Abstract
Purpose
The aim of this study is to investigate the difference of the clinical course in recurrent intermittent exotropia after second surgery compared with both recurrent intermittent exotropia after its first of two surgeries and intermittent exotropia after only a single surgery.
Methods
We retrospectively reviewed the medical records of patients diagnosed with intermittent exotropia who underwent lateral rectus recession and medial rectus resection (R&R) between January 1992 and January 2011 at Yeungnam University Hospital. Repeated measure ANOVA (rmANOVA) was used to compare the clinical course of recurrent intermittent exotropia before and after a second surgery with that of intermittent exotropia with a single surgery.
Results
A total of 352 intermittent exotropia patients who underwent one R&R procedure and 77 recurrent intermittent exotropia patients who underwent a second R&R in the contralateral eye were included in this study. Although exodrift of recurrent intermittent exotropia was observed at 24 months of follow-up even after a second surgery, it was significantly lower than both intermittent exotropia with a single surgery and after its first of two surgeries (P<0.001, rmANOVA).
Conclusion
The clinical course of recurrent intermittent exotropia after a second surgery was improved compared with both recurrent intermittent exotropia after its first of two surgeries and intermittent exotropia after a single surgery.
Similar content being viewed by others
Introduction
Intermittent exotropia is the most common type of strabismus among Asians, especially Koreans. Although surgical treatment results in a better outcome than nonsurgical treatment, such as orthoptics or occlusion therapy, many studies have reported postoperative exodrift and recurrence of intermittent exotropia over time after surgical treatment.1, 2, 3, 4, 5 Regarding a second surgery for recurrent intermittent exotropia, we are often asked by patients or their parents whether a second surgery will improve the outcome following the first surgery. Some studies using survival analysis have found a lower recurrence rate after a second surgery.6, 7 However, few studies have conducted longitudinal comparisons of the clinical course of recurrent intermittent exotropia after a second surgery and intermittent exotropia that showed good ocular alignment after a single surgery. Moreover, we were also interested in the difference of clinical course in recurrent intermittent exotropia before and after a second surgery. Therefore, we investigated the clinical course of recurrent intermittent exotropia after a second surgery, and compared it with not only the clinical course after a single surgery but also the clinical course after the first surgery when a second was performed.
Subjects and methods
Patient selection criteria
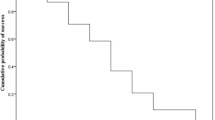
We reviewed retrospectively the medical records of intermittent exotropia patients who underwent lateral rectus recession and medial rectus resection (R&R) between January 1992 and January 2011 at Yeungnam University Hospital. For inclusion in this study, the required follow-up period after surgery was 24 months. Intermittent exotropia patients included in this study were first divided into two groups: primary surgery group: those who had good ocular alignment after a single surgery; resurgery group: those who had recurred intermittent exotropia after first surgery and underwent a second surgery. To compare the difference between clinical course of recurrent intermittent exotropia after first surgery and after second surgery, resurgery group was divided into two subgroups: resurgery 1 group: the clinical course of recurrent intermittent exotropia during postoperative follow-up after the first surgery until before the second surgery; resurgery 2 group: the clinical course of recurrent intermittent exotropia during postoperative follow-up after the second surgery. The division of patients into three groups is summarized graphically in Figure 1a. Patients with any other types of strabismus such as oblique muscle dysfunction, dissociated vertical deviation, A–V pattern, and nystagmus were excluded from this study. Patients with previous intraocular surgery, any neurological impairment such as cerebral palsy, or unilateral amblyopia were also excluded.
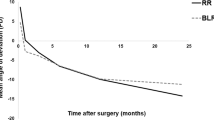
The summarized design and result of study. (a) Intermittent exotropia patients were divided into three groups: primary surgery group, resurgery 1 group, and resurgery 2 group. The difference in the postoperative angle of deviation within and between the three groups was analyzed using repeated measure ANOVA. (b) Postoperative angle of deviation in the three groups: primary surgery group, resurgery 1 group, and resurgery 2 group. Repeated measure ANOVA found significant difference among the groups (P<0.001).
Preoperative evaluation
At the initial visit, all patients underwent a full ophthalmologic examination, including visual acuity testing, ocular alignment status, slit-lamp biomicroscopy, refraction, fundus examination, and stereoacuity test. The angle of deviation was measured by alternate prism cover testing at 6 m and 33 cm fixation in cooperative children both pre- and postoperatively. Best-corrected visual acuity was measured where possible. Amblyopia was defined as an interocular difference in visual acuity of two lines or more. If amblyopia was found, the occlusion therapy was performed to treat amblyopia as soon as possible before surgery. Stereoacuity was measured with Lang I test and Titmus stereotest when the patient was able to cooperate and complete the test.
Surgical plan
Every surgery was performed by a single surgeon (MMK) under general anesthesia. The unilateral R&R procedure was undertaken using surgical dosage of our clinic (Table 1) based on the patients’ angle of deviation measured the day before the surgery. The contralateral R&R procedure was performed as the second surgery in recurrent intermittent exotropia patients who had previously undergone unilateral R&R procedure.
Postoperative evaluation
The patients were followed-up at 1, 3, 6, and 12 months after the surgery, and every 6 months thereafter. The postoperative angle of deviation was measured at each visit. Patients who missed any regular follow-up over the 24 postoperative months were excluded from this study.
Statistical analysis
Continuous data are presented as a mean with SD, and categorical data are presented as counts. Comparisons for continuous variables were performed using independent t-test. The χ2 method was used to test the significance of differences between proportions and categorical variables. We used repeated measures ANOVA (rmANOVA) to analyze the difference in clinical course between the primary surgery group, resurgery 1 group, and resurgery 2 group. Univariate and multivariate logistic regression tests were conducted to evaluate factors associated with the second surgery. The SPSS statistical software, version 20.0 (SPSS, Inc., an IBM Company, Chicago, IL, USA) was used for statistical analyses. A P-value of <0.05 was regarded as statistically significant.
Results
The clinical records of 1618 intermittent exotropia patients who underwent R&R procedure were retrospectively reviewed. Among them, 182 patients underwent contralateral R&R procedure as a second surgery. No patient required an additional surgery for overcorrection after first surgery and one patient underwent a third surgery for overcorrection after second surgery. Of the total 1618 patients, 429 patients met the inclusion criteria for this study. In all, 352 patients were included in the primary surgery group and 77 patients in the resurgery group. The demographic and clinical characteristics of these patients at the first surgery are in Table 2. In the resurgery group, the mean interval from the first surgery to second surgery was 46.32±27.87 (24–195) months. The basic type, which was defined when the difference between distant and near angle was within 10 PD, was the most common in both groups. The pre- and postoperative angle of deviation for each group are shown in Table 3. The postoperative angle of deviation significantly increased in each group at all postoperative follow-ups over 24 months. An rmANOVA analysis revealed statistically significant group-by-time effects for the postoperative angle of deviation (Figure 1b, rmANOVA, P<0.001). The postoperative angle of deviation of resurgery 2 group was lower than that of both the primary surgery group and resurgery 1 group over postoperative 24 months.
The association between the resurgery group and clinical characteristics was assessed by univariate and multivariate logistic regression. Multicollinearity was evaluated by the tolerance and variance-inflation-factor, and the assumption of multicollinearity was not violated with these variables. Age at first surgery, gender, spherical equivalent refractive error, the result of Lang I stereotest, and pre- and postoperative angle of deviation were first tested using univariate analysis; variables with P<0.2 in univariate analysis are shown in Table 4. The preoperative angle of deviation showed little association with the second surgery (P=0.739). Filtered variables with P<0.2 in univariate analysis were further evaluated to identify association using multivariate analysis. In entry mode of multivariate analysis, age at first surgery (odds ratio: 0.752, P<0.001) showed the strongest association with the second surgery.
Discussion
When considering a second surgery for recurrent intermittent exotropia, we are usually asked by patient or their parents about the expected prognosis after a second surgery. The two most frequently asked questions are as follows: ‘Is there any possibility of recurrence even after a second surgery?’ and ‘Will the clinical course after the second surgery be better than after the first surgery?’ Several studies have addressed the first question. Hahm et al6 reported that exotropia did recur even after a repeat surgery, although the recurrence rate was lower than that after a primary surgery. The study of Kim and Kim7 using survival analysis showed decreasing cumulative probabilities of the surgical success rate after a second surgery for recurrent intermittent exotropia. Addressing the second question, we were not able to find out any previous study of longitudinal comparison of clinical course of recurrent intermittent exotropia after second operation. In addition, we aimed to clarify whether there is any difference in the clinical course of recurrent intermittent exotropia after a second surgery as compared with not only intermittent exotropia after a single surgery but also recurrent intermittent exotropia after the first of two surgeries. These questions led us to investigate the clinical course of recurrent intermittent exotropia after a second surgery. We analyzed the data of intermittent exotropia patients who underwent an R&R procedure using the rmANOVA method.
This study design was used for the following two main reasons. First, the R&R procedure is one of the most common surgical methods used for correction of intermittent exotropia,8, 9, 10 and we are of the opinion that the surgical data gained by a single surgical procedure performed by a single surgeon will be more valid than that gained by different surgeons performing different procedures. Second, the rmANOVA method is able to analyze the difference over time not only within groups but also between groups. Moreover, since our clinic opened, postoperative examinations have been conducted using the same follow-up protocol. Therefore, we could use the rmANOVA test for our study. To enhance the accuracy of the analysis, any patient who missed any regular follow-up in the postoperative 24 months was excluded from this study.
The results showed significant increasing postoperative angle of deviation in all three groups over time. This result is consistent with previous reports of exodrift of intermittent exotropia after surgery.1, 3, 8, 9, 11 Exodrift was also observed after a second surgery in recurrent intermittent exotropia patients. However, the postoperative angle of deviation of the resurgery 2 group was significantly lower than that of both the primary surgery group and resurgery 1 group over 24 months of follow-up. This demonstrates that the clinical course of recurrent intermittent exotropia after a second surgery is better than both intermittent exotropia after a single surgery and recurrent intermittent exotropia after the first of two surgeries.
Why was the incidence of exodrift of the resurgery 2 group lower than that of both the primary surgery group and resurgery 1? In a study of large angle amblyopic exotropia, large resection of the medial rectus using a stay suture was stressed to mechanically prevent an exotropic recurrence.12 The mechanical force caused by resected medial rectus muscles in both eyes after the first and second surgery is postulated to be the main cause of the lower exodrift of recurrent intermittent exotropia after a second surgery. In addition, previous studies reported that immediate postoperative deviation showed significant association with favorable surgical result.3, 8, 11 In the present study, recurrent intermittent exotropia after second surgery showed lower immediate postoperative deviation than intermittent exotropia with a single surgery (P<0.001). The difference in immediate postoperative deviation is also considered the reason of the lower exodrift of recurrent intermittent exotropia after a second surgery.
In the analysis of associated factors related to the second surgery using multivariate logistic regression test, age at surgery showed the strongest association with second surgery. The risk of resurgery decreased with increased age at the first surgery. This result agrees with our previous study by Lim et al.8
There is controversy regarding the association between stereopsis and surgical outcome of intermittent exotropia. Beneish and Flanders13 reported that poor preoperation stereopsis dose not necessarily preclude, and may enhance, long-term alignment stability postoperatively. However, Yildirim et al14 reported that better distance stereoacuity and central fusion are frequently associated with better surgical success in intermittent exotropia. In the present study, there was no difference in stereoacuity measured using Lang I stereotest between primary group and resurgery group. The result of Lang I stereotest did not shown any association with second surgery. We could not analyze an association between Titmus test and second surgery for missing observations. The limitation of our study was that a small number of recurrent intermittent exotropia patients whose interval from first to second surgery was <24 months were excluded from the study. However, those data would have little influence on the results.
In conclusion, our results demonstrate that the clinical course of recurrent intermittent exotropia after a second surgery is better at postoperative 24-month follow-up compared with both intermittent exotropia with a single surgery and after its first of two surgeries. These results shed light on the prognosis of recurrent intermittent exotropia after a second surgery.

References
Leow P-L, Ko STC, Wu PKW, Chan CWN . Exotropic drift and ocular alignment after surgical correction for intermittent exotropia. J Pediatr Ophthalmol Strabismus 2010; 47 (1): 12–16.
Figueira EC, Hing S . Intermittent exotropia: comparison of treatments. Clin Exp Ophthalmol 2006; 34 (3): 245–251.
Pineles SL, Ela-Dalman N, Zvansky AG, Yu F, Rosenbaum AL . Long-term results of the surgical management of intermittent exotropia. J AAPOS 2010; 14 (4): 298–304.
Maruo T, Kubota N, Sakaue T, Usui C . Intermittent exotropia surgery in children: long term outcome regarding changes in binocular alignment. A study of 666 cases. Binocul Vis Strabismus Q 2001; 16 (4): 265–270.
Ekdawi NS, Nusz KJ, Diehl NN, Mohney BG . Postoperative outcomes in children with intermittent exotropia from a population-based cohort. J AAPOS 2009; 13 (1): 4–7.
Hahm IR, Yoon SW, Baek S-H, Kong SM . The clinical course of recurrent exotropia after reoperation for exodeviation. Korean J Ophthalmol 2005; 19 (2): 140–144.
Kim WJ, Kim MM . The clinical course of recurrent intermittent exotropia after previous unilateral recess-resection surgery. J Korean Opthalmol Soc 2009; 50 (9): 1386–1391.
Lim SH, Hong JS, Kim MM . Prognostic factors for recurrence with unilateral recess-resect procedure in patients with intermittent exotropia. Eye (Lond) 2011; 25 (4): 449–454.
Hatsukawa Y, Nishina S, Sugasawa J, Kimura A, Yagasaki T, Fujikado T et al. Surgical results of unilateral recession-resection for intermittent exotropia in children: multicenter study in Japan. Nippon Ganka Gakkai Zasshi 2011; 115 (5): 440–446.
Choi J, Chang JW, Kim SJ, Yu YS . The long-term survival analysis of bilateral lateral rectus recession versus unilateral recession-resection for intermittent exotropia. Am J Ophthalmol 2012; 153 (2): 343–351.e1.
Lim SH, Hwang BS, Kim MM . Prognostic factors for recurrence after bilateral rectus recession procedure in patients with intermittent exotropia. Eye (Lond) 2012; 26 (6): 846–852.
Rayner JW, Jampolsky A . Management of adult patients with large angle amblyopic exotropia. Ann Ophthalmol 1973; 5 (1): 95–99.
Beneish R, Flanders M . The role of stereopsis and early postoperative alignment in long-term surgical results of intermittent exotropia. Can J Ophthalmol 1994; 29 (3): 119–124.
Yildirim C, Mutlu FM, Chen Y, Altinsoy HI . Assessment of central and peripheral fusion and near and distance stereoacuity in intermittent exotropic patients before and after strabismus surgery. Am J Ophthalmol 1999; 128 (2): 222–230.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This study was presented as a free paper at the annual meeting of the Korean Ophthalmological Society in Seoul, 1–3 November 2013.
Rights and permissions
About this article
Cite this article
Kim, W., Kim, M. The clinical course of recurrent intermittent exotropia following one or two surgeries over 24 months postoperatively. Eye 28, 819–824 (2014). https://doi.org/10.1038/eye.2014.93
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.93
This article is cited by
-
The subjective controllability of exotropia and its effect on surgical outcomes in patients with intermittent exotropia
BMC Ophthalmology (2023)
-
Effects of orthoptic therapy in children with intermittent exotropia after surgery: study protocol for a randomized controlled trial
Trials (2022)
-
Surgical success of lateral rectus resection for residual and recurrent esotropia
International Ophthalmology (2021)
-
Risk factors associated with poor outcome after medial rectus resection for recurrent intermittent exotropia
Graefe's Archive for Clinical and Experimental Ophthalmology (2020)
-
The fast exodrift after the first surgical treatment of exotropia and its correlation with surgical outcome of second surgery
BMC Ophthalmology (2018)