD, Goldberg RA . Orbital exenteration: one size does not fit all. Am J Ophthalmol 2005; 139 (1): 11–17.
Bartley GB, Kasperbauer JL . Use of a flap of extraocular muscle and fat during subtotal exenteration to repair bony orbital defects. Am J Ophthalmol 2002; 134 (5): 787–788.
Mohr C, Esser J . Orbital exenteration: surgical and reconstructive strategies. Graefes Arch Clin Exp Ophthalmol 1997; 235 (5): 288–295.
Malhotra R, Huilgol SC, Huynh NT, Selva D . The Australian Mohs database: periocular squamous cell carcinoma. Ophthalmology 2004; 111 (4): 617–623.
Nemet AY, Martin P, Benger R, Kourt G, Sharma V, Ghabrial R et al. Orbital exenteration: a 15-year study of 38 cases. Ophthal Plast Reconstr Surg 2007; 23 (6): 468–472.
Putterman AM . Orbital exenteration with spontaneous granulation. Arch Ophthalmol 1986; 104 (1): 139–140.
Mauriello Jr JA, Han KH, Wolfe R . Use of autogenous split-thickness dermal graft for reconstruction of the lining of the exenterated orbit. Am J Ophthalmol 1985; 100 (3): 465–467.
Cuesta-Gil M, Concejo C, Acero J, Navarro-Vila C, Ochandiano S . Repair of large orbito-cutaneous defects by combining two classical flaps. J Craniomaxillofac Surg 2004; 32 (1): 21–27.
Menon NG, Girotto JA, Goldberg NH, Silverman RP . Orbital reconstruction after exenteration: use of a transorbital temporal muscle flap. Ann Plast Surg 2003; 50 (1): 38–42.
Reese AB, Jones IS . Exenteration of the orbit and repair by transplantation of the temporalis muscle. Am J Ophthalmol 1961; 51: 217–227.
Lee HB, Hong JP, Kim KT, Chung YK, Tark KC, Bong JP . Orbital floor and infraorbital rim reconstruction after total maxillectomy using a vascularized calvarial bone flap. Plast Reconstr Surg 1999; 104 (3): 646–653.
Uusitalo M, Ibarra M, Fulton L, Kaplan M, Hoffman W, Lee C et al. Reconstruction with rectus abdominis myocutaneous free flap after orbital exenteration in children. Arch Ophthalmol 2001; 119 (11): 1705–1709.
Wax MK, Burkey BB, Bascom D, Rosenthal EL . The role of free tissue transfer in the reconstruction of massive neglected skin cancers of the head and neck. Arch Facial Plast Surg 2003; 5 (6): 479–482.
Lim N, Mulhern MG, Joshi N, Waterhouse N, Peterson D, Coghlan B . The use of autologous autoclaved bone in orbital reconstruction after exenteration for invasive cutaneous carcinoma. Orbit 2002; 21 (3): 181–187.
Nerad JA, Carter KD, LaVelle WE, Fyler A, Branemark PI . The osseointegration technique for the rehabilitation of the exenterated orbit. Arch Ophthalmol 1991; 109 (7): 1032–1038.
Tse DT (ed). Color Atlas of Oculoplastic Surgery, 2nd ed. Lipincott, Williams, and Wilkins, Philadephia, PA, USA, 2011.
Nassab RS, Thomas SS, Murray D . Orbital exenteration for advanced periorbital skin cancers: 20 years experience. J Plast Reconstr Aesthet Surg 2007; 60 (10): 1103–1109.
Sekulic A, Migden MR, Oro AE, Dirix L, Lewis KD, Hainsworth JD et al. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. N Engl J Med 2012; 366 (23): 2171–2179.
Ally MS, Aasi S, Wysong A, Teng C, Anderson E, Bailey-Healy I et al. An investigator-initiated open-label clinical trial of vismodegib as a neoadjuvant to surgery for high-risk basal cell carcinoma. J Am Acad Dermatol 2014; 71 (5): 904–11 e1.
Mortier L SP, Leccia MT, Mahmoudi A, Mirakovska L, Meddour D, Duhamel A et al. A phase II study to assess vismodegib in the neoadjuvant treatment of locally advanced basal cell carcinoma (laBCC). The Vismodegib Neoadjuvant (VISMONEO) Study. J Clin Oncol 2014; 32 (5s)suppl; abstr TPS9104.
Soysal HG, Markoc F . Invasive squamous cell carcinoma of the eyelids and periorbital region. Br J Ophthalmol 2007; 91 (3): 325–329.
Yin VT, Pfeiffer ML, Esmaeli B . Targeted therapy for orbital and periocular basal cell carcinoma and squamous cell carcinoma. Ophthal Plast Reconstr Surg 2013; 29 (2): 87–92.
Catalano PJ, Laidlaw D, Sen C . Globe sparing orbital exenteration. Otolaryngol Head Neck Surg 2001; 125 (4): 379–384.
Madge SN, Khine AA, Thaller VT, Davis G, Malhotra R, McNab A et al. Globe-sparing surgery for medial canthal Basal cell carcinoma with anterior orbital invasion. Ophthalmology 2010; 117 (11): 2222–2228.
Taylor A, Roberts F, Kemp EG . Orbital exenteration–-a retrospective study over an 11 year period analyzing all cases from a single unit. Orbit 2006; 25 (3): 185–193.
Wong JC, Thampy R, Cook A . Life expectancy following orbital exenteration. Br J Ophthalmol 2015; 99 (1): 1–4.
Acknowledgements
This work was supported by NIH Center Core Grant P30EY014801, Research to Prevent Blindness Unrestricted Grant.
Author contributions
Presentation: RCG, CTO, STW, ZBS. Orbital Exenteration for Advanced Periorbital Non-Melanoma Skin Cancer: Prognostic Factors and Survival. American Academy of Otolaryngology Annual Meeting, Vancouver, BC, Canada, September, 2013.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gerring, R., Ott, C., Curry, J. et al. Orbital exenteration for advanced periorbital non-melanoma skin cancer: prognostic factors and survival. Eye 31, 379–388 (2017). https://doi.org/10.1038/eye.2016.218
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2016.218
This article is cited by
-
A registration trend in eyelid skin cancers and associated risk factors in Iran, 2005–2016
BMC Cancer (2023)
-
Primary cemiplimab treatment for orbital squamous cell carcinoma is effective and may alleviate the need for orbital exenteration
Eye (2023)
-
A Systematic Review Article on Orbital Exenteration: Indication, Complications and Reconstruction Methods
Indian Journal of Otolaryngology and Head & Neck Surgery (2022)
-
Periorbital, conjunctival and primary intraorbital carcinomas: Survival and risk factors after orbital exenteration
Eye (2021)
-
Efficacy and safety of an artificial dermal graft for the reconstruction of exenterated sockets: a preliminary report
Graefe's Archive for Clinical and Experimental Ophthalmology (2021)